Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Dec 21, 2009; 15(47): 5889-5897
Published online Dec 21, 2009. doi: 10.3748/wjg.15.5889
Published online Dec 21, 2009. doi: 10.3748/wjg.15.5889
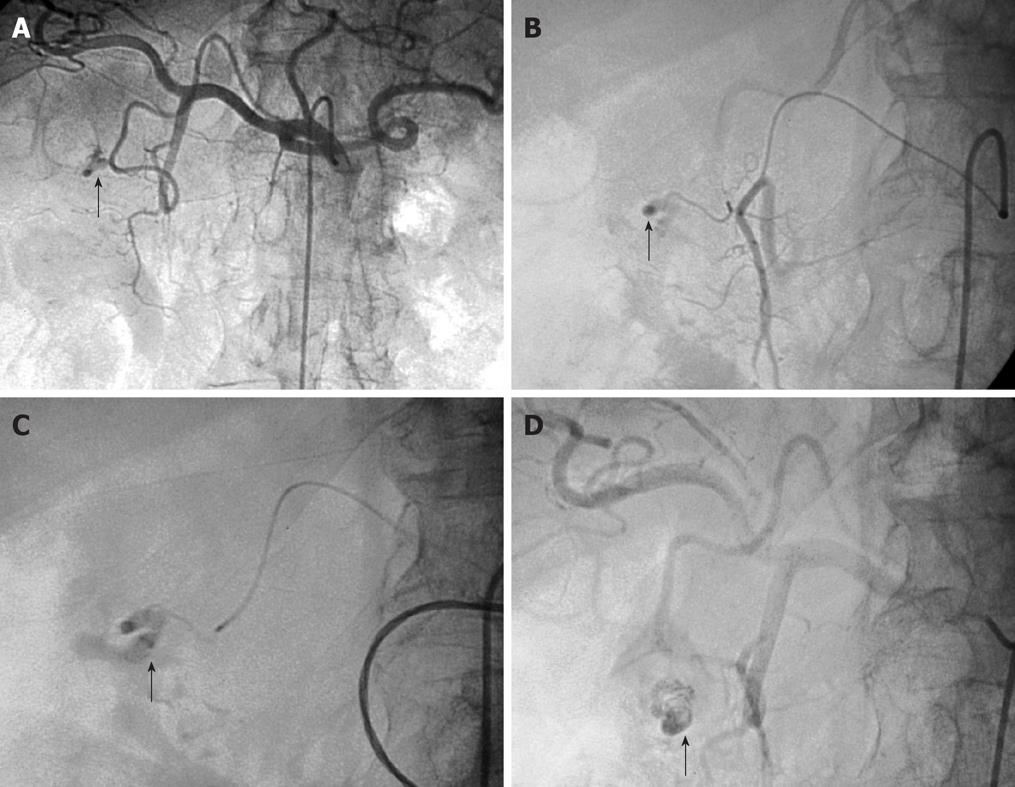
Figure 1 Arteriogram images of bleeding from a bulbar duodenal ulcer in a 76-year-old man.
A, B: Arteriogram showing contrast medium extravasated from a slender branch of the gastroduodenal artery (GDA) into the duodenum (arrows); C, D: After microcatheterization, selective glue embolization (radiopaque because of associated lipiodol (arrows) preserving the GDA ensured control of the bleeding, with no early or late recurrences.
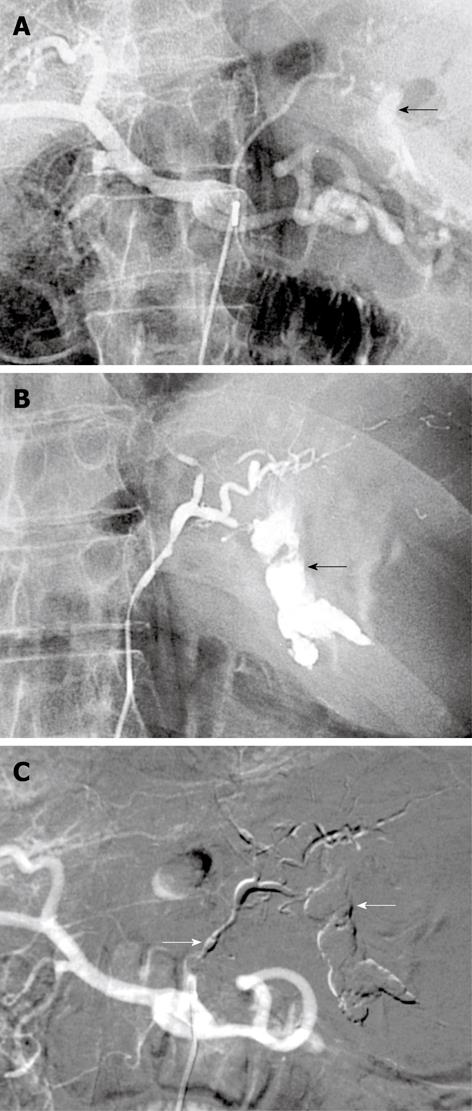
Figure 2 Bleeding Dieulafoy lesion in an 87-year-old man.
