Copyright
©2007 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 21, 2007; 13(3): 408-413
Published online Jan 21, 2007. doi: 10.3748/wjg.v13.i3.408
Published online Jan 21, 2007. doi: 10.3748/wjg.v13.i3.408
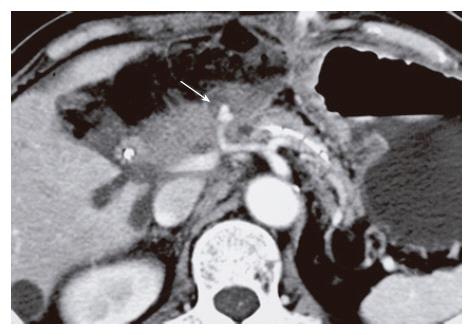
Figure 1 A 66-year-old female with pylorus-preserving pancreaticoduodenectomy (12 d after surgery).
A contrast-enhanced CT scan presents a pseudoaneurysm on the distal side of the common hepatic artery (arrow).
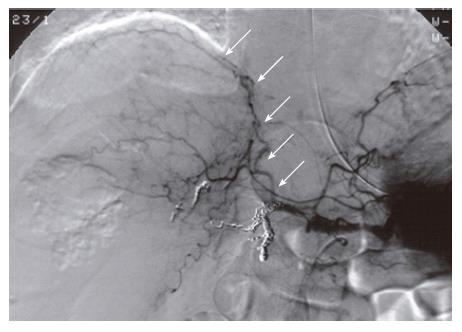
Figure 2 A 74-year-old male with left hepatic lobectomy (105 d after surgery).
The right inferior phrenic artery (arrows) is presented as a collateral pathway to the liver on an angiography after TAE for the proper hepatic and gastroduodenal arteries.
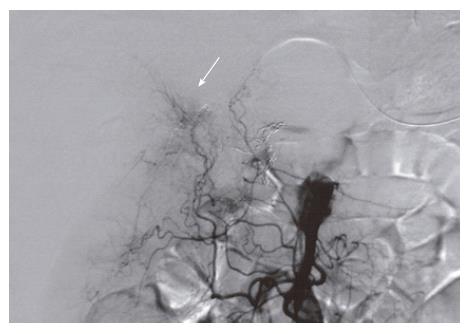
Figure 3 The jejunal branches (arrow) are seen as a collateral pathway to the liver in the same patient as in Figure 2.
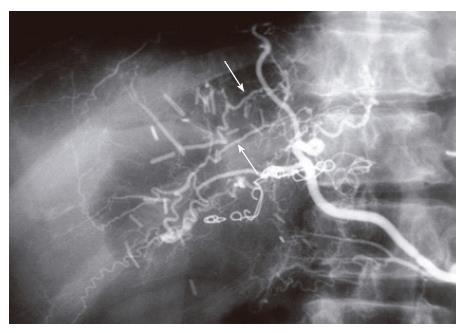
Figure 4 A 71-year-old male with left hepatic lobectomy (41 d after surgery).
The intrahepatic communicating branches (arrows) are visualized via the branches of the right inferior phrenic artery on an angiography after TAE for the right hepatic artery.
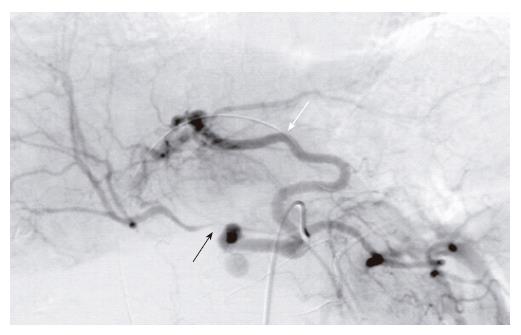
Figure 5 A diagnostic celiac angiography showing a stenosis of the right hepatic artery (black arrow) distal to the ruptured hepatic artery pseudoaneurysm in the same patient as in Figure 1.
The aberrant left hepatic artery (white arrow) originating from the left gastric artery was dilated and supplied arterial blood flow to the right hepatic artery through the intrahepatic communicating branches before TAE.
- Citation: Tajima Y, Kuroki T, Tsutsumi R, Sakamoto I, Uetani M, Kanematsu T. Extrahepatic collaterals and liver damage in embolotherapy for ruptured hepatic artery pseudoaneurysm following hepatobiliary pancreatic surgery. World J Gastroenterol 2007; 13(3): 408-413
- URL: https://www.wjgnet.com/1007-9327/full/v13/i3/408.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i3.408