Copyright
©2010 Baishideng.
World J Gastroenterol. Aug 7, 2010; 16(29): 3716-3722
Published online Aug 7, 2010. doi: 10.3748/wjg.v16.i29.3716
Published online Aug 7, 2010. doi: 10.3748/wjg.v16.i29.3716
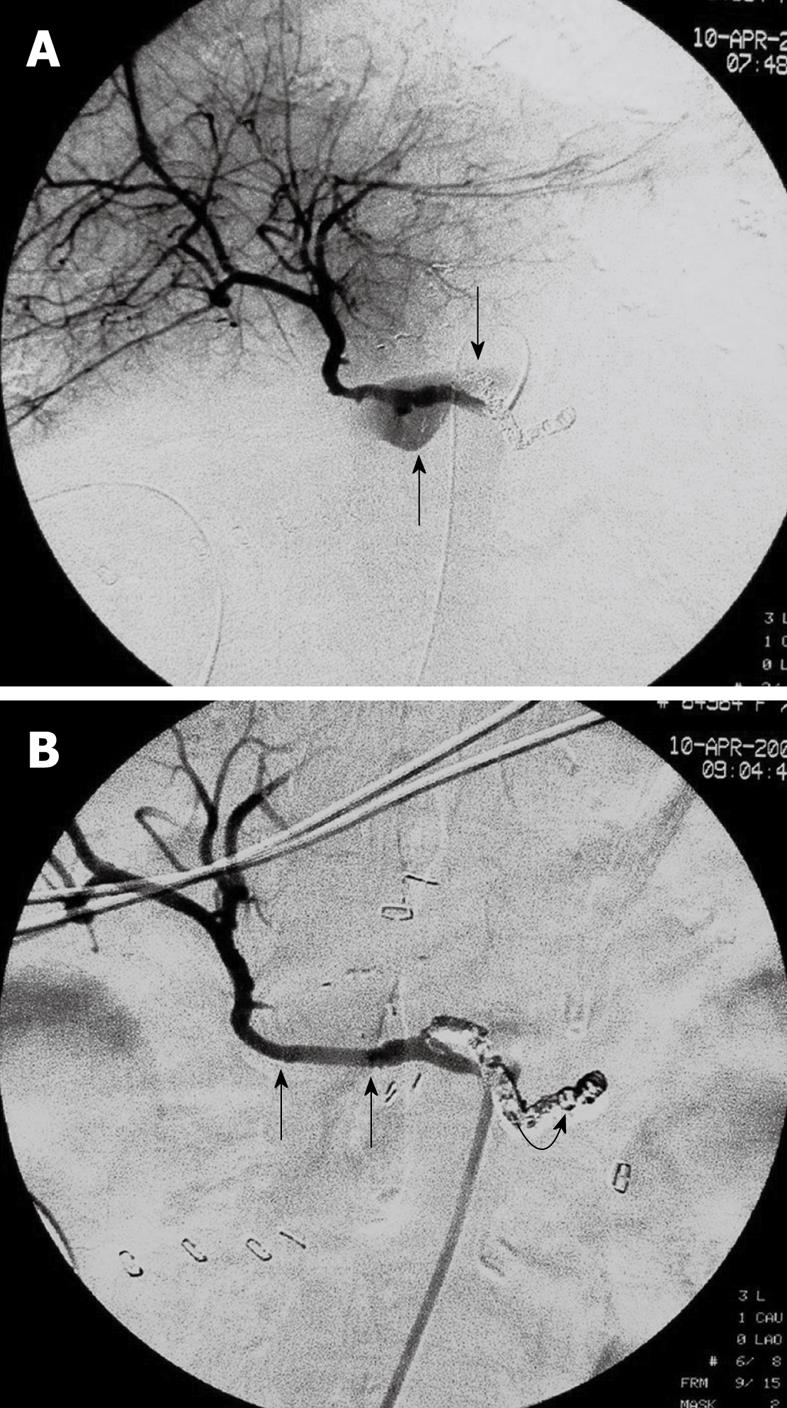
Figure 1 A 75-year-old female with pancreatic head malignancy underwent a pylorus-preserving pancreaticoduodenectomy (Case 1).
A: Selective angiography of the common hepatic artery shows a large ruptured hepatic artery pseudoaneurysm with extravasation of contrast medium (arrows); B: Angiography after two stent-grafts placement demonstrates exclusion of the aneurysm and preserved hepatic artery blood flow through the stent-grafts (arrows). Note the splenic artery was embolized 4 d ago due to bleeding from the splenic artery (curved arrow).
