Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Feb 14, 2009; 15(6): 684-693
Published online Feb 14, 2009. doi: 10.3748/wjg.15.684
Published online Feb 14, 2009. doi: 10.3748/wjg.15.684
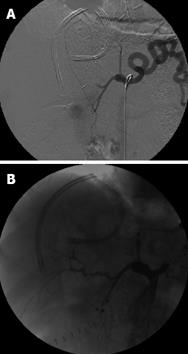
Figure 1 Status post right lobe LRLT in 18-year-old male.
A: Celiac arteriogram showed acute HAT. Local thrombolysis with TPA was performed by placing a microcatheter in the hepatic artery stump; B: Celiac arteriogram after TPA infusion showed patent hepatic artery. In this patient, splenic artery embolization was performed by coils and PVA in order to increase the flow in hepatic artery. Although a good and early flow restoration was achieved, the patient underwent re-transplantation 2 d later for graft failure.
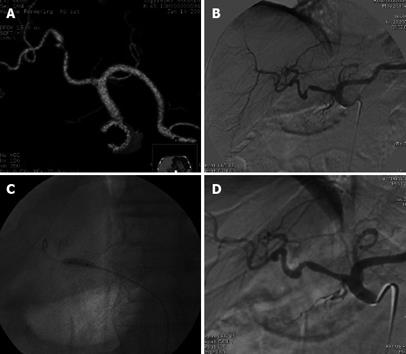
Figure 2 Status post deceased donor LT.
Doppler US performed 5 mo after the transplant showed low intrahepatic resistive index 0.50 and prolonged systolic acceleration time 0.113 s, suspected for HAS. A: MDCT volume rendering 3D reconstruction showed a severe stenosis in the hepatic artery anastomosis; B: Digital subtraction angiography (DSA) celiac arteriogram confirmed the stenosis, trans-stenotic pressure gradient measured by a microcatheter was 50 mmHg; C: DSA percutaneous transluminal angioplasty performed by 4 mm diameter balloon catheter; D: DSA final arteriogram showed good patency of the arterial anastomosis with trans-stenotic pressure gradient reduced to 4 mmHg. Doppler US performed 4 mo later showed regular resistive index 0.70 and systolic acceleration time 0.100 s. Patient currently in good general condition and without biliary tree impairment after 6 mo of follow-up.
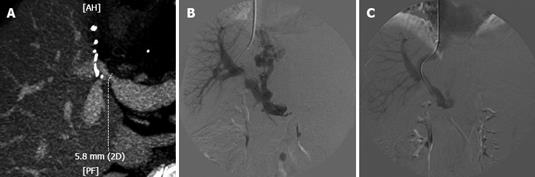
Figure 3 Status post right lobe LRLT in 60-year-old female.
A: MDCT, MIP reconstruction showed a stenosis in portal vein anastomosis. The stenosis is very near the bifurcation of anterior and posterior branches; B: DSA, portogram performed from transjugular approach confirmed the PVS, 15 mmHg trans-stenotic pressure gradient was measured; note large patent coronary vein with filling gastro-oesophageal varices; C: DSA, final portogram performed after the deployement of a 10-mm diameter WallStent; note good filling of intrahepatic branches and no more evidence of the coronary vein, trans-stenotic pressure gradient reduced to 6 mmHg. Patient currently in good general condition with 1 year of follow-up.
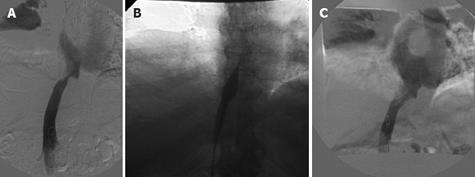
Figure 4 Status post deceased donor LT.
Patient with refractory ascites in association with renal insufficiency and lower extremities edema 4 years after the transplant. A: DSA, cavogram showed a stenosis of IVC upper anastomosis, 12 mmHg trans-stenotic pressure gradient was measured. In the same session hepatic veins catheterization was performed showing no concomitant stenoses in hepatic vein anastomosis; B: DSA percutaneous transluminal angioplasty performed by 16-mm diameter balloon catheter; C: DSA final cavogram showed good patency of the caval anastomosis with trans-stenotic pressure gradient reduced to 2 mmHg. From 2001 to 2007, four other trans-luminal caval angioplasties were performed in the same patient. The patient is currently in good general condition after 15 mo and has avoided re-transplantation.
