Published online Mar 19, 2024. doi: 10.5498/wjp.v14.i3.409
Peer-review started: November 30, 2023
First decision: December 18, 2023
Revised: December 30, 2023
Accepted: January 23, 2024
Article in press: January 18, 2024
Published online: March 19, 2024
Dysphoria and despondency are prevalent psychological issues in patients undergoing Maintenance Hemodialysis (MHD) that significantly affect their quality of life (QOL). High levels of social support can significantly improve the physical and mental well-being of patients undergoing MHD. Currently, there is limited research on how social support mediates the relationship between dysphoria, despondency, and overall QOL in patients undergoing MHD. It is imperative to investigate this mediating effect to mitigate dysphoria and despondency in patients undergoing MHD, ultimately enhancing their overall QOL.
To investigate the mediating role of social support in relationships between dysphoria, despondency, and QOL among patients undergoing MHD.
Participants comprised 289 patients undergoing MHD, who were selected using a random sampling approach. The Social Support Rating Scale, Self-Rating Anxiety Scale, Self-Rating Depression Scale, and QOL Scale were administered. Correlation analysis was performed to examine the associations between social support, dysphoria, despondency, and QOL in patients undergoing MHD. To assess the mediating impact of social support on dysphoria, despondency, and QOL in patients undergoing MHD, a bootstrap method was applied.
Significant correlations among social support, dysphoria, despondency, and quality in patients undergoing MHD were observed (all P < 0.01). Dysphoria and despondency negatively correlated with social support and QOL (P < 0.01). Dysphoria and despondency had negative predictive impacts on the QOL of patients undergoing MHD (P < 0.05). The direct effect of dysphoria on QOL was statistically significant (P < 0.05). Social support mediated the relationship between dysphoria and QOL, and this mediating effect was significant (P < 0.05). Similarly, the direct effect of despondency on QOL was significant (P < 0.05). Moreover, social support played a mediating role between despondency and QOL, with a significant mediating effect (P < 0.05).
These findings suggest that social support plays a significant mediating role in the relationship between dysphoria, despondency, and QOL in patients undergoing MHD.
Core Tip: Dysphoria and despondency are prevalent negative emotional experiences in patients undergoing maintenance hemodialysis (MHD), significantly affecting both prognosis and overall quality of life (QOL). Enhancing social support can improve the QOL of patients undergoing MHD. This study surveyed 289 patients undergoing MHD using questionnaires to examine the mediating role of social support in the relationship between dysphoria, despondency, and QOL. The findings contribute to the development of a theoretical foundation for psychological interventions in patients undergoing MHD, ultimately aiming to effectively alleviate dysphoria and despondency and subsequently enhance their overall QOL.
- Citation: Zhou X, Jiang H, Zhou YP, Wang XY, Ren HY, Tian XF, Zhang QQ. Mediating role of social support in dysphoria, despondency, and quality of life in patients undergoing maintenance hemodialysis. World J Psychiatry 2024; 14(3): 409-420
- URL: https://www.wjgnet.com/2220-3206/full/v14/i3/409.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i3.409
Maintenance Hemodialysis (MHD) is an enduring and often lifelong therapy for patients with end-stage kidney disease. This treatment is known for its lengthy and demanding process, which frequently results in a range of psychological challenges for patients[1]. Numerous studies have demonstrated a high prevalence of psychological disorders in patients undergoing MHD, with dysphoria and despondency being particularly prevalent[2]. These psychological issues have a significant impact on the physical and mental well-being of patients and can diminish their sense of hope for survival. Social support refers to the emotional and material assistance individuals receive from their social relationships, including family members, friends, significant others, and various organizations[3]. Strong social support has been shown to positively affect a patient’s quality of life (QOL). Research has consistently revealed negative associations among social support, dysphoria, and despondency, highlighting the role of social support in reducing the risk of these psychological problems[4,5]. Additionally, social support is positively correlated with QOL, with improved social support leading to enhanced QOL[6]. Despite the existing body of research on dysphoria, despondency, social support, and QOL in patients undergoing MHD[7-10], few studies have investigated the underlying mechanisms through which social support influences dysphoria, despondency, and QOL in these patients. This study aimed to explore the intricate relationships between social support and dysphoria, despondency, and QOL in patients undergoing MHD. Furthermore, this study aimed to investigate the mediating role of social support in the relationship between dysphoria, despondency, and QOL among these patients. The ultimate goal of this study was to provide a theoretical foundation for clinical healthcare professionals to deliver targeted treatments and comprehensive care for individuals undergoing MHD.
