Published online Dec 16, 2015. doi: 10.12998/wjcc.v3.i12.1000
Peer-review started: July 7, 2015
First decision: July 29, 2015
Revised: August 19, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: December 16, 2015
IgG4-related disease (IgG4-RD) is an immune-mediated fibroinflammatory disorder that can occur in almost all systemic organs and generally responds to corticosteroid treatment. We report a rare case of an IgG4-related intrapelvic mass lesion that responded to steroid therapy but caused a fistula between the sigmoid colon and bladder. A 71-year-old man was followed after treatment for hepatocellular carcinoma. Follow-up computed tomography (CT) incidentally depicted left hydronephrosis with an ill-demarcated intrapelvic mass lesion. This lesion was histologically diagnosed as IgG4-RD by open biopsy, and peroral steroid therapy was initiated. One month after starting steroids, a colovesical fistula was detected by follow-up CT. A colostomy and urethral catheterization were emergently performed. The patient recovered and the mass lesion was drastically minimized by the initiation of glucocorticoids; however, he still needs urethral catheterization. IgG4-RD develops in various systemic organs and generally responds well to steroids. Clinicians must be watchful for the complications of responses to corticosteroids, such as fistulization, when the mass lesion of IgG4-RD is adjacent to multiple luminal organs.
Core tip: IgG4-related disease (IgG4-RD) is an immune-mediated fibroinflammatory condition that is effectively treated with glucocorticoids. Progression of this disease may cause serious complications or several symptoms; hence, glucocorticoid therapy is often inevitable. To date, critical adverse events caused by steroid treatment for IgG4-RD have seldom been reported. The current case report describes a rare, but severe, adverse event of colovesical fistula following a good response to glucocorticoids.
- Citation: Yabuuchi Y, Matsubayashi H, Matsuzaki M, Shiomi A, Moriguchi M, Kawamura I, Ito I, Ono H. Colovesical fistula caused by glucocorticoid therapy for IgG4-related intrapelvic mass. World J Clin Cases 2015; 3(12): 1000-1004
- URL: https://www.wjgnet.com/2307-8960/full/v3/i12/1000.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i12.1000
IgG4-related disease (IgG4-RD) is recognized as an autoimmune disorder that can affect multiple systemic organs through the formation of fibroproliferative and/or tumefactive lesions. Today, the disease concept and diagnostic criteria of IgG4-RD are globally widespread, and opportunities to diagnose and treat this disease are increasing. Patients with active IgG4-RD tend to demonstrate multiple systemic lesions[1,2], and therefore, often meet the indications for glucocorticoid therapy. Glucocorticoid is effective for most IgG4-related lesions; however, the period before a response to steroid is observed may vary depending on the affected organ or the degree of fibrosis[3]. A response is usually recognized in two weeks to a month following the initiation of steroids[1,4].
In general, corticosteroids improve the lesions or symptoms associated with IgG4-RD, while concerns regarding adverse effects of glucocorticoid therapy are well known and limited. We herewith report a patient who developed a colovesical fistula caused by glucocorticoid therapy to treat an IgG4-related intrapelvic mass and subsequently required surgical treatment.
