Published online Jul 16, 2014. doi: 10.12998/wjcc.v2.i7.284
Revised: March 23, 2014
Accepted: May 19, 2014
Published online: July 16, 2014
Verrucous carcinoma of the esophagus is a variant of a squamous cell cancer. Our case is a 78-year-old male patient comes in with the dysphagia and weight loss, and on endoscopy (EGD) he is found to have an irregular intraluminal mass at the distal esophagus. With the deep EGD assisted biopsy, diagnosis of the verrucous carcinoma is made. Due to multiple co morbidities and possible infiltration to the pericardium, patient is taken for the esophageal stent placement and is being referred for the chemo-radiation treatment. The diagnosis can be very difficult to make with the superficial biopsies due to very non specific histological changes and requires very high clinical suspicion and deep mucosal biopsies are required for accurate diagnosis of the tumor. Chronic and local disease process is the main risk factor for the development of the verrucous carcinoma of the esophagus. Surgery is the treatment of the choice for the early stage tumor and advanced cases are treated with the palliation and possibly chemo- radiation. The prognosis is usually guarded and needs long term follow up.
Core tip: A verrucous carcinoma is a slow growing, well differentiated, rare form of squamous carcinoma variant. It is associated with chronic, local disease process and it invades locally. On endoscopy (EGD), it appears as an exophytic irregular warty projecting mass, and it is very difficult to diagnose by superficial biopsy due to non specific superficial histological findings. So it requires high index of suspicion and deep biopsy with EGD or endoscopic ultrasonography (EUS). It projects as hypoechoic mucosal thickening on EUS. Early stages of cancers are treated surgically. Advanced cases can be referred for esophageal stent placement for palliation and chemo radiation. It has high morbidity and mortality and requires long term follow up for accurate numbers regarding to the treatment and the follow up.
- Citation: Ramani C, Shah N, Nathan RS. Verrucous carcinoma of the esophagus: A case report and literature review. World J Clin Cases 2014; 2(7): 284-288
- URL: https://www.wjgnet.com/2307-8960/full/v2/i7/284.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i7.284
Verrucous carcinoma of the esophagus is a rare form of carcinoma of squamous cell origin[1-9]. Majority of the cases are associated with the smoking, reflux esophagitis, alcohol use, human papilloma virus (HPV), achalasia and few other chronic inflammatory conditions[1-9]. An incidence rate of such cancer has been shown to be higher in males than females with a ratio of 2:1 and seen in the group from 35 to 80 years[1-3,6]. Superficial biopsies of the lesion often show merely chronic inflammation with no high grade dysplasia, which makes it difficult to diagnose.
So far, less than 30 cases of such carcinomas are reported in the English literature. We are presenting a case of the verrucous carcinoma of the esophagus with no documented risk factors associated with the carcinoma and a diagnosis is made by deep biopsies of the lesions.
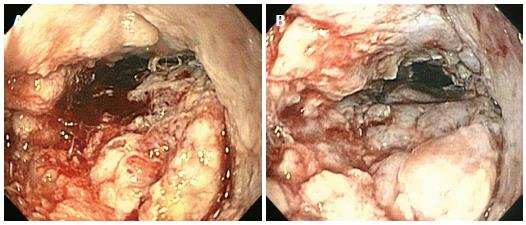
We have recently seen a 78-year-old African American man, presenting with dysphagia, weight loss of 15 Lbs over 4-5 wk and right lower quadrant dull, and non radiating abdominal pain. His past medical history included coronary artery disease status post angioplasty with stent placement, hypertension, dyslipidemia, and diabetes mellitus with complications including diabetic retinopathy and nephropathy. He was non-smoker and non-drinker and denied any history of GERD. And symptoms were gradual in onset over last couple of months. His physical exam showed no abnormality. On lab evaluation, His BUN and serum creatinine were 42 and 2.4 respectively, normal liver function tests; Hemoglobin was 12.4 g/dL with MCV 84.4 fl. All other labs were within normal limits. ultrasonography of the abdomen and computed tomography (CT) scan of the abdomen and pelvis were unremarkable for any hepatobilliary, pancreatic or intestinal pathology. He underwent barium esophagogram, and was found to have a long, irregular stricture involving the mid and distal esophagus with an apparent intraluminal mass at its proximal end. The endoscopic examination showed a luminal warty appearing mass occupying distal 8 cm of the esophagus (Figure 1). Endoscopic ultrasonography (EUS) examination was performed which showed solid tumor measuring approx 5 cm in greatest dimension, possibly infiltrating into the pericardium (Figure 2). It also showed hypoechoic concentric wall thickening that appeared to be either an inflammatory process or lymphoma.