Between January and December 2022, a random sampling method was employed to select patients undergoing MHD from the hemodialysis center of the People’s Hospital of Xinjiang Uygur Autonomous Region for participation in a questionnaire survey. The demographic information of patients is shown in Table 1. All patients included in this study were of biological sex. Inclusion criteria were as follows: (1) Age ≥ 18 years; (2) undergoing regular hemodialysis for a minimum of three months; (3) conscious and free from communication disorders; and (4) willing to participate in the survey. Exclusion criteria included: (1) The presence of a mental disorder or cognitive impairment; (2) experiencing acute infections, acute heart failure, or other severe organ dysfunction; and (3) inability to complete the questionnaire.
| Variables | Categories | Number, n (%) |
| Sex | Male | 158 (54.67) |
| Female | 131 (45.33) | |
| Age | < 45 yr | 39 (13.50) |
| 45-60 yr | 128 (44.29) | |
| > 60 yr | 122 (42.21) | |
| Education | Below high school | 164 (56.75) |
| High school and above | 125 (43.25) | |
| Marital status | Married | 242 (83.74) |
| Single (unmarried, divorced, widowed) | 47 (16.26) | |
| Monthly income | < 3000 yuan | 55 (19.03) |
| 3000-5000 yuan | 129 (44.64) | |
| > 5000 yuan | 105 (36.33) | |
| Medical insurance status | Medical insurance/social insurance | 212 (73.36) |
| Self-payment | 77 (26.64) |
Social support rating scale: The Social support rating scale version developed by Xiao et al[11] was utilized in this study. This scale comprises ten items categorized into three dimensions: Subjective support (items 1, 3-5), objective support (items 2, 6-7), and the utilization of social support (items 8-10). Items 1-4 and 8-10 were single-choice questions. A 4-point Likert scoring method was employed, with items 1-4 scored individually. Item 5 offered five options (A-E). Each option was assigned a score from 1 to 4 (“none” = 1 point, “very little” = 2 points, “general” = 3 points, and “full support” = 4 points). For items 6-7, selecting “no source” was scored as 0, while choosing “the following sources” resulted in points being calculated based on the number of sources selected. The scores for the 10 items were summed to calculate the scale’s total score, which ranged from 12 to 66. These scores were divided into three levels: A total score of ≤ 22 indicated a low level of support, a total score of 23-44 denoted a medium level of support, and a total score of 45-66 signified a high level of support. A higher score indicated greater availability of social support. The Cronbach’s α coefficient for this scale was 0.808.
Self-rating anxiety scale: The dysphoria scale developed by Zhang et al[12] was used in this study. The scale consisted of 20 items scored on a 4-point scale. The total raw score was calculated by adding the scores of the 20 Self-rating anxiety scale (SAS) items. The integer part of this total score, when multiplied by 1.25, yielded the standard score. A cut-off value of 50 points was used to assess dysphoria, with scores below 50 indicating the absence of dysphoria, scores between 50-59 indicating mild dysphoria, scores between 60-69 indicating moderate dysphoria, and scores equal to or greater than 70 indicating severe dysphoria. The Cronbach’s α coefficient for this scale was 0.855.
Self-rating depression scale: The 2-item despondency scale developed by Xu et al[13] was used. Each item was scored on a 4-point scale. The total raw score was calculated by summing the scores of the 20 Self-rating depression scale (SDS) items, and the integer part of this total score, when multiplied by 1.25, yielded the standard score. A cutoff value of 53 was used to assess despondency, with scores less than 53 indicating the absence of despondency, scores between 53-62 indicating mild despondency, scores between 63-72 indicating moderate despondency, and scores greater than 72 indicating severe despondency. The Cronbach’s α coefficient for this scale was 0.8.
