Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 28, 2006; 12(4): 526-538
Published online Jan 28, 2006. doi: 10.3748/wjg.v12.i4.526
Published online Jan 28, 2006. doi: 10.3748/wjg.v12.i4.526
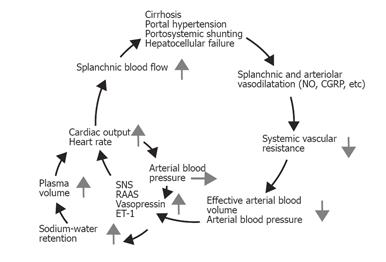
Figure 1 Pathophysiology of the splanchnic and peripheral arteriolar vasodilation and systemic hemodynamic changes in cirrhosis.
Endogenous vasodilators may escape hepatic degradation, owing to portosystemic shunting and/or hepatocellular damage, and induce vasodilatation preferentially in the splanchnic vascular area. Reduced systemic and splanchnic vascular resistance leads to a reduced effective arterial blood volume, and hence to activation of vasoconstrictor systems. The hemodynamic and clinical consequences are increases in cardiac output, heart rate, and plasma volume and decreased renal blood flow, low arterial blood pressure, and fluid and water retention. The development of the hyperdynamic circulation may increase portal inflow and further aggravate the portal pressure in a vicious cycle. SNS, sympathetic nervous system; RAAS, renin-angiotensin-aldosterone system; ET-1, endothelin-1.
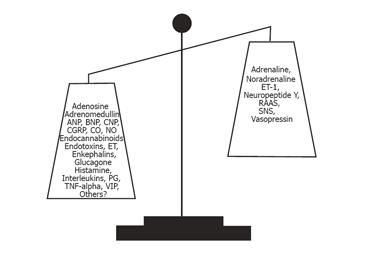
Figure 2 Imbalance between vasoconstricting and vasodilating forces.
ANP, atrial natriuretic peptide; BNP and CNP: B- and C-type natriuretic peptides; CGRP, calcitonin gene-related peptide; ET, endothelin;, TNF-α, tumor necrosis factor α; VIP, vasoactive intestinal polypeptide; RAAS, The renin–angiotensin–aldosterone system; SNS, The sympathetic nervous system.
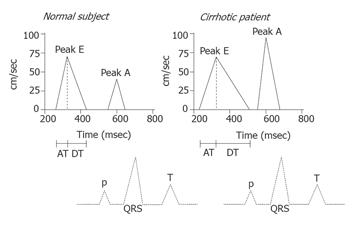
Figure 3 Diagram of the transmitral Doppler flow signal in the healthy state and in a patient with cirrhosis.
The Doppler flow profile reflects the early filling of the ventricle (Peak E) and the late atrial contribution to its filling (Peak A). A decrease in the E/A ratio and prolonged acceleration time (AT) and deceleration time (DT) indicate diastolic dysfunction, as illustrated in the right panel. The broken lines are the time-related electrocardiogram.
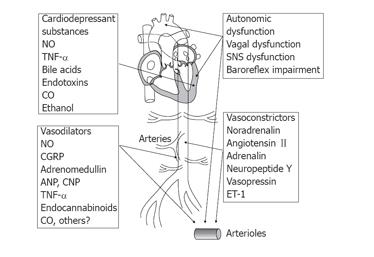
Figure 4 Vascular hyporeactivity in cirrhosis may originate in the central nervous system, the autonomic nervous system, from local mediators, or within the smooth muscle cell/heart muscle cell.
An autonomic dysfunction may act at cardiac, arterial, and arteriolar levels. Vasodilators and vasoconstrictors may act variably at cardiac, arterial, and arteriolar levels. At the smooth cellular (arteriolar) level, hyporeactivity may be caused by increased concentrations of vasodilators (NO, nitric oxide; CGRP, calcitonin gene-related peptide; ANP, atrial natriuretic peptide; TNF-α, tumor necrosis factor-alpha; endocannabinoids; CO: carbon monoxide) and/or decreased sensitivity to vasoconstrictors (ET-1: endothelin-1).
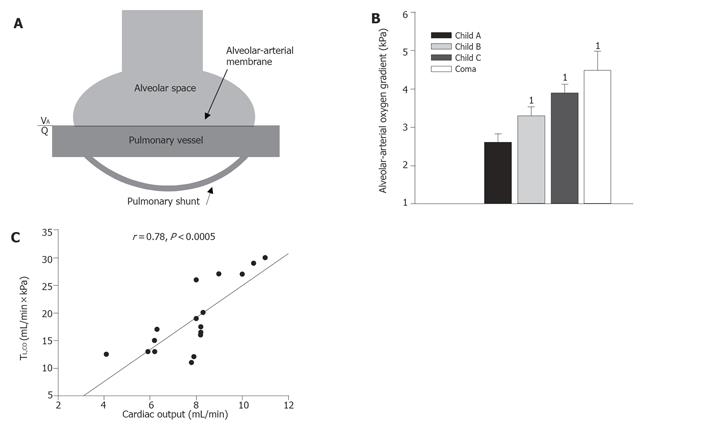
Figure 5 Panel A.
Lung diffusion and blood oxygenation depend on the diffusion properties of the alveolar-arterial membrane, the degree of arterial-venous shunting through pulmonary shunts, and the degree of ventilation-perfusion inequality (VA/Q). Panel B. The alveolar-arterial oxygen gradient increases with the severity of liver disease e.g. graduated according to the Child-Turcotte classification with the highest values in patients with hepatic coma. 1denotes significant difference from Child class A patients (from Ref. [143]). Panel C. In cirrhosis, the diffusing capacity bears a direct relation to the increased cardiac output and to the central blood volume (not shown). Data from Ref. [45].
- Citation: Møller S, Henriksen JH. Cardiopulmonary complications in chronic liver disease. World J Gastroenterol 2006; 12(4): 526-538
- URL: https://www.wjgnet.com/1007-9327/full/v12/i4/526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i4.526