Published online Jun 26, 2015. doi: 10.5662/wjm.v5.i2.26
Peer-review started: March 2, 2015
First decision: April 27, 2015
Revised: May 17, 2015
Accepted: June 1, 2015
Article in press: June 2, 2015
Published online: June 26, 2015
Processing time: 129 Days and 3.2 Hours
Seventy-five percent of upper limb disorders that are related to work are regarded as diagnostically unclassifiable and therefore challenging to the clinician. Therefore it has been generally less successfully to prevent and treat these common and frequently disabling disorders. To reach a diagnosis requires the identification of the responsible pathology and the involved tissues and structures. Consequently, improved diagnostic approaches are needed. This editorial discusses the potentials of using the clinical neurologic examination in patients with upper limb complaints related to work. It is argued that a simple but systematic physical approach permits the examiner to frequently identify patterns of neurological findings that suggest nerve afflictions and their locations, and that electrophysiological studies are less likely to identify pathology. A diagnostic algorithm for the physical assessment is provided to assist the clinician. Failure to include representative neurological items in the physical examination may result in patients being misinterpreted, misdiagnosed and mistreated.
Core tip: Patients with work-related upper limb disorders should be subjected to a systematic upper limb examination including neurological items with the main focus on muscle strength testing. A refined version of the classical neurological upper limb examination can be rewarding because it permits the clinician to frequently identify patterns in accordance with nerve afflictions with specific locations. This examination is suitable in any clinical setting because it is simple, inexpensive, noninvasive, and highly reproducible.
- Citation: Jepsen JR. Clinical neurological examination vs electrophysiological studies: Reflections from experiences in occupational medicine. World J Methodol 2015; 5(2): 26-30
- URL: https://www.wjgnet.com/2222-0682/full/v5/i2/26.htm
- DOI: https://dx.doi.org/10.5662/wjm.v5.i2.26
An estimated three quarters of upper limb disorders that are related to work are regarded as diagnostically unclassifiable[1] and consequently these conditions remain a diagnostic challenge to the physician. Therefore evidence-based prevention and treatment have been largely unsuccessful. To reach a diagnosis requires the identification of the tissues and specific structures that are involved, and also of the pathology that causes the condition. To achieve this goal, improved diagnostic approaches to these frequent and disabling conditions should be applied.
Frequently, patients with work-related upper limb disorders have pain with characteristics that suggest that the pain is neuropathic. The pain may be accompanied by sensory abnormalities such as paraesthesia, subjective weakness or heaviness and/or tactile dysfunction. The combination of a neuropathic pain with motor and sensory symptoms suggests that the nervous system is involved and therefore that the upper limb peripheral nerves should be included in the physical examination. Still, clinicians and also researchers tend to ignore this possibility and to rather attribute these conditions to pathology located in muscles, tendons or insertions. Even if involvement of peripheral nerve(s) is considered, the attention tends to be directed - and limited - to carpal tunnel syndrome and afflictions of a cervical root. The intermediate portion of nerve of a length approaching one meter, and other potential locations of focal neuropathies receive less attention.
Focal neuropathies cause rather specific neurological patterns: If muscles are innervated distally to a nerve-lesion they are likely to be weak; the sensibility in supplied cutaneous territories will be altered; there will be abnormal soreness where the nerve trunk is affected. The classical neurological examination is based on these principles and all physicians have been trained in its execution. Still, there seems to be reluctance to perform a detailed neurological examination in upper limb patients with work-related complaints. This is particularly the case with respect to the portions of the upper limb nerves that are located proximally such as in the forearm, arm and shoulder. To the experience of the author this inadequacy applies to physicians in any specialty including neurology. Performing a detailed clinical neurological examination and to interpret its outcome may be regarded as difficult, and this examination may also be assumed to be time consuming. It is true that relevant benefit of the examination requires knowledge of anatomy such as the location of nerves and their innervation patterns. This has been previously learned but might be forgotten. To achieve a neurological diagnosis such as the identification of a focal nerve affliction of the upper limb, the neurological examination may also be perceived as less rewarding than paraclinical studies. Although this view is not justified physical neurological upper limb examinations are rarely more than basic. Rather than performing a detailed examination it may be easier for the clinician to refer the patient to electrophysiological examination (and frequently to MR-imaging - in particular of the cervical spine) and so to leave the diagnostic work to others.