QOL scale (SF-36): The SF-36 scale, developed by the Boston Health Research Institute and the Chinese version by Zhejiang University[14], was used. This scale consisted of 36 items distributed across 8 dimensions: Physical Functioning (PF), Role Physical (RP), Bodily Pain (BP), General Health (GH), Vitality (VT), Social Functioning (SF), Role Emotional (RE), and Mental Health (MH). The original scores for each dimension were computed using the summated rating method and converted into a hundred-mark system (0-100)[15]. QOL was assessed based on the overall scores of the physical component summary (PCS) and mental component summary (MCS), with scores for both domains converted into hundred-mark scores[16]. The overall PCS and MCS scores were calculated based on the scores from each dimension: PCS = PF + RP + BP + GH and MCS = VT + SF + RE + MH. The Cronbach’s α coefficient for this scale was 0.869.
A questionnaire survey was conducted to collect the data. Before the survey, approval was obtained from the relevant hospital authorities, and the research’s purpose, significance, and ethical aspects were explained to the participants. Informed consent was obtained from all the participants. The distribution and collection of questionnaires were managed by the research investigators. A consistent set of instructions was used in the survey questionnaire to ensure uniformity in the data collection process. Upon completion of the questionnaires, the participants were collected onsite to ensure the responses’ authenticity, validity, and completeness. In total, 300 questionnaires were distributed, with 289 valid questionnaires successfully collected, for a recovery rate of 96.33%.
SPSS statistical software (version 26.0) was used for data analysis, and the significance level was set at P < 0.05. The scores obtained from each scale were described using the interquartile range, and the count data were presented as n (%). Nonparametric and correlation tests were used to analyze the data. The mediating effect was assessed using PROCES.
The total social support scores obtained from the 289 patients undergoing MHD ranged from 13 to 60, indicating a moderate overall level of support. Of the participants, 63 (20.80%) were categorized as having a low level of support, 128 (44.29%) as having a medium level of support, and 98 (33.91%) as having a high level of support (Table 2). Based on the different levels of social support, patients undergoing MHD were grouped into three categories: Low, medium, and high levels of support. Subsequently, the levels of dysphoria, despondency, and QOL were analyzed for each group.
| Items | Number, n (%) | Score range (points) | Score (points) |