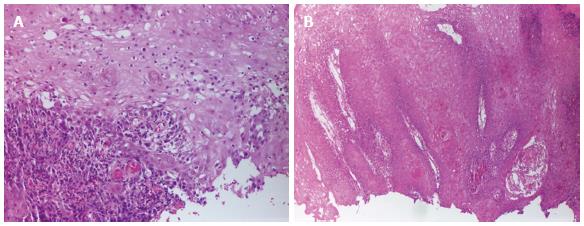
Initial biopsies were remarkable for squamous epithelial cells with parakeratosis and marked acute and chronic inflammation, ulceration and focal squamous cell with atypia. The repeat endoscopic examination and extensive biopsies with jumbo forceps revealed the diagnosis of verrucous carcinoma of the esophagus. In situ hybridization for both high and low risk HPV was negative.
A CT scan of the chest showed some mediastinal lymph nodes. Bone scan showed no any bone metastasis. In view of the dysphagia, patient underwent endoscopy (EGD) and placement of an esophageal Wallflex stent (Boston scientific partially covered 23 mm wide and 125 mm long).
Due to extensive medical history and fairly advanced stage, surgery was contraindicated and the patient was referred for chemotherapy and radiation.
Verrucous carcinomas are a variant of squamous carcinoma. They are slow growing and seen in the oropharynx, larynx, glans penis, scrotum, vulva, vagina, cervix, endometrium, urinary bladder, anorectal region and the sole of the feet[2-4]. The Verrucous carcinomas are believed to be associated with the chronic mucosal irritation or inflammation or a long-term disease process[2,4].
Amongst all different sites for verrucous carcinoma, it is rarely seen in the esophagus[1-9]. First ever case of such cancer in esophagus was reported by Minelly in 1967[2,3,4,7] and thereafter so far less than 30 cases are reported in the English literature[8].
The etiological factors are not clearly delineated in the literature but it seems to be associated with the chronic inflammatory conditions or long term local disease process[1-9]. Risk factors may include smoking; alcohol abuse; hiatal hernia; achalasia; esophagitis; caustic injury from lye, battery or kerosene ingestion; esophageal diverticulum or nutcracker esophagus. In the recent years, few reported cases have shown the association with the HPV virus, although the clear association is very unclear[5,6,8,9]. Our case was not clearly associated with the any of these documented risk factors. Devlin et al[3] mentions that the acid inhibition decreases the tumor length and also changes the appearance from polypoid to sessile and warty. This hypothesizes that the long term acid damage could be a contributory for the development of the verrucous carcinoma.
The incidence rate is higher in male as compared to female with a ratio of approx 2:1[1-3]. An age distribution of this type of carcinoma ranges from 36 to 79 with a mean age of 61[1-3]. Most common presenting sign and symptoms in the verrucous carcinoma of the esophagus are dysphagia and weight loss, seen in our case as well[1-3,5,6]. Other symptoms would be hematemesis, coughing and odynophagia[2,6]. Endoscopic appearance of such lesions includes, shaggy, white, exophytic, wartlike, velvety, papillary, spiked, cauliflower like mass[1-3,7-9]. The tumor is located mostly in the lower esophagus (70%) with no clear reason but it can involve the upper (23%) or the mid part of the esophagus (7%) as well[2-9].