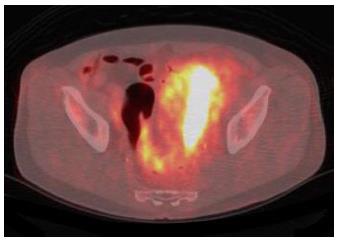
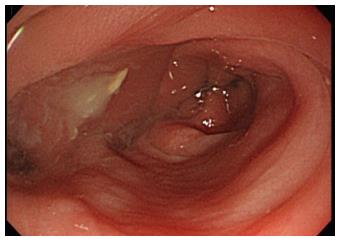
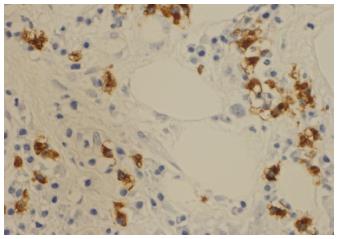
The patient, a 71-year-old man with a history of hepatitis C and hepatocellular carcinoma, had been treated with interferon, percutaneous ethanol injection, transcatheter arterial chemoembolization, and radio frequent ablation, and had been continuously followed up with clinical images. Follow-up computed tomography (CT) incidentally revealed left hydronephrosis and an ill-demarcated mass lesion extending to the left lower ureter, left margin of the bladder, and sigmoid colon (Figure 1). 18F-fluorodeoxyglucose positron emission tomography demonstrated strong uptake around the left lower ureter (SUV max: 19.0) (Figure 2). Colonoscopy showed a severe extrinsic compression at the sigmoid colon (Figure 3). Cystoscopy demonstrated whitish edematous protrusions at the upper left area of the bladder but the left ureteral orifice was intact. Under the suspected diagnosis of left-lower ureter cancer invading the adjacent organs, transurethral resection was performed for a histological diagnosis. Histology of the TUR specimens revealed intraepithelial papillary urothelial carcinoma (G1, low grade, pTa), which was not invasive, contradicting our previous diagnosis. An open biopsy was done for a conclusive diagnosis of the intrapelvic mass lesion. Histology of the biopsied material did not show cancerous tissue, but dense fibrous tissue with abundant lymphoplasmacyte infiltration. Immunohistochemistry by using mouse anti-human IgG4 monoclonal antibody in enzyme immunoassay revealed ≥ 10 IgG4 positive cells per high-power field (Figure 4), although the ratio of IgG4/IgG positive cells was < 40%. Serum IgG4 was then examined and found elevated (190 mg/dL, normal range: 4.8-105 mg/dL). With these results, we diagnosed “Possible IgG4-RD”, based on the comprehensive diagnosis criteria[5]. Glucocorticoid therapy was initiated with 40 mg/d of prednisolone and tapered in the standard pitch[6] to treat the hydronephrosis due to the IgG4-related mass lesion and subsequently recover renal function.
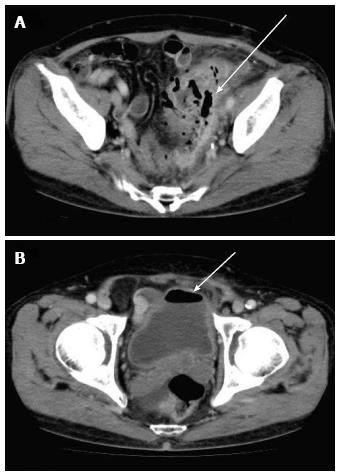
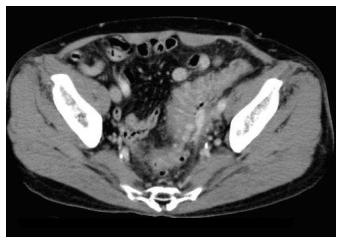
One month later, the patient visited the hospital for evaluation of his steroid response, but he had a continued moderate fever, diarrhea, and urine with a feces odor for a few days. CT demonstrated shrinkage of the intrapelvic mass lesion, as well as extraluminal air in the mass lesion and bladder (Figure 5). The laboratory findings showed leukocytosis (white blood cell: 21480/μL), thrombocytopenia (platelet: 3.4 × 104/μL), elevated C-reactive protein (14.87 mg/dL), and renal dysfunction (creatinine: 1.64 mg/dL). Large quantities of bacteria (Escherichia coli and Enterococcus faecalis, etc.) were detected in urine cultures, and fistulization between the urinary bladder and sigmoid colon with enteric bacterial infection of the mass lesion was confirmed. A percutaneous drainage was placed into the infected mass lesion, and colostomy was performed with urethral catheterization and antibiotic administration as emergent management. The patient gradually recovered and was discharged in two weeks. He has been in good health subsequently, and the intrapelvic mass has remained minimized with a maintenance dose of prednisolone (Figure 6). However, he has sometimes experienced urinary incontinence from the anus when the urethral catheter is occluded.
Eight months after steroid initiation with 5 mg/d of prednisolone, the screening cystoscopy revealed a polypoid lesion near the fistula. The recurrence of superficial bladder cancer was ruled out by a repeat TUR. This histology and response to glucocorticoid provided diagnostic confirmation[3,5,7]. Today, the remaining fistula is still visible with a cystoscope, so that the urethral catheter cannot be withdrawn and the artificial anus has been unclosed for nearly two years.