| Subjective support | 289 (100.00) | 8-32 | 19 (12, 26) |
| Objective support | 289 (100.00) | 1-22 | 9 (5, 16) |
| The utilization of social support | 289 (100.00) | 3-12 | 7 (5, 10) |
| Total score | 289 (100.00) | 13-60 | 39 (24.5, 46) |
| Low level of support | 63 (20.80) | 14-22 | 20 (18, 21) |
| High levels of support | 128 (44.29) | 23-44 | 37 (30, 41) |
| High levels of support | 98 (33.91) | 45-60 | 49 (46, 53) |
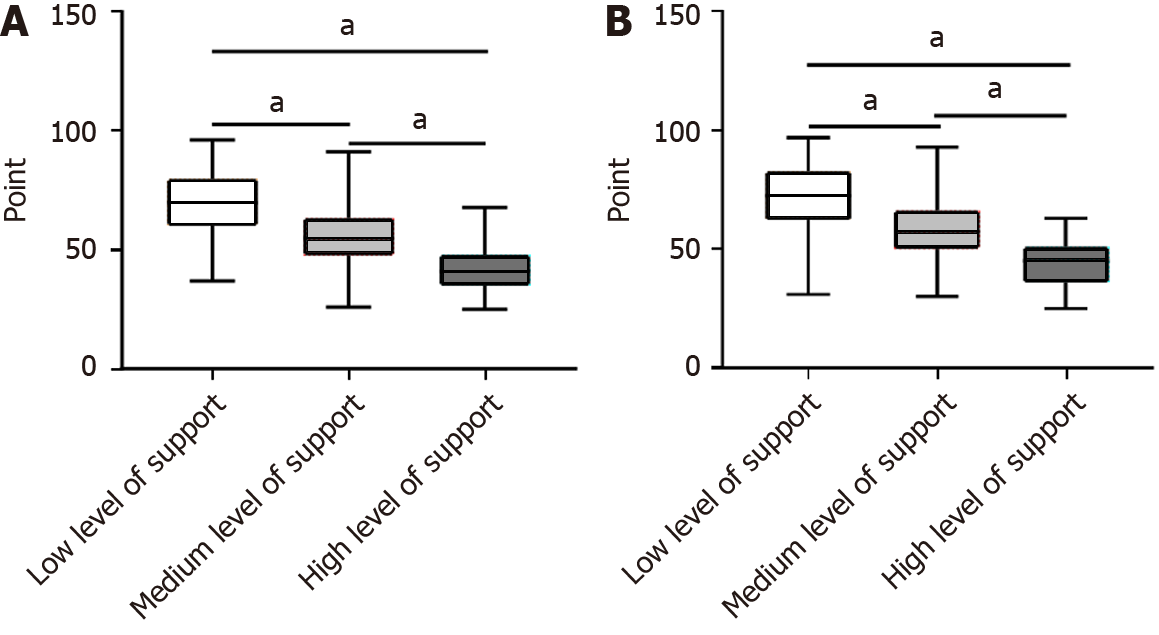
The SAS scores of the 289 patients undergoing MHD had a score of 52 (42, 65), indicating an overall level of mild dysphoria. Among them, 115 (39.79 %) patients did not exhibit dysphoria, 73 (25.26%) had mild dysphoria, 54 (18.69%) had moderate dysphoria, and 47 (16.26%) had severe dysphoria (Table 3). Significant differences were observed in the SAS scores among the low, medium, and high levels of support (P < 0.05). Additionally, significant differences were noted in pairwise comparisons among the low, medium, and high support levels (P < 0.05; Figure 1A).
| Number, n (%) | Score (points) | |
| Standard score | 289 (100.00) | 52 (42, 65) |
| No dysphoria | 115 (39.79) | 41 (35, 43) |
| Mild dysphoria | 73 (25.26) | 53 (51, 56) |
| Moderate dysphoria | 54 (18.69) | 65 (62, 66) |
| Severe dysphoria | 47 (16.26) | 77 (74, 86) |
The median SDS score of the 289 patients had a score of 55 (45, 67), indicating an overall level of mild despondency. Among them, 132 (45.67%) did not experience despondency, 63 (21.80%) had mild despondency, 44 (15.23%) had moderate despondency, and 50 (17.30%) experienced severe despondency (Table 4). Significant differences were observed in the SDS scores between the low, medium, and high support levels (P < 0.05). Additionally, significant differences were noted in pairwise comparisons among the low, medium, and high support levels (P < 0.05; Figure 1B).
| Number, n (%) | Score (points) | |
| Standard score | 289 (100.00) | 55 (45, 67) |
| No despondency | 132 (45.67) | 43 (37, 48) |
| Mild despondency | 63 (21.80) | 57 (56, 61) |
| Moderate despondency | 44 (15.23) | 67 (64, 70.5) |
| Severe despondency | 50 (17.30) | 81 (77, 87) |
Among the 289 patients undergoing MHD, the QOL (PCS) score had a value of 105.11 (80.70, 126.64). Similarly, the QOL (MCS) score had a value of 111.64 (84.74, 130.18; Table 5). Significant differences were noted in the scores of all eight dimensions as well as in QOL (PCS) and QOL (MCS) among the low, medium, and high levels of support (P < 0.05). Moreover, significant differences were observed in pairwise comparisons among the low, medium, and high support levels (P < 0.05; Table 6).