A, B: Selective angiography shows contrast medium extravasation from the left gastric artery at the celiac trunk, indicating active bleeding (arrows); C: After arterial microcatheterization, bleeding was controlled after embolization of the left gastric artery using a Glubran/Lipidol mixture (1:3) (arrows).
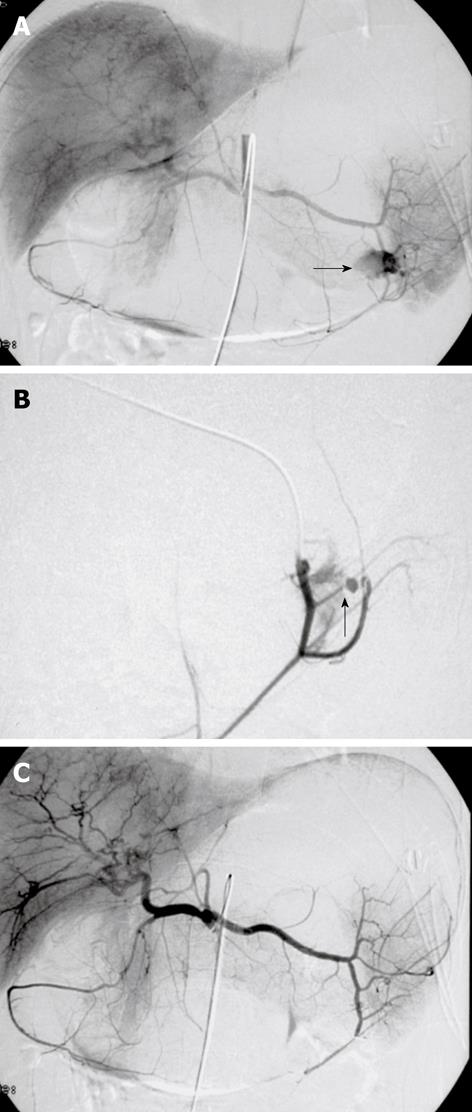
Figure 3 Digital subtraction images from a 37-year-old man with massive hematemesis.
A, B: Selective angiography shows a bleeding ulcer in the fundus of the stomach. Extravasation of contrast medium from a branch of the left gastroepiploic artery is seen (arrows); C: The control angiogram after glue embolization throughout the splenic artery shows complete and selective occlusion of the bleeding branch, with no active bleeding. The patient was discharged from the hospital 4 d later.
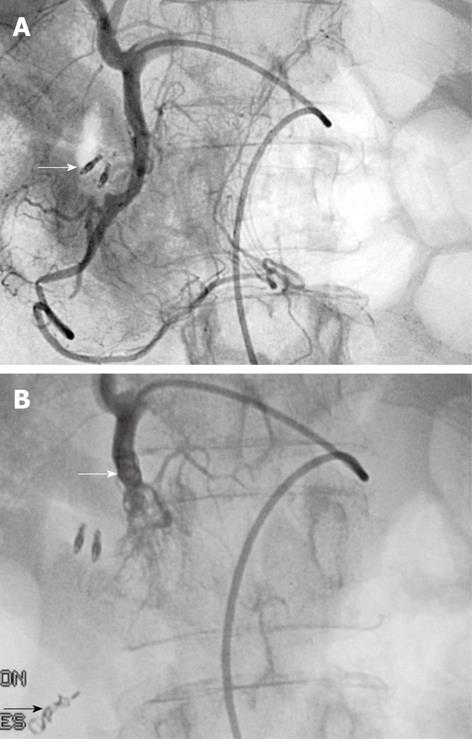
Figure 4 Typical sandwich embolization in a 75-year-old woman with bleeding from a postbulbar duodenal ulcer at endoscopy.
A: Angiography before embolization, guided by clip position (arrow): no evidence of active bleeding; B: Result after coil embolization of the distal and proximal GDA (with gelatine sponge in the arterial trunk), including the anterior and posterior superior pancreaticoduodenal arteries and the right gastroepiploic artery, to prevent retrograde flow (arrows). No ischemic complications were reported.
- Citation: Loffroy R, Guiu B. Role of transcatheter arterial embolization for massive bleeding from gastroduodenal ulcers. World J Gastroenterol 2009; 15(47): 5889-5897
- URL: https://www.wjgnet.com/1007-9327/full/v15/i47/5889.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5889