A diagnosis is usually made by either endoscopy guided deep mucosal biopsy or EUS guided tunnel biopsy or post surgery specimen evaluation. Verrucous carcinoma of the esophagus usually evolves in the sequential fashion from acanthosis, hyperkeratosis, parakeratosis, leukoplakia, verrucous lesions, and papillary hyperplasia to verrucous carcinoma[2]. Superficial biopsies of such lesions show only non specific acanthosis, parakeratosis, or hyperkeratosis, with associated acute or chronic inflammation[2,3,6,8]. which makes these types of carcinomas are difficult to diagnose and requires high index of suspicion and repeat endoscopic deep biopsies as in our case (Figure 3). Endoscopic biopsies have revealed 46% cases of the verrucous carcinoma, remaining of them have been diagnosed either after surgery or with the use of EUS[2-9]. EUS is highly accurate imaging modalities for the diagnosis and staging as well as follow up of esophageal tumors. It also estimates the depth of invasion as well as any lymphadenopathy which is helpful in staging. EUS guided tunnel biopsy of such lesions can be useful as seen in few case reports[2-4,8]. A Verrucous carcinoma of the esophagus commonly projects as a diffuse hypoechoic mucosal thickening with varying degree of depth with varying degree of lymphadenopathy in EUS exam[2-4,7,8]. It invades as a column of neoplastic cells in a pushing manner instead of invasion in discreet cells[3], with the 80% invades through and beyond superficial epithelium, 8% limited to the superficial epithelium only and 12% unclear[2-9]. More than 50% cases are found have inflammatory infiltrates surrounding the tumor[3,6], and the lymphnode biopsy mostly shows hyperplastic nodes secondary to local inflammation which can prove that the chronic inflammation predisposes to the verrucous carcinoma of the esophagus[2,7]. Overall, histologically, it is similar to benign squamous papilloma and the tumor infiltration beyond the superficial mucosa fairly differentiates it from the benign squamous cell papilloma[2].
Despite of its slow growth and high degree of differentiation, it has very poor prognosis. As per literature, there is a delay between the onset of the symptoms and the diagnosis. And at the time of the diagnosis, majority of the cases are locally advanced[1-9]. Morbidity and mortality associated with such tumors are mainly due to local invasion or due to surgical complications. There is no any reported case of distant metastasis in the literature. It can spread locally to the lungs, bronchi, pleura and can form fistulas[1,2,8]. Our case is the first reported instance of pericardial invasion confirmed with EUS study. With regards to therapy, early stages of the cancer can be treated surgically with esophageal resection or polypectomy/mucosal resection[1-9]. More advanced cases, or non surgical candidates can be treated with esophageal stent placement, as done in our case. Due to rarity of such tumors, no clear data are available for any effective chemo- radiation therapy. However, most recent post operative follow up case series have shown better prognosis with cancer free survival ranges from 9 mo to 3 years[2,3]. We need a long term follow up with such patients and that can improve the outcome.
A verrucous carcinoma is a slow growing, well differentiated, rare form of squamous carcinoma variant. It is associated with chronic, local disease process and it invades locally. On EGD, it appears as an exophytic irregular warty projecting mass, and it is very difficult to diagnose by superficial biopsy due to non specific superficial histological findings. So it requires high index of suspicion and deep biopsy with EGD or EUS. It projects as hypoechoic mucosal thickening on EUS. Early stages of cancers are treated surgically. Advanced cases can be referred for esophageal stent placement for palliation and chemo radiation. It has high morbidity and mortality and requires long term follow up for accurate numbers regarding to the treatment and the follow up.
A 78-year-old African American man presented with dysphagia, weight loss of 15 Lbs over 4-5 wk and right lower quadrant dull, and non radiating abdominal pain.
Physical examination was unremarkable.
Benign squamous papilloma, adenocarcinoma of the esophagus
BUN and serum creatinine were 42 and 2.4 respectively, normal liver function tests; Hemoglobin was 12.4 with MCV 84.4.
