Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Jan 21, 2009; 15(3): 280-288
Published online Jan 21, 2009. doi: 10.3748/wjg.15.280
Published online Jan 21, 2009. doi: 10.3748/wjg.15.280
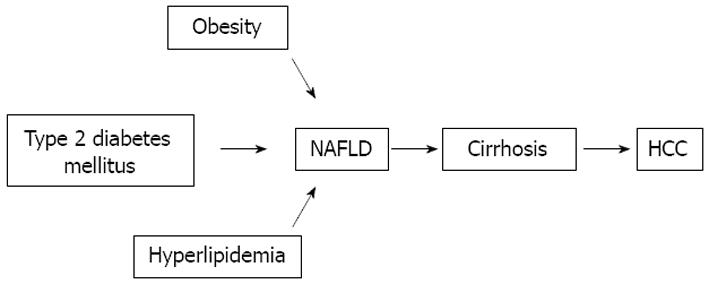
Figure 1 Type 2 diabetes mellitus may give raise to non-alcoholic fatty liver disease (NAFLD) which could progress to cirrhosis and hepatocellular carcinoma (HCC).
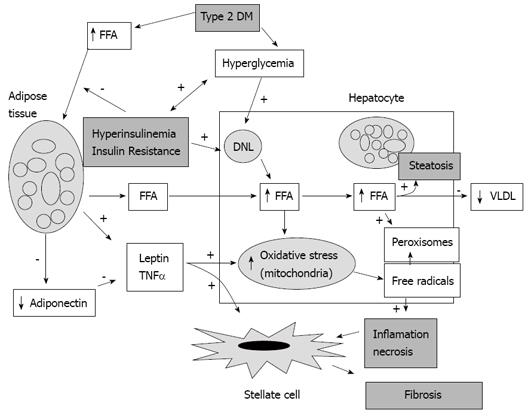
Figure 2 Liver damage caused by type 2 DM.
Insulin resistance promotes release of free fatty acids (FFA) from adipose tissue. The FFAs are accumulated in the liver cells, and de novo liponeogenesis (DNL) contributes also. The reduced secretion of very low density lipoprotein (VLDL) by hepatic cells saturates hepatocytes producing steatosis. Mitochondrial oxidative stress is increased as a result of excess intracellular FFAs and the influence of adipokines (leptin and tumor necrosis factor alpha (TNF-α). Excess of oxidative stress produces free radicals which in turn induces inflammation and cellular necrosis. Tissue inflammation stimulates the stellate cells to produce collagen.
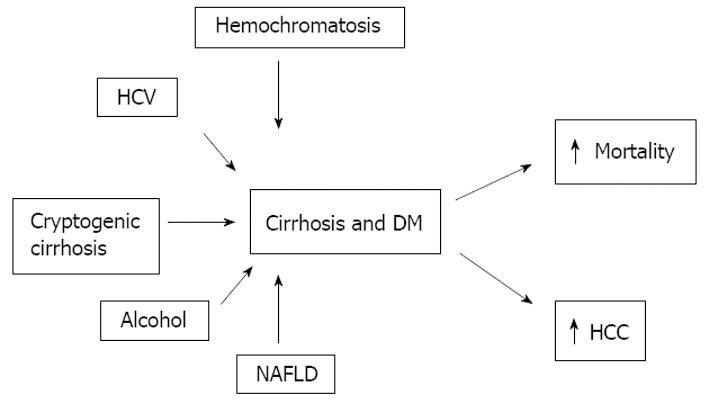
Figure 3 Etiology of liver cirrhosis most frequently associated with diabetes mellitus.
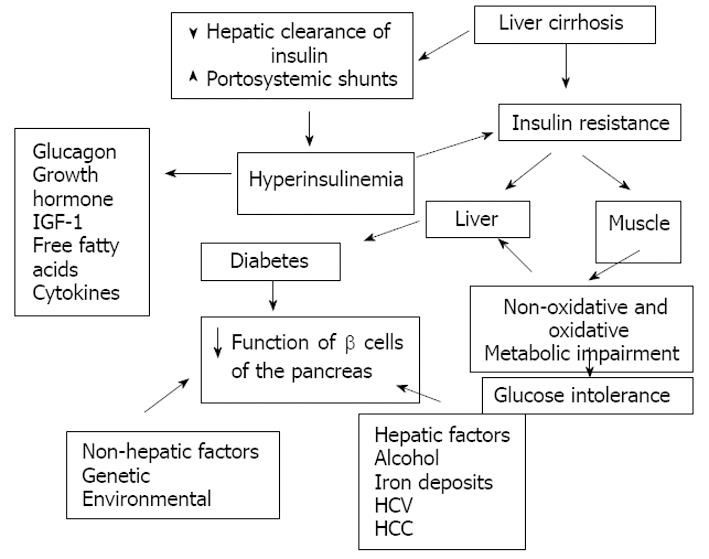
Figure 4 Pathophysiology of hepatogenous diabetes.
One of the main abnormalities is insulin resistance in muscular cells and the hepatic tissue. Insulin resistance in muscle impairs non-oxidative and oxidative glucose metabolism. The reduction of insulin clearance by the damaged liver and the presence of portosystemic shunts in one hand and the desensitization of the beta cells of the pancreas produced by diverse factors on the other hand may produce hyperinsulinemia. With progression of the diabetes there is a reduction in sensitivity of β-cells for production of insulin.
- Citation: Garcia-Compean D, Jaquez-Quintana JO, Gonzalez-Gonzalez JA, Maldonado-Garza H. Liver cirrhosis and diabetes: Risk factors, pathophysiology, clinical implications and management. World J Gastroenterol 2009; 15(3): 280-288
- URL: https://www.wjgnet.com/1007-9327/full/v15/i3/280.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.280