Copyright
©2005 Baishideng Publishing Group Inc.
World J Gastroenterol. Nov 21, 2005; 11(43): 6848-6852
Published online Nov 21, 2005. doi: 10.3748/wjg.v11.i43.6848
Published online Nov 21, 2005. doi: 10.3748/wjg.v11.i43.6848
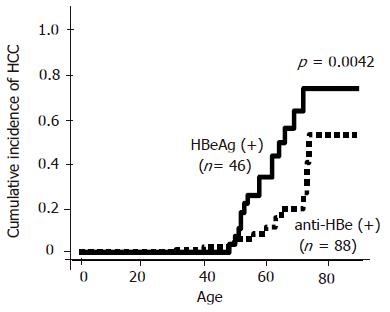
Figure 1 Cumulative incidence of HCC in patients with HBeAg or anti-HBe (Kaplan–Meier analysis and log-rank test).
The incidence of HCC in both groups was increasing after the age of 50. The incidence of HCC was significantly higher in the patients with HBeAg positive (solid line) than those with anti-HBe positive (dot line) (P=0.0042).
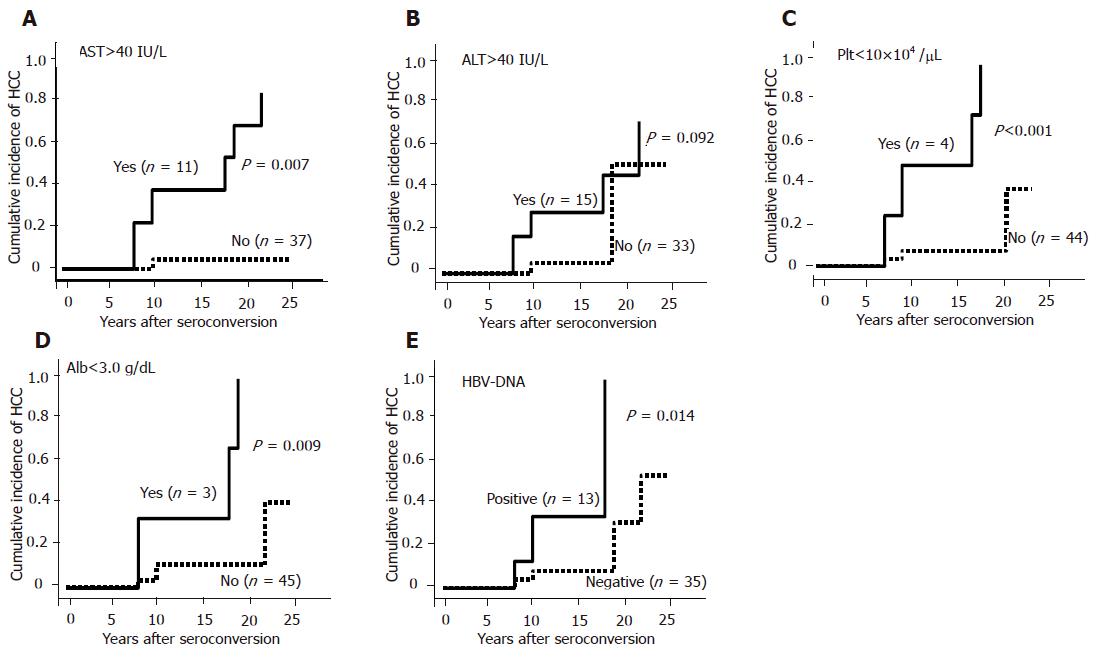
Figure 2 Cumulative incidence of HCC in patients with different parameters (Kaplan–Meier analysis and log-rank test).
A: AST level (>40 or ≤40 IU/L); B: ALT level (>40 or ≤40 IU/L); C: platelet counts (<10×104 or ≥10×104/μL): D: albumin level (<30 or ≥30 g/L); E: HBV-DNA (positive or negative).
Figure 3 Cumulative incidence of HCC in patients after seroconversion (Kaplan–Meier analysis and log-rank test).
A: Spontaneous or post-therapeutic seroconversion; B: age at seroconversion (>40 or ≤40 years).
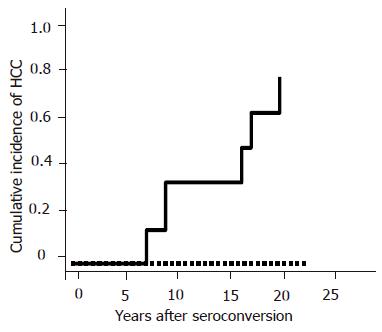
Figure 4 Cumulative incidence of HCC in patients with or without risk factors (Kaplan–Meier analysis and log-rank test).
Solid line: either platelet counts<10×104/μL or AST>40 IU/L; dot line: both platelet counts≥10×104/μL, and AST<40 IU/L.
- Citation: Murata K, Sugimoto K, Shiraki K, Nakano T. Relative predictive factors for hepatocellular carcinoma after HBeAg seroconversion in HBV infection. World J Gastroenterol 2005; 11(43): 6848-6852
- URL: https://www.wjgnet.com/1007-9327/full/v11/i43/6848.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i43.6848