| Score (points) | |
| PF | 55 (25, 80) |
| RP | 50 (25, 75) |
| BP | 62.5 (46, 87.5) |
| GH | 62 (40, 82) |
| VT | 60 (40, 80) |
| SF | 64 (44, 84) |
| RE | 66.67 (44.44, 88.89) |
| MH | 66.67 (0, 100) |
| Quality of life (PCS) | 105.11 (80.70, 126.64) |
| Quality of life (MCS) | 111.64 (84.74, 130.18) |
| Low level of support | Medium level of support | High level of support | H | P value | |
| Physical functioning | 10 (5, 20) | 50 (30, 70) | 85 (73.75, 91.25) | 169.696 | < 0.001 |
| Role physical | 0 (0, 25) | 50 (25, 75) | 75 (75, 100) | 135.561 | < 0.001 |
| Bodily pain | 49.5 (33.5, 58.5) | 58.5 (37.5, 69.5) | 94 (81.5, 100) | 109.892 | < 0.001 |
| General health | 25 (20, 35) | 57 (45, 67) | 87 (75, 92) | 180.510 | < 0.001 |
| Vitality | 30 (20, 40) | 57.5 (46.25, 70) | 85 (73.75, 91.25) | 164.913 | < 0.001 |
| Mental health | 32 (20, 40) | 64 (52, 76) | 92 (76, 96) | 170.850 | < 0.001 |
| Social functioning | 22.22 (11.11, 22.22) | 55.56 (44.44, 75) | 88.89 (77.785, 100) | 173.945 | < 0.001 |
| Role emotional | 0 (0, 33.33) | 66.67 (0, 100) | 66.67 (66.67, 100) | 57.644 | < 0.001 |
| Quality of life (PCS) | 73.17 (60.73, 73.17) | 99.04 (83.29, 113.28) | 129.76 (121.32, 140.17) | 177.620 | < 0.001 |
| Quality of life (MCS) | 73.72 (64.62, 87.28) | 106.86 (88.02, 127.40) | 129.16 (116, 138.81) | 115.293 | < 0.001 |
Social support was positively correlated with both QOL (PCS and MCS) (P < 0.01). Dysphoria showed a positive correlation with despondency (P < 0.01). Dysphoria and despondency were negatively correlated with QOL (PCS and MCS) and social support (P < 0.01; Table 7).
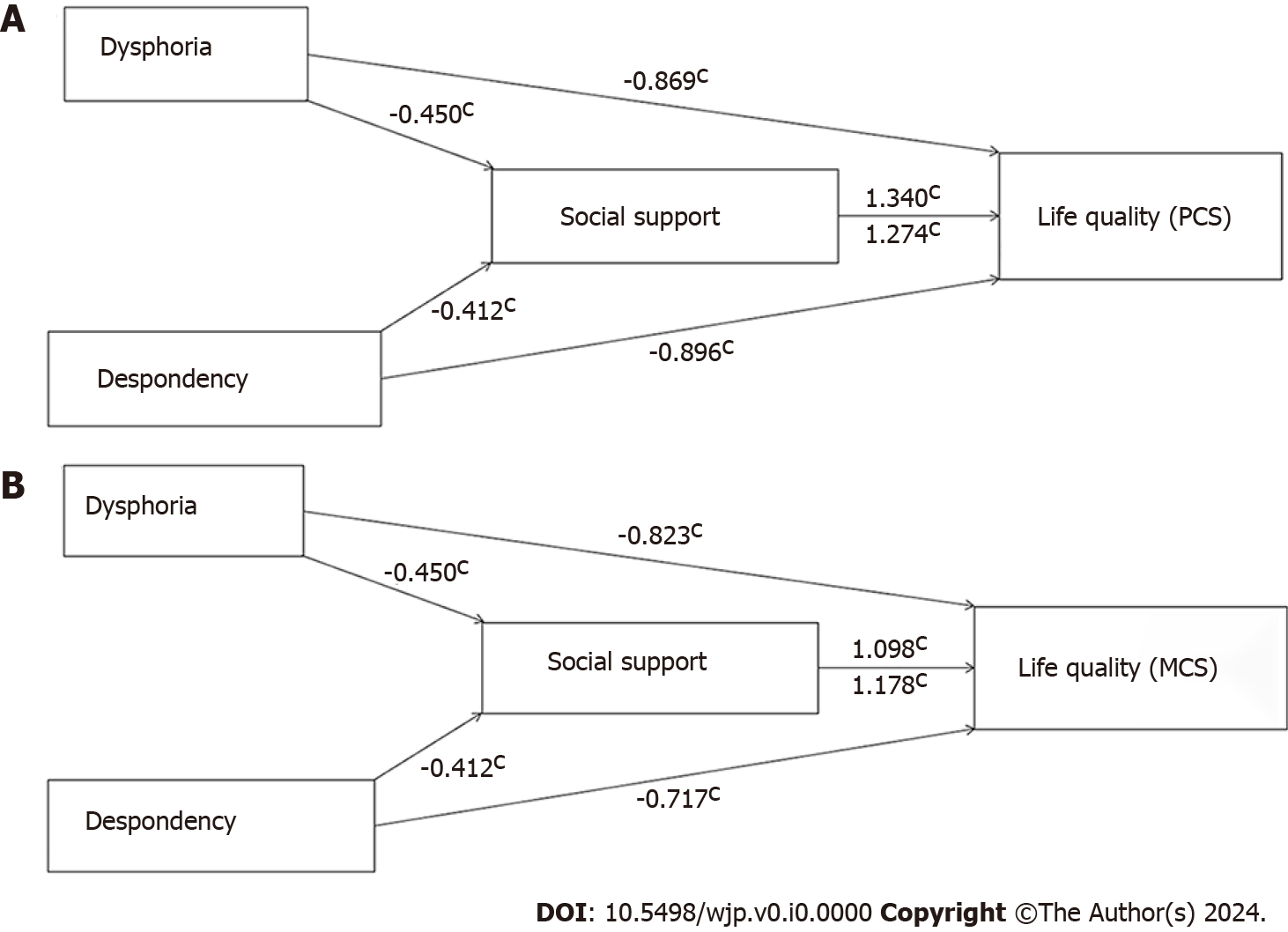
Dysphoria: In the first step, the regression coefficient was examined when dysphoria was considered the independent variable, and PCS and MCS were the dependent variables. Second, the regression coefficient was analyzed with dysphoria as the independent variable and social support as the dependent variable. In the third step, a regression equation was constructed, involving both dysphoria and social support as independent variables and PCS and MCS as dependent variables. The results revealed that dysphoria had a negative predictive effect on PCS and MCS (β = -0.869, β = -0.823, P < 0.05). Furthermore, dysphoria negatively predicted social support (β = -0.450, P < 0.05). The impact of dysphoria on PCS and MCS decreased when accounting for the presence of social support (β of PCS from -0.869 to -0.267, β of MCS from -0.823 to -0.329, P < 0.05). This suggests that social support partially mediated the relationship between dysphoria and QOL (PCS and MCS) in patients undergoing MHD (Table 8).