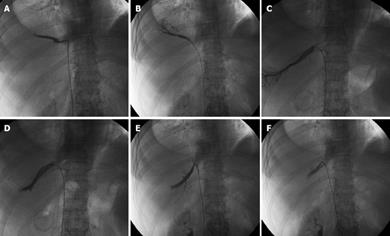
Figure 5 Status post deceased donor right lobe split LT in 65-year-old female.
Three separates HV anastomoses were performed. One month after LT, patient developed refractory ascites and right pleural effusion with worsening of liver function tests. Doppler US was suspicious of HVs. A cavogram performed from the femoral approach showed widely patent IVC anastomosis. Selective catheterization of the three HVs (A, C and E) showed stenosis in the three anastomoses with trans-stenotic pressure gradient of 15, 20 and 16 mmHg, respectively. Balloon angioplasties were performed with balloon catheters ranging from 7 to 10 mm in diameter. Final venogram showed patent anastomoses (B, D and F). Trans-anastomotic pressure gradient reduced to 4, 2.5 and 8 mmHg. Eight months of follow-up without recurrence of refractory ascites and/or hydrothorax.
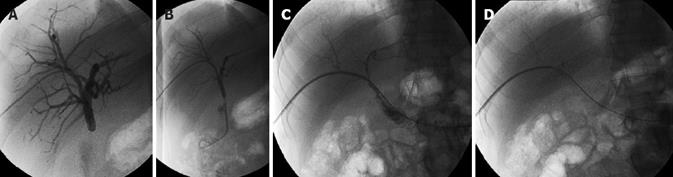
Figure 6 Status post deceased donor LT in 40-year-old man.
Hepatico-jejunostomy was performed. A: PTC shows moderate biliary duct dilatation and subocclusive biliary anastomosis stricture; B: The stricture was crossed and trans-anastomotic. 6F Ring biliary catheter was placed; C: cholangiogram performed after four sessions of percutaneous bilioplasty shows no bile duct dilatation and patent anastomosis; D: Evidence of complete contrast transition from the bile ducts into the bowel loop within 2 min after the cholangiography. Three years of follow-up without clinical evidence of stricture recurrency.
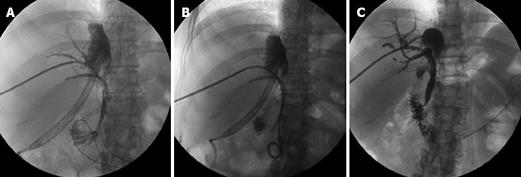
Figure 7 Status post LRLT (right lobe) in 56-year-old woman.
Two separate biliary anastomoses were performed. Approximately 300 mL of bile was drained every day from the existing perihepatic drainage catheter (JP) placed during the transplantation. ERCP was performed, revealing a BL from the anastomotic region. An endoscopic stent was deployed in the posterior duct anastomosis but endoscopy failed to place a stent in the anterior duct anastomosis. A: PTC of the anterior duct showed no bile ducts dilatation and a BL arising from the anastomosis; B: 12F external internal catheter without side holes was placed in the leak region. The bile output from the JP progressively reduced and stopped a few days later. The JP and the endoscopic stent were removed 1 mo later; C: Final cholangiogram performed 4 mo later showed no BL and patent biliary anastomosis. The catheter was removed. The patient is still in good condition after 12 mo of follow-up.
- Citation: Miraglia R, Maruzzelli L, Caruso S, Milazzo M, Marrone G, Mamone G, Carollo V, Gruttadauria S, Luca A, Gridelli B. Interventional radiology procedures in adult patients who underwent liver transplantation. World J Gastroenterol 2009; 15(6): 684-693
- URL: https://www.wjgnet.com/1007-9327/full/v15/i6/684.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.684