Copyright
©The Author(s) 2023.
World J Methodol. Jun 20, 2023; 13(3): 67-78
Published online Jun 20, 2023. doi: 10.5662/wjm.v13.i3.67
Published online Jun 20, 2023. doi: 10.5662/wjm.v13.i3.67
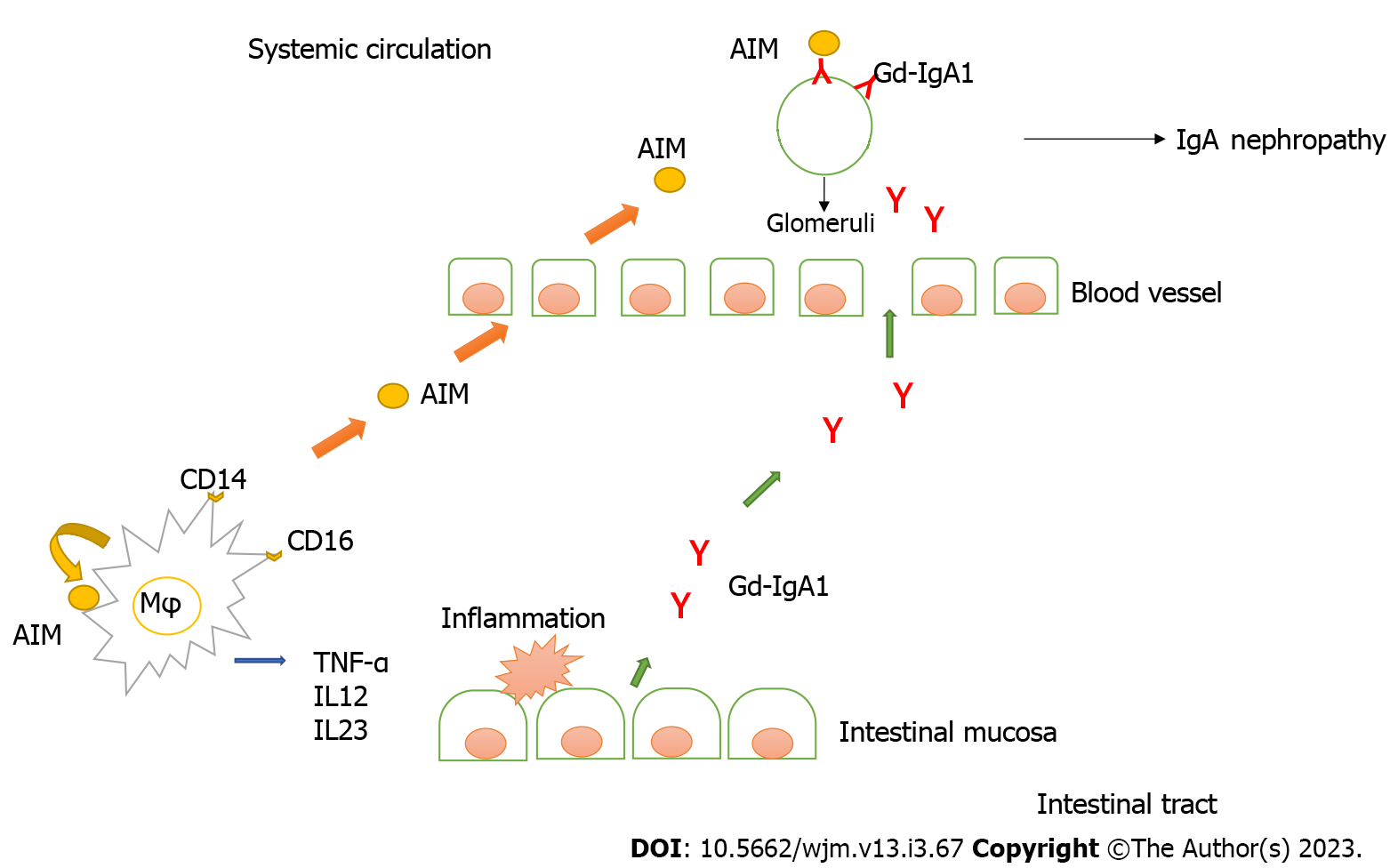
Figure 1 Intestinal mucosal barrier disruption due to Crohn’s disease enhances the production of glycosylated IgA.
Apoptosis inhibitor of macrophages (AIM) produced by resident macrophages in the intestinal tissue contributes to intestinal inflammation, and active macrophage-derived AIM in the gut leads to elevated serum AIM levels. AIM is involved in the recruitment of inflammatory macrophages via autocrine and paracrine and induces inflammatory cytokine (TNF-α) in mesenteric adipose tissue in Crohn’s disease. AIM influences the pathogenesis of Crohn’s disease by inhibiting apoptosis of active intestinal macrophages and enhancing the expression of TNF-α in these mesenteric adipose tissues. Intestinal mucosal barrier disruption due to Crohn’s disease enhances the production of glycosylated IgA. In IgA nephropathy, it was clarified that the deposition of IgA in the glomerulus is essential as the first step, and that AIM leads to inflammation as the second step. AIM: Apoptosis inhibitor of macrophages; CD: Crohn's disease; Mφ: Macrophages.
Figure 2 Clinical course after the appearance of hematuria.
Hematuria and proteinuria persisted, and IgA nephropathy was suspected. Since there were some reports of IgA nephropathy caused by infliximab, we switched from infliximab to vedolizumab. After the change to vedolizumab, Crohn’s disease worsened, and there was a marked increase in proteinuria. Fever and abdominal symptoms worsened, and infliximab was administered again. Thereafter, Crohn’s disease improved rapidly, and decrease in the urinary protein level was noted. OB: Occult blood urine; U-TP/Cre: Urinary protein creatinine ratio; PCDAI: Pediatric Crohn’s disease activity index; y: years; m: Months.
- Citation: Tamura H. IgA nephropathy associated with Crohn's disease. World J Methodol 2023; 13(3): 67-78
- URL: https://www.wjgnet.com/2222-0682/full/v13/i3/67.htm
- DOI: https://dx.doi.org/10.5662/wjm.v13.i3.67