This choice may be justified if electrophysiological studies of the upper limb nerves reflect the truth better than the traditional neurological examination. Clinicians - including many neurologists - tend to view electrophysiological (and imaging) studies as superior to their own physical examination and judgement. Consequently, the outcome of a physical examination based on patterns of neurological abnormalities suggesting focal peripheral neuropathy is likely to be regarded as less valid if electrophysiological studies do not identify abnormalities. However, according to the scientific literature, the superiority of electrophysiology has not been demonstrated and certainly not for disorders of the upper limb studied in an occupational context. While electrophysiological studies tend to be generally viewed as “golden standard” for peripheral neuropathy their sensitivity - in particular with minor nerve afflictions such as may be the case with work-related upper limb complaints - is limited because nerve lesions may be mixed and partial with few myelinated fibres intact and reinnervation taking place. Therefore the electrophysiological findings may be entirely normal[2]. The potentials of a refined electrophysiological assessment are acknowledged but the application of expanded techniques is also very time consuming and consequently expensive, and therefore rarely applied. There is also agreement that a detailed neurological physical examination should precede an electrophysiological study of the peripheral nerves and guide its content. Evidently, it has no sense to study electrophysiologically the median nerve in the carpal tunnel when a nerve affliction is located elsewhere. Some common locations of upper limb nerve entrapment can only rarely be identified by electrophysiological studies, e.g., radial tunnel syndrome[3], pronator syndrome[4] and brachial plexopathy[5].
It is essential that the physical examination focuses on all nerves of relevance and on the entire length of nerves from the roots to their muscular and cutaneous supply. That means that the examiner should include neurological items that are representative to nerve afflictions with any location that one would expect. The physical neurological examination should be reliable and also valid, meaning that it should be capable to identify abnormalities in symptomatic limbs and exclude abnormalities in healthy limbs, respectively.
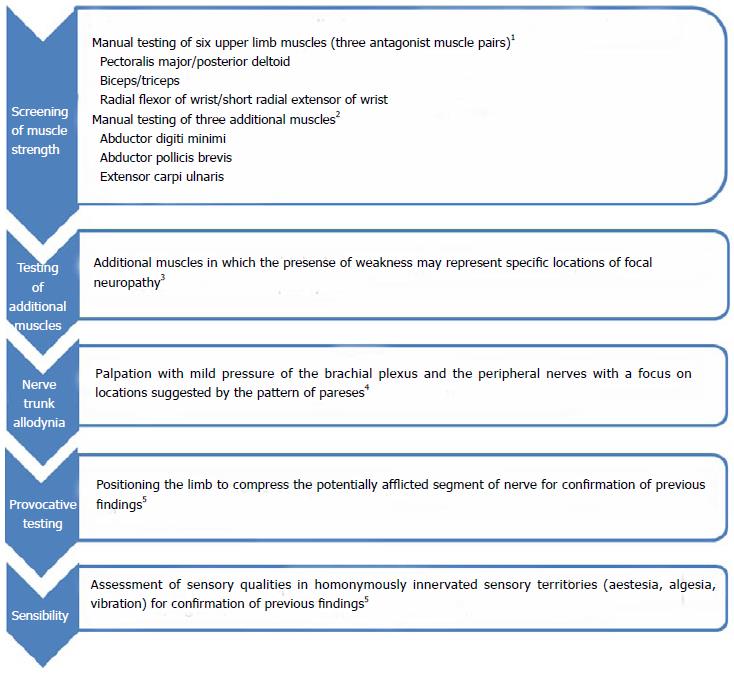
A semiquantitative detailed upper limb neurological examination, which has been developed for this purpose consists of manual strength-testing in selected individual and representative muscles[6]. It also contains of an assessment of sensory deviations from normal in representative territories, which are homonymously innervated. Finally, the presence of allodynia of nerve trunks with mild palpation should be studied at the location(s) where nerves may be affected[7]. This low-tech examination is rapid to perform and requires no equipment beside a needle and a 256 Hz tuning fork.
When this examination was carried out on patients that were referred for assessment in a hospital department of occupational medicine there was a high occurrence of patterns of neurological findings. These patterns were in accordance with the topography of the nerves and their muscular and sensory innervation – and they were also frequently demonstrated in upper limb patients that could not be diagnosed by conventional means. The construct validity of this approach in terms of interrelations of nerve afflictions with various location has previously been demonstrated[8]. There was a high inter-rater reliability of the identification of neurological patterns[7]. The validity of this approach was further indicated by demonstrating that the presence of neurological patterns was related to the presence of symptoms[9]. The most frequent location of nerve afflictions in the upper limb was at the infraclavicular brachial plexus (behind the minor pectoral muscle below the clavicle). This location of nerve affliction was often found in combination with median neuropathy (just proximally to and medially to the elbow joint) and radial (posterior interosseous) neuropathy (at the Arcade of Frohse) at elbow level. Whether diagnosed by criteria that included a thorough neurological examination or by conventional diagnostic criteria, neuropathic upper limb conditions could also be identified as the most frequent among patients in general practice[10].
It is frequently frustrating to experience when a patient with peripheral upper limb nerve affliction(s) with certain location(s) diagnosed by this examination is subsequently examined by a neurologist. After a mostly limited neurological examination and an electrophysiological study targeting a few selected parameters, the neurologist is likely to conclude the absence of a neurological condition and to interpret the patient’s complaints and findings (e.g., “pain induced weakness” or “sensory deviation with a non-dermatomal extension”) as either due to a disorder located to muscles or to be functional and without any somatic origin. These patients are likely to be misinterpreted, misdiagnosed and mistreated. Furthermore, the legal authorities seem to trust the basic examination by the neurologist rather than to appreciate a detailed neurological examination.