Standard therapy for IgG4-RD is peroral steroid therapy in the form of prednisolone initiated at a dose of 0.6 mg/kg with subsequent tapering[3,6,7]. Glucocorticoids are highly effective in treating IgG4-RD and a response to steroids can be seen in most systemic lesions within 2-4 wk as determined by clinical images[1,6]. The current case also responded well to standard glucocorticoid therapy; however, this response caused a fistula between the urinary bladder and sigmoid colon.
To date, severe complications have been described in many cases with IgG4-RD; however, these are related to the occurrence or progression of the disease, rather than adverse steroid responses. For example, complications of IgG4-RD have included clinical emergencies such as leptomeningitis with rapidly progressive cognitive decline, gastric-pericardial fistula, aortoduodenal fistula, stenosis of the coronary arteries, stenosis of the colon, and splenic haemorrhage[8-13]. A case of IgG4-related inflammatory pseudotumor of the urinary bladder causing a colovesical fistula, similar to the present case, has also been reported[14]. However, these complications are all caused by the progression of the disease and are not results of glucocorticoid therapy. To the best of our knowledge, based on a PubMed keyword survey, this is the first report of a severe complication due to a good response to corticosteroid therapy in a case of IgG4-RD.
A colovesical fistula can occur in various diseases. Common causes are colonic diverticula, inflammatory bowel disease, and carcinomas of the colon, urological, and gynecological organs. A gastrointestinal foreign body, trauma, and iatrogenic injuries are rare causes[15]. A colovesical fistula usually develops as a consequence of the progression of these diseases; however, fistulization rarely occurs in cases of malignancy treated with chemotherapy or radiation therapy[16]. Fistulas are thought to arise simply due to more rapid shrinkage and necrosis of the tumor compared with slow repair of the interstitial tissue. A similar explanation is speculated for the fistula formation observed in the current case.
Predicting the risk of the fistulization is difficult in cases with IgG4-RD. In the present case, the mass lesion was adjacent to multiple luminal organs. This condition might be one of the risk factors that led to fistulization. A widespread area affected by the stromal tissue, the level of inflammatory cell infiltration, and colonic diverticula might be also the risk factors. Earlier detection could increase the chance of a cure or prevention of severe complications.
After the initiation of steroids, we examined abdominal ultrasonography at two weeks and CT at one month, as the response to glucocorticoid can be usually obtained within this timeframe in cases with IgG4-RD[1,6]. Although long-term risk of complications by the accumulated radiation dose is a concern, CT is a suitable modality for the evaluation of the steroid response, colovesical fistula, and adjacent anatomical structures[17]. During the early period after the initiation of glucocorticoids, the IgG4-related mass lesions located at rare sites must be followed using a suitable image modality.
In conclusion, fistulization between the bladder and sigmoid colon occurred after glucocorticoid therapy in a case with IgG4-RD. An intrapelvic mass adjacent to multiple luminal organs, a wide range of spread of the mass lesion and the good response to glucocorticoids may have caused this severe complication. Early follow-up imaging as well as blood examination is necessary for the evaluation of the steroid response as well as the detection of complications arising in response to glucocorticoid treatment.
One month after the initiation of glucocorticoid therapy for IgG4-related disease, a 71-year-old man had a continued moderate fever, diarrhea, and urine with a feces odor for a few days.
The patient slightly had lower abdominal pain.
Fistulization between the bladder and colon due to colonic diverticulitis, inflammatory bowel disease and carcinomas of the colon or urological organs.
The laboratory findings showed leukocytosis, thrombocytopenia, elevated C-reactive protein and renal dysfunction, with large quantities of bacteria in urine cultures.
Computed tomography demonstrated shrinkage of the intrapelvic mass lesion, as well as extraluminal air in the mass lesion and bladder.
A percutaneous drainage was placed into the infected mass lesion, and colostomy was performed with urethral catheterization and antibiotic administration.
Fistulization have been described in some cases with IgG4-related disease, such as gastric-pericardial fistula and aortoduodenal fistula. However these are related to the progression of the disease.
This case was a rare complication of IgG4-related disease due to the good response to glucocorticoid therapy. Early follow-up imaging is necessary for the evaluation of the steroid response as well as the detection of complications arising in response to glucocorticoid treatment.