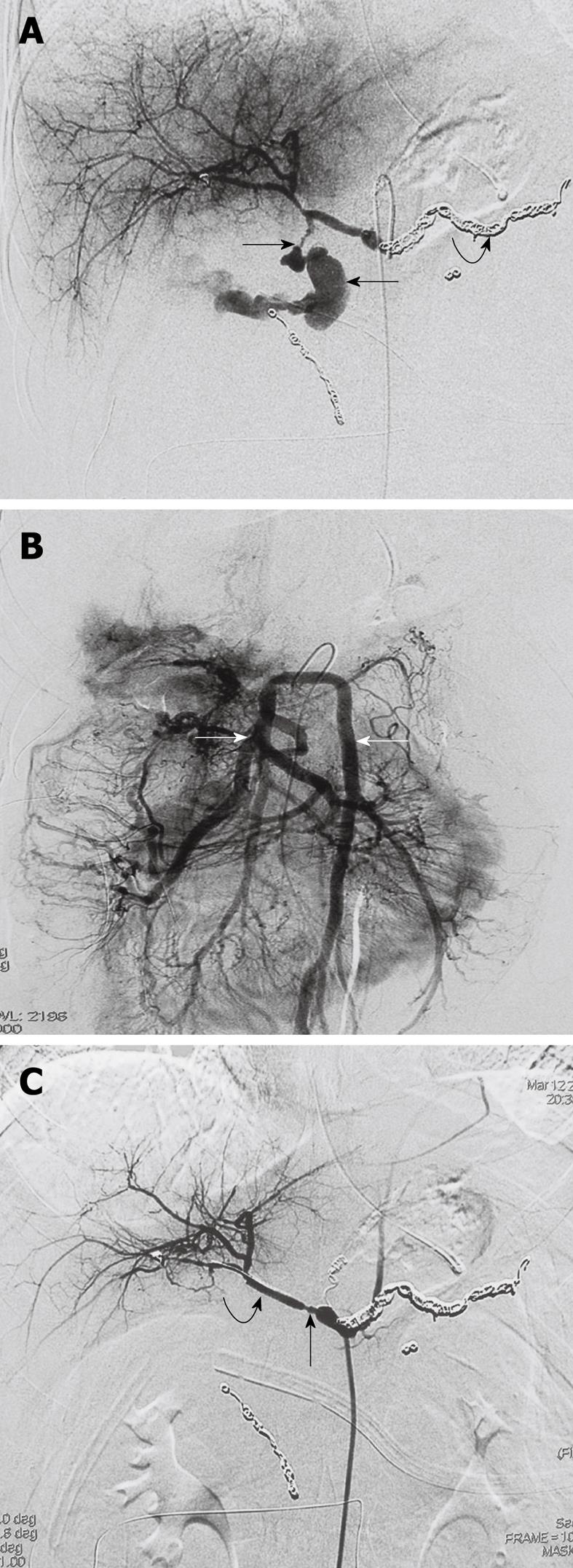
Figure 2 A 23-year-old female with pancreatic trauma underwent a pylorus-preserving pancreaticoduodenectomy (Case 2).
A: Emergent selective angiography of the celiac trunk demonstrates massive extravasation of contrast medium into the abdominal cavity from the ruptured hepatic artery pseudoaneurysm (arrows). Note the splenic artery was embolized 6 d ago due to bleeding from the splenic artery (curved arrow); B: Digital substraction superior mesenteric artery angiogram with delayed phase demonstrates no visualization of the portal vein, and remarkable pooling of contrast medium at the branches of the SMV (arrows); C: Angiography after two pieces of stent-grafts placement shows exclusion of the bleeding hepatic pseudoaneurysm and good hepatic arterial blood flow through the stent-grafts (curved arrow). Note the spasm of the proximal hepatic artery (arrow).
- Citation: Wang MQ, Liu FY, Duan F, Wang ZJ, Song P, Fan QS. Stent-grafts placement for treatment of massive hemorrhage from ruptured hepatic artery after pancreaticoduodenectomy. World J Gastroenterol 2010; 16(29): 3716-3722
- URL: https://www.wjgnet.com/1007-9327/full/v16/i29/3716.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i29.3716