| Model path | Standard regression equation | β | SE | t | P value |
| Step 1 | Y1 = -0.869A | -0.869 | 0.087 | -9.963 | < 0.001 |
| Step 2 | M = -0.450A | -0.450 | 0.038 | -11.998 | < 0.001 |
| Step 3 | Y1 = -0.267A + 1.340M | -0.267 | 0.088 | -3.046 | 0.003 |
| 1.340 | 0.113 | 11.902 | < 0.001 | ||
| Step 1 | Y2 = -0.823A | -0.823 | 0.090 | -9.190 | < 0.001 |
| Step 2 | M = -0.450A | -0.450 | 0.038 | -11.998 | < 0.001 |
| Step 3 | Y2 = -0.329A + 1.098M | -0.329 | 0.098 | -3.371 | < 0.001 |
| 1.098 | 0.126 | 8.752 | < 0.001 |
Despondency: In the first step, the regression coefficient was assessed with despondency as the independent variable and PCS and MCS as the dependent variables. Second, the regression coefficient was investigated with despondency as the independent variable and social support as the dependent variable. In the third step, a regression equation was established involving both despondency and social support as independent variables and PCS and MCS as dependent variables. The findings indicated that despondency had a negative predictive effect on PCS and MCS (β = -0.896, β = -0.717, P < 0.05). Additionally, despondency negatively predicted social support (β = -0.412, P < 0.05). Importantly, the influence of despondency on PCS and MCS decreased when considering the presence of social support (β of PCS from -0.896 to -0.372, β of MCS from -0.717 to -0.232, P < 0.05). This implies that social support played a partial mediating role in the relationship between despondency and QOL (PCS and MCS) in patients undergoing MHD (Table 9).
| Model path | Standard regression equation | β | SE | t | P value |
| Step 1 | Y1 = -0.896B | -0.896 | 0.084 | -10.709 | < 0.001 |
| Step 2 | M = -0.412B | -0.412 | 0.038 | -10.891 | < 0.001 |
| Step 3 | Y1 = -0.372B + 1.274M | -0.372 | 0.082 | -4564 | < 0.001 |
| 1.274 | 0.107 | 11.888 | < 0.001 | ||
| Step 1 | Y2 = -0.717B | -0.717 | 0.090 | -7.945 | < 0.001 |
| Step 2 | M = -0.412B | -0.412 | 0.038 | -10.891 | < 0.001 |
| Step 3 | Y2 = -0.232B + 1.178M | -0.232 | 0.093 | -2.483 | 0.014 |
| 1.178 | 0.123 | 9.590 | < 0.001 |
To further assess the mediating effect of social support on dysphoria, despondency, and QOL in patients undergoing MHD, a bootstrap method was employed. The bootstrap 95%CI was analyzed but did not include 0.