This case report is interesting and well documented.
P- Reviewer: Grizzi F, Nakamura T, Triadafilopoulos G S- Editor: Tian YL L- Editor: A E- Editor: Lu YJ
| 1. | Matsubayashi H, Yoneyama M, Nanri K, Sugimoto S, Shinjo K, Kakushima N, Tanaka M, Ito S, Takao M, Ono H. Determination of steroid response by abdominal ultrasound in cases with autoimmune pancreatitis. Dig Liver Dis. 2013;45:1034-1040. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Matsubayashi H, Sawai H, Kimura H, Yamaguchi Y, Tanaka M, Kakushima N, Takizawa K, Kadooka M, Takao T, Hebbar S. Characteristics of autoimmune pancreatitis based on serum IgG4 level. Dig Liver Dis. 2011;43:731-735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539-551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1856] [Cited by in F6Publishing: 1739] [Article Influence: 144.9] [Reference Citation Analysis (83)] |
| 4. | Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, Chari ST, Della-Torre E, Frulloni L, Goto H. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol. 2015;67:1688-1699. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 573] [Cited by in F6Publishing: 589] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 5. | Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 244] [Cited by in F6Publishing: 601] [Article Influence: 50.1] [Reference Citation Analysis (0)] |
| 6. | Kamisawa T, Shimosegawa T, Okazaki K, Nishino T, Watanabe H, Kanno A, Okumura F, Nishikawa T, Kobayashi K, Ichiya T. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009;58:1504-1507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 500] [Cited by in F6Publishing: 460] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 7. | Kamisawa T, Zen Y, Pillai S, Stone JH. IgG4-related disease. Lancet. 2015;385:1460-1471. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 794] [Cited by in F6Publishing: 771] [Article Influence: 85.7] [Reference Citation Analysis (0)] |
| 8. | Mehta SH, Switzer JA, Biddinger P, Rojiani AM. IgG4-related leptomeningitis: a reversible cause of rapidly progressive cognitive decline. Neurology. 2014;82:540-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Frydman J, Grunner S, Kluger Y. IgG4-related disease manifesting as an acute gastric-pericardial fistula. World J Gastroenterol. 2014;20:16782-16785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Sarac M, Marjanovic I, Bezmarevic M, Zoranovic U, Petrovic S, Mihajlovic M. An aortoduodenal fistula as a complication of immunoglobulin G4-related disease. World J Gastroenterol. 2012;18:6164-6167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 13] [Cited by in F6Publishing: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Patel NR, Anzalone ML, Buja LM, Elghetany MT. Sudden cardiac death due to coronary artery involvement by IgG4-related disease: a rare, serious complication of a rare disease. Arch Pathol Lab Med. 2014;138:833-836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Matsubayashi H, Kishida Y, Yoshida Y, Yoshida M, Tanaka Y, Igarashi K, Imai K, Ono H. Autoimmune pancreatitis with colonic stenosis: an unusual complication and atypical pancreatographic finding. BMC Gastroenterol. 2014;14:173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Hanna MS, Terlevich A, Przemioslo R, Marden P. Autoimmune pancreatitis complicated by spontaneous subcapsular splenic haemorrhage. JOP. 2013;14:502-505. [PubMed] [Cited in This Article: ] |
| 14. | Park S, Ro JY, Lee DH, Choi SY, Koo H. Immunoglobulin G4-associated inflammatory pseudotumor of urinary bladder: a case report. Ann Diagn Pathol. 2013;17:540-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Kiani QH, George ML, Carapeti EA, Schizas AM, Williams AB. Colovesical fistula: should it be considered a single disease? Ann Coloproctol. 2015;31:57-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Palmowski M, Zechmann C, Satzl S, Bartling S, Hallscheidt P. Large gastrosplenic fistula after effective treatment of abdominal diffuse large-B-cell lymphoma. Ann Hematol. 2008;87:337-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Golabek T, Szymanska A, Szopinski T, Bukowczan J, Furmanek M, Powroznik J, Chlosta P. Enterovesical fistulae: aetiology, imaging, and management. Gastroenterol Res Pract. 2013;2013:617967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |