Copyright
©2005 Baishideng Publishing Group Inc.
World J Gastroenterol. Mar 14, 2005; 11(10): 1426-1432
Published online Mar 14, 2005. doi: 10.3748/wjg.v11.i10.1426
Published online Mar 14, 2005. doi: 10.3748/wjg.v11.i10.1426
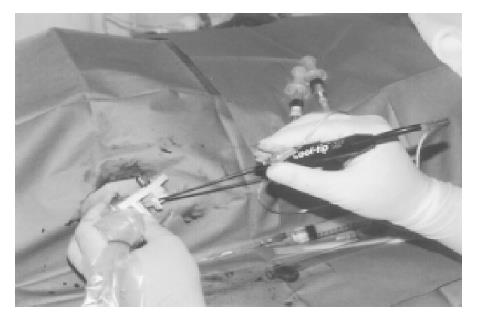
Figure 1 Appearance of PEI-RFA treatment.
A 17-gauge RFA needle with 2 or 3 cm electrode was first inserted into the tumor through the hole of the attachment beside the echo probe, and then 21-gauge PEI needle was inserted through the same hole. RFA was performed immediately after injecting the ethanol into the tumor. The ablation was performed under the impedance control. The amount of ethanol injected into the tumors was always kept below the double of the estimated tumor volume and the injection of ethanol was ceased if resistance to the injection was felt.
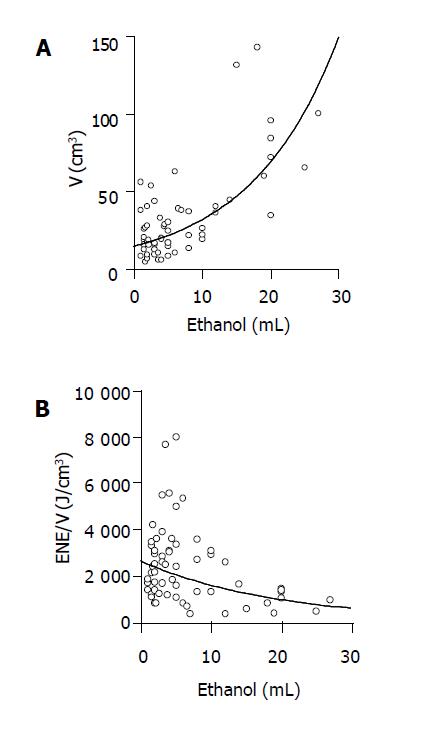
Figure 2 Relationship between the amount of ethanol injected and the volume of coagulated necrosis or the energy requirement for inducing per unit volume of coagulated necrosis in PEI-RFA.
PEI-RFA was performed on 60 patients with HCC. The ablation was done by using the Cool-tip RF system. The amount of ethanol injected into tumors positively correlated with the volume of coagulated necrosis (A: r = 0.71, P<0.0001) and it negatively correlated with the energy requirement for inducing per unit volume of coagulated necrosis (B: r = -0.41, 0.014).
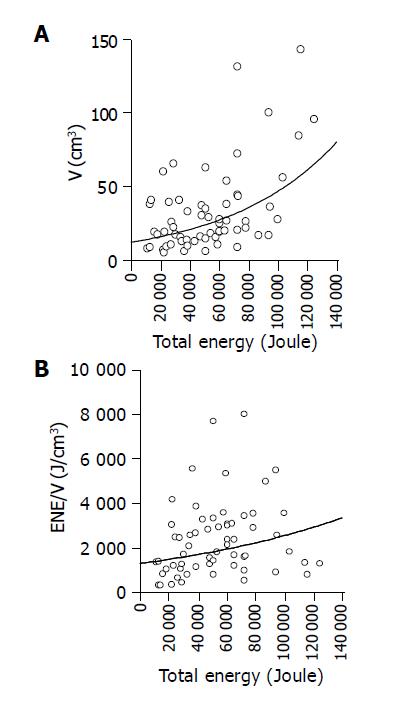
Figure 3 Relationship between the amount of total energy requirement and the volume of coagulated necrosis or the energy requirement for inducing per unit volume of coagulated necrosis in PEI-RFA.
PEI-RFA was performed on 60 patients with HCC. The ablation was done by using the Cool-tip RF system. The amount of total energy requirement positively correlated with the volume of coagulated necrosis (r = 0.47, P = 0.0013), whereas no significant correlation was admitted between the total amount of energy requirement and the energy requirement for inducing per unit volume of coagulated necrosis (r = 0.35, P = 0.13) in PEI-RFA.