Dysphoria: The direct effects of dysphoria on PCS and MCS were statistically significant (P < 0.05), accounting for 30.61% and 40.10% of the total effect value, respectively. The mediating effect of social support on dysphoria, PCS, and MCS was significant (P < 0.05), accounting for 69.39% and 59.90% of the total effect value, respectively.
Despondency: The direct effects of despondency on PCS and MCS were statistically significant (P < 0.05), accounting for 41.52% and 32.36% of the total effect value, respectively. The mediating effect of social support on despondency, PCS, and MCS was significant (P < 0.05), accounting for 50.48% and 67.64% of the total effect value, respectively (Table 10 and Figure 2).
| The path | Coeff | SE | LLCI | ULCI | Relative effect Size (%) | ||
| Dysphoria | Direct effect | Dysphoria → Quality of life (PCS) | -0.266 | 0.088 | -0.439 | -0.094 | 30.61 |
| Indirect effect | Dysphoria → Social support → Quality of life (PCS) | -0.603 | 0.064 | -0.731 | -0.482 | 69.39 | |
| Total effect | -0.869 | 0.087 | -1.041 | -0.698 | |||
| Dysphoria | Direct effect | Dysphoria → Quality of life (MCS) | -0.330 | 0.098 | -0.521 | -0.137 | 40.10 |
| Indirect effect | Dysphoria → Social support → Quality of life (MCS) | -0.493 | 0.071 | -0.644 | -0.366 | 59.90 | |
| Total effect | -0.823 | 0.090 | -0.999 | -0.647 | |||
| Despondency | Direct effect | Despondency → Quality of life (PCS) | -0.372 | 0.082 | -0.533 | -0.212 | 41.52 |
| Indirect effect | Despondency → Social support → Quality of life (PCS) | -0.524 | 0.063 | -0.659 | -0.412 | 50.48 | |
| Total effect | -0.896 | 0.084 | -1.061 | -0.732 | |||
| Despondency | Direct effect | Despondency → Quality of life (MCS) | -0.232 | 0.093 | -0.416 | -0.048 | 32.36 |
| Indirect effect | Despondency → Social support → Quality of life (MCS) | -0.485 | 0.065 | -0.620 | -0.367 | 67.64 | |
| Total effect | -0.717 | 0.090 | -0.894 | -0.539 | |||
The buffer effect model of social support posits that when individuals encounter stressors, social support can mitigate the negative impact of these stressors on individuals[17]. In the context of long-term hemodialysis treatment, as time progresses and the disease advances, patients often experience significant psychological and financial burdens, leading to feelings of despondency and dysphoria. These emotional struggles can have a profound impact on the patient’s QOL for patients[18]. This study focused on patients undergoing MHD at our hospital’s blood dialysis center using a questionnaire-based investigation. We aimed to explore the relationship among social support, dysphoria, despondency, and QOL in these patients. Through correlation analysis, we constructed a mediating effect model to delve deeper into the role of social support in mediating the effects of dysphoria and despondency on QOL in patients undergoing MHD. Our findings provide valuable insights into targeted interventions to improve the QOL of these patients.
