Copyright
©2007 Baishideng Publishing Group Co.
World J Gastroenterol. Dec 28, 2007; 13(48): 6458-6464
Published online Dec 28, 2007. doi: 10.3748/wjg.v13.i48.6458
Published online Dec 28, 2007. doi: 10.3748/wjg.v13.i48.6458
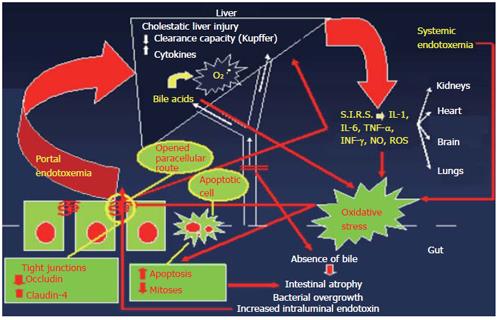
Figure 1 Pathophysiology of obstructive jaundice-induced gut barrier failure, endotoxemia and systemic complications.
Absence of intraluminal bile deprives the gut from its bacteriostatic, endotoxin-neutralizing and mucosal-trophic effect leading to increased intestinal bacterial and endotoxin load and mucosal atrophy. These alterations promote bacterial and endotoxin translocation into portal circulation and subsequently, through a decreased clearance capacity of Kupffer cells because of cholestasis, into systemic circulation. Systemic endotoxemia activates a systemic inflammatory response, which is associated with dysfunction of remote organs, while it further aggravates intestinal barrier dysfunction and cholestatic liver injury. Endotoxemia, cytokinemia and increased bile acids concentrations represent important promoters of reactive oxygen species formation in diverse organs, encompassing the intestine. Increased intestinal oxidative stress in obstructive jaundice, contributes to induction of apoptosis and inhibition of cell proliferation in intestinal crypts, leading to mucosal atrophy. In parallel, intestinal oxidative stress, endotoxemia, systemic release of inflammatory mediators and absence of intraluminal bile, disrupts the integrity of enterocytes’ tight junctions by altering the expression of their molecular components. As a consequence the intestinal paracellular route opens, contributing to further escape of endotoxin from the intestinal lumen into portal circulation, thus leading to a vicious cycle.
- Citation: Assimakopoulos SF, Scopa CD, Vagianos CE. Pathophysiology of increased intestinal permeability in obstructive jaundice. World J Gastroenterol 2007; 13(48): 6458-6464
- URL: https://www.wjgnet.com/1007-9327/full/v13/i48/6458.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i48.6458