A barium esophagogram showed a long, irregular stricture involving the mid and distal esophagus with an apparent intraluminal mass at its proximal end. A computed tomography scan of the chest showed some mediastinal lymph nodes. Bone scan showed no any bone metastasis.
The endoscopic examination and extensive biopsies with jumbo forceps revealed the diagnosis of verrucous carcinoma of the esophagus. In situ hybridization for both high and low risk HPV was negative.
Due to extensive medical history and fairly advanced stage, surgery was contraindicated and the patient Patient underwent EGD and placement of an esophageal Wallflex stent and was referred to chemotherapy and radiation.
The etiological factors are not clearly delineated in the literature. It has high morbidity and mortality and requires long term follow up for accurate numbers regarding to the treatment and the follow up.
This report presents a case of rare variant of squamous cell cancer of esophagus, and difficulties associated with the diagnosis and treatment. It is very beneficial for the patients, if it is diagnosed in the early stages. But nonspecific superficial biopsies make it difficult to diagnose and it requires high index of suspicion even without any associated risk factors.
It is indeed a rare form of squamous cell carcinoma. Due to the same reasons, there are not enough studies available in terms of management that can be applied to general population.
P- Reviewers: Eslick GD, Gimeno-Garcia AZ, Natsugoe S S- Editor: Qi Y L- Editor: A E- Editor: Wu HL
| 1. | Malik AB, Bidani JA, Rich HG, McCully KS. Long-term survival in a patient with verrucous carcinoma of the esophagus. Am J Gastroenterol. 1996;91:1031-1033. [PubMed] [Cited in This Article: ] |
| 2. | Osborn NK, Keate RF, Trastek VF, Nguyen CC. Verrucous carcinoma of the esophagus: clinicopathophysiologic features and treatment of a rare entity. Dig Dis Sci. 2003;48:465-474. [PubMed] [Cited in This Article: ] |
| 3. | Devlin S, Falck V, Urbanski SJ, Mitchell P, Romagnuolo J. Verrucous carcinoma of the esophagus eluding multiple sets of endoscopic biopsies and endoscopic ultrasound: a case report and review of the literature. Can J Gastroenterol. 2004;18:459-462. [PubMed] [Cited in This Article: ] |
| 4. | Na S, Choi KD, Yoo C, Chang Y, Song HJ, Lee GH, Jung HY, Cho KJ, Kim JH. Verrucous carcinoma of the esophagus. Gastrointest Endosc. 2009;70:803-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Tonna J, Palefsky JM, Rabban J, Campos GM, Theodore P, Ladabaum U. Esophageal verrucous carcinoma arising from hyperkeratotic plaques associated with human papilloma virus type 51. Dis Esophagus. 2010;23:E17-E20. [PubMed] [Cited in This Article: ] |
| 6. | Macias-Garcia F, Martinez-Lesquereux L, Fernandez B, Parada P, Larino-Noia J, Sobrino-Faya M, Iglesias-Canle J, Iglesias-Garcia J, Forteza J, Dominguez-Munoz JE. Verrucous carcinoma of the esophagus: a complex diagnosis. Endoscopy. 2010;42 Suppl 2:E137-E138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Chu Q, Jaganmohan S, Kelly B, Hobley J. Verrucous carcinoma of the esophagus: a rare variant of squamous cell carcinoma for which a preoperative diagnosis can be a difficult one to make. J La State Med Soc. 2011;163:251-253. [PubMed] [Cited in This Article: ] |
| 8. | Feinstein AR. The unit fragility index: an additional appraisal of “statistical significance” for a contrast of two proportions. J Clin Epidemiol. 1990;43:201-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Liberale G, De Simone P, Snoeck R, Féron P, Gelin M, El Nakadi I. Verrucous carcinoma of the esophagus. A case report. Minerva Chir. 2005;60:61-65. [PubMed] [Cited in This Article: ] |