Copyright
©2008 The WJG Press and Baishideng.
World J Gastroenterol. Jun 28, 2008; 14(24): 3781-3791
Published online Jun 28, 2008. doi: 10.3748/wjg.14.3781
Published online Jun 28, 2008. doi: 10.3748/wjg.14.3781
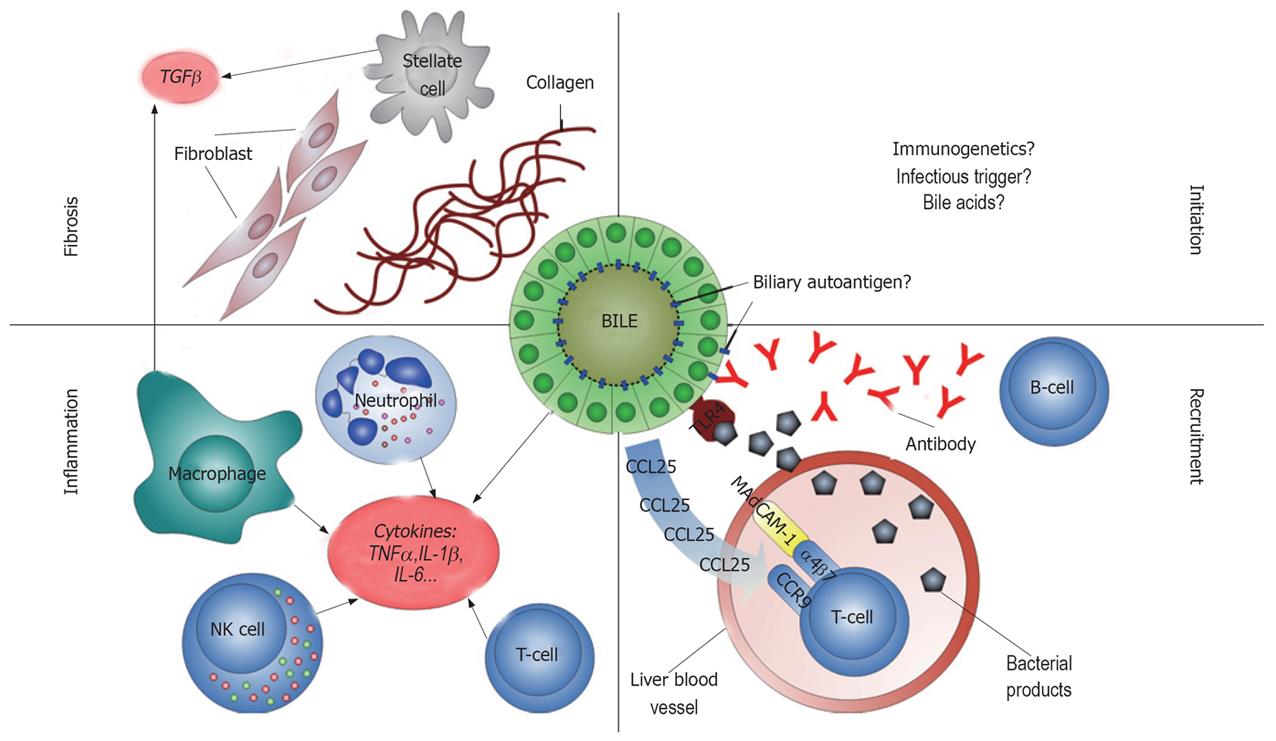
Figure 1 Schematic illustration of key elements of PSC pathogenesis.
Initiation (upper right): The initiating factor(s) of PSC pathogenesis are unknown. Immunogenetic factors (including the presentation of autoantigens on PSC associated HLA molecules), an infectious trigger, and toxic or immunological effects from bile acids have been proposed. Recruitment (lower right): Autoantibodies produced by B-lymphocytes bind to biliary epithelial cells (BECs), leading to inflammation when there is concomitant stimulation of toll like receptors (TLRs) by bacterial products [LPS and other pathogen-associated molecular patterns (PAMPs)] from the gut. Recruitment of gut-primed (α4β7) T-lymphocytes in inflammatory bowel disease may contribute to the inflammation because of aberrant expression of the MadCAM-1 ligand in the endothelium and production of the CCL25 chemokine by BECs. Inflammation (lower left): T-lymphocytes and natural killer (NK) cells predominate in PSC affected livers, but neutrophils and macrophages are also recruited. Together with activated BECs they are sources of the cytokines and chemokines that perpetuate the inflammation in PSC. A specific cellular component of neutrophils (tubulin beta 5 chain), has been hypothesized to serve as an autoantigen in this inflammatory process, possibly cross-reacting with the bacterial homolog FtsZ and leading to the generation of anti-neutrophil cytoplasmic antibodies (ANCAs). Fibrosis (upper left): Characteristically in PSC, there is extensive fibrosis and stricturing of the bile ducts. Resulting from the inflammation and possibly concomitant bile leakage, pro-fibrotic factors [e.g. transforming growth factor beta (TGF-β)] from macrophages and/or stellate cells are ultimately responsible for the fibrotic obliteration of the bile ducts and liver cirrhosis in PSC.
- Citation: Hov JR, Boberg KM, Karlsen TH. Autoantibodies in primary sclerosing cholangitis. World J Gastroenterol 2008; 14(24): 3781-3791
- URL: https://www.wjgnet.com/1007-9327/full/v14/i24/3781.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3781