The results of this study revealed the following: (1) Among the 289 patients undergoing MHD included in the study, the incidences of dysphoria and despondency were 60.21% and 54.33%, respectively. Comparatively, Ye et al[19] reported an incidence rate of 36.89% for dysphoria (68.93% for despondency), whereas Meng et al[20] reported an incidence rate of 25.9% for dysphoria (55.1% for despondency). These variations in research results may be attributed to differences in the assessment scales used for patients undergoing MHD, regional economic development, educational level, living environment, and sample size. However, dysphoria and despondency are prevalent in patients undergoing MHD; (2) This study found a positive correlation between social support and QOL. Higher levels of social support were associated with a better QOL, which is consistent with the findings of Alexopoulou et al[21]. Social support encompasses the assistance provided by various social relationships. The psychological well-being of patients undergoing MHD is often influenced by the support they receive from their families and social environments. Social support plays a crucial role in helping patients effectively cope with various pressures and challenges[22]. Medical staff should pay close attention to the social support levels of patients undergoing MHD and collaborate with their families to provide assistance and support tailored to their individual needs, ultimately enhancing the quality of patients undergoing MHD; (3) This study found positive correlations between dysphoria and despondency and negative correlations between dysphoria, despondency, social support, and QOL. These findings are consistent with those reported by Al-Nashri and Almutary[23], Hoang et al[24], and Ma et al[1]. Our findings indicated that deeper dysphoria was associated with deeper despondency. Furthermore, increased levels of dysphoria and despondency are linked to lower levels of social support and diminished QOL. This relationship can be partially explained by the social isolation that may result from hemodialysis, which requires patients undergoing MHD to spend extended periods (3-4 h) in dialysis rooms at least twice a week. Psychological challenges, particularly dysphoria and despondency, often go unnoticed and can gradually affect physical and MH. Moreover, long-term dysphoria and despondency can lead to reduced social engagement and overall life satisfaction, negatively impacting quality[25]. To address this issue, medical staff should recognize that low social support may contribute to dysphoria and despondency in patients undergoing MHD. Intervention strategies can be developed to strengthen these patients’ social networks, encourage them to express their feelings, and address their psychological needs, thereby helping them cope with the emotional burden of their condition; and (4) This study revealed that social support mediated the relationship between dysphoria, despondency, and QOL. With increased social support, the adverse effects of dysphoria and despondency on QOL were mitigated, consistent with the findings of Shang et al[26] and Shukri et al[27]. Dysphoria and despondency not only directly influence the QOL of patients undergoing MHD but also indirectly affect it by shaping their level of social support. This implies that enhancing social support levels can improve the QOL of patients undergoing MHD who experience dysphoria and despondency. This improvement may be attributed to the encouragement and strength that patients on MHD derive from various forms of social support, thereby enabling them to cope better with life challenges and significantly enhancing their MH and overall QOL[28]. In clinical practice, it is advisable to develop tailored, individualized psychological intervention measures aimed at improving social support levels, boosting the confidence of patients undergoing MHD in managing their condition, and ultimately working toward the goal of enhancing their overall QOL.
This study had some limitations: (1) This study employed a cross-sectional design, and the participants were exclusively patients undergoing MHD at our hospital’s hemodialysis center. This single-source sample with a relatively small size could potentially limit the generalizability of the findings. Future research should consider conducting multicenter studies to enhance the representativeness of the results[29]; and (2) The research outcomes were based solely on data from patients in our hospital, which may not fully capture the experiences of all patients undergoing MHD in the broader region. To gain a more comprehensive understanding, future research should incorporate longitudinal studies that track the dynamics of social support, dysphoria, despondency, and life patients undergoing MHD.
This study revealed that dysphoria and despondency had a direct negative impact on the QOL of patients undergoing MHD. Additionally, social support plays a mediating role in the relationship between dysphoria, despondency, and QOL among patients undergoing MHD. Thus, enhancing the level of social support provided to patients on MHD can help mitigate the occurrence of dysphoria and despondency, ultimately leading to an improved QOL for these patients. These findings provide valuable insights for clinical staff and offer a theoretical basis for the implementation of targeted treatment and nursing care for patients undergoing MHD.
Patients undergoing Maintenance Hemodialysis (MHD) frequently experience dysphoria and despondency during extended dialysis treatment. These psychological difficulties can lead to alterations in daily routines, a decline in physical capabilities, a loss of social roles and status, and a profound influence on physical and mental well-being, along with overall quality of life (QOL). Consequently, enhancing their QOL is of the utmost importance.
Dysphoria and despondency can significantly diminish the QOL of patients undergoing MHD, whereas strong social support can enhance it. This study investigated the role of social support as a mediator between dysphoria, despondency, and QOL in patients undergoing MHD. This