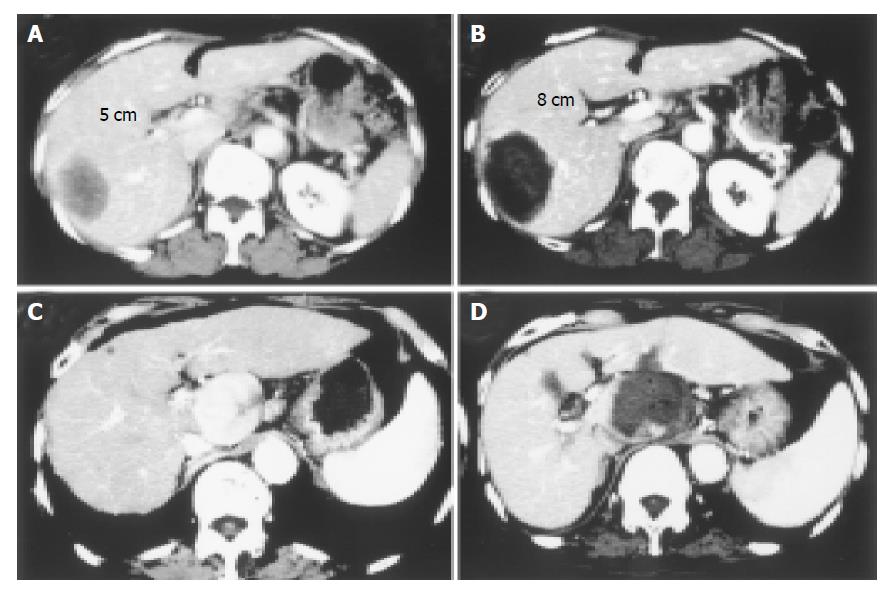
Figure 4 Two cases with large-sized HCC treated with PEI-RFA are shown.
Contrast-enhanced CT before (A: delay phase, C: early vascular phase) and after (B: delay phase, D: delay phase) PEI-RFA. Massive HCCs of 5 cm in the longest diameter were located in the right lobe of the liver in both cases. In the first case (A and B), RFA was started at 30 W and the power output was increased stepwise to 100 W every two min and the ablation was performed for 20 min. In the second case (C and D), because the tumor was located close by blood vessel such as inferior vena cava, portal tract and aorta, it was likely to be difficult to treat with RFA under high power control. After injecting 19 mL of ethanol into the tumor, one session of RFA was performed at 30 W for 12 min. The massive tumor was completely eliminated by PEI-RFA.
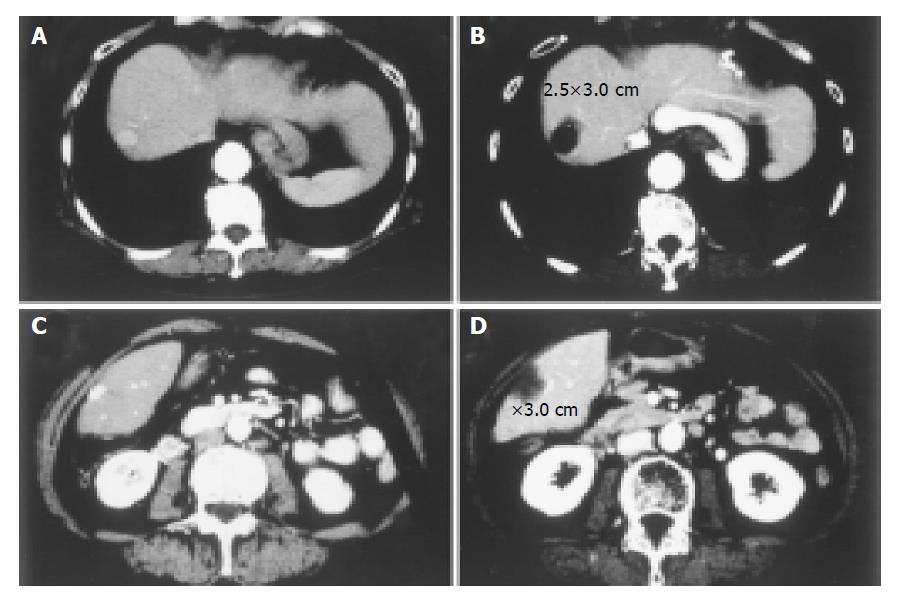
Figure 5 Two cases with small-sized HCCs treated with PEI-RFA under low power output control are shown.
Contrast-enhanced CT before (A, C) and after (B, D) PEI-RFA. Small HCCs of 1.5 cm in the longest diameter were located in the S8 region of the liver in both cases. In both cases, RFA was performed at 40 W for 5 min. Though the ablation was performed at relatively low power output for short duration, the coagulated necrosis larger than 2.5 cm was induced after the treatment.
- Citation: Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Miyauchi Y, Himoto T, Kimura Y, Nakai S, Deguchi A, Yoneyama H, Yoshida S, Kuriyama S. Comparison between combination therapy of percutaneous ethanol injection and radiofrequency ablation and radiofrequency ablation alone for patients with hepatocellular carcinoma. World J Gastroenterol 2005; 11(10): 1426-1432
- URL: https://www.wjgnet.com/1007-9327/full/v11/i10/1426.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i10.1426