I regard the assessment of individual muscle strength as the most important part of the clinical neurological tests. I would therefore suggest clinicians who see upper limb patients to routinely integrate in their physical examination a screening approach consisting of manual muscle testing of six to nine representative upper limb muscles (Figure 1). This approach is sensitive and permits the identification of patients that should be physically examined further to determine the location of an upper limb nerve affliction[11]. Any physician can easily learn to manually assess the strength in individual muscles[6,11]. This part of the examination is therefore feasible in any clinical setting whether it be in industrialized countries or in the developing world.
A correct diagnosis is essential for targeted preventive intervention at workplaces as well as for treatment, which may follow the concepts of neuromobilisation[13-15]. There is increasing evidence of an effect of nerve mobilisation in the treatment of upper limb nerve afflictions[14]. Neurolytic surgery for upper limb nerve afflictions has been undertaken for years but its success depends of a precise location of the affliction.
Including a systematic neurologic examination in the diagnostic physical approach to patients with work-related upper limb disorders may eventually constitute a step towards improved prevention but this remains to be demonstrated. The first step would be to demonstrate risk factors in work as has been done for certain neuropathic upper limb conditions such as, e.g., radial tunnel syndrome[16] and brachial plexopathy[17]. Next would be to see whether the removal or reduction of these risk factors would reduce the occurrence.
I would caution against blind faith in diagnostic tools such as electrophysiological studies. As demonstrated by others, it is not automatically the best or safest choice to trust device outputs that have a potential for flawed measurement. Trained judgement should be applied when interpreting results generated from devises[18] such as results from electrophysiological studies. The clinician should know their potentials and limitations, and be able to assess whether they are better or inferior than the clinical examination.
P- Reviewer: Hamill OP, Trohman R S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Palmer K, Cooper C. Repeated movement and repeated trauma affecting the musculoskeletal disorders of the upper limbs. Hunter’s Diseases of Occupations. 9th ed. London: Arnold 2000; 453-475. |
| 2. | Krarup C. Pitfalls in electrodiagnosis. J Neurol. 1999;246:1115-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Werner CO. Lateral elbow pain and posterior interosseous nerve entrapment. Acta Orthop Scand Suppl. 1979;174:1-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 83] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Werner CO, Rosén I, Thorngren KG. Clinical and neurophysiologic characteristics of the pronator syndrome. Clin Orthop Relat Res. 1985;231-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Aminoff MJ, Olney RK, Parry GJ, Raskin NH. Relative utility of different electrophysiologic techniques in the evaluation of brachial plexopathies. Neurology. 1988;38:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Jepsen J, Laursen L, Larsen A, Hagert CG. Manual strength testing in 14 upper limb muscles: a study of inter-rater reliability. Acta Orthop Scand. 2004;75:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Jepsen JR, Laursen LH, Hagert CG, Kreiner S, Larsen AI. Diagnostic accuracy of the neurological upper limb examination I: inter-rater reproducibility of selected findings and patterns. BMC Neurol. 2006;6:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Jepsen JR, Laursen LH, Kreiner S, Larsen AI. Neurological examination of the upper limb: a study of construct validity. Open Neurol J. 2009;3:54-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Jepsen JR, Laursen LH, Hagert CG, Kreiner S, Larsen AI. Diagnostic accuracy of the neurological upper limb examination II: relation to symptoms of patterns of findings. BMC Neurol. 2006;6:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Laursen LH, Sjøgaard G, Hagert CG, Jepsen JR. Diagnostic distribution of non-traumatic upper limb disorders: vibrotactile sense in the evaluation of structured examination for optimal diagnostic criteria. Med Lav. 2007;98:127-144. [PubMed] |
| 11. | Jepsen JR. Can testing of six individual muscles represent a screening approach to upper limb neuropathic conditions? BMC Neurol. 2014;14:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Jepsen JR, Hagert CG. Muscle testing in the diagnosis of work-related upper limb complaints. Europ Neurol J. 2010;2:1-9. |
| 13. | Schmid AB, Nee RJ, Coppieters MW. Reappraising entrapment neuropathies--mechanisms, diagnosis and management. Man Ther. 2013;18:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Butler DS. Mobilisation of the nervous system. Melbourne: Churchill Livingstone 1992; . |
| 15. | Butler DS. The sensitive nervous system. Adelaide: Noigroup Publications 2000; . |
| 16. | Roquelaure Y, Raimbeau G, Dano C, Martin YH, Pelier-Cady MC, Mechali S, Benetti F, Mariel J, Fanello S, Penneau-Fontbonne D. Occupational risk factors for radial tunnel syndrome in industrial workers. Scand J Work Environ Health. 2000;26:507-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Jepsen JR. Brachial plexopathy: a case-control study of the relation to physical exposures at work. J Occup Med Toxicol. 2015;10:14. [PubMed] |
| 18. | Trohman RG. Trust in technology: straddling the line between faith and reason. Crit Care Med. 2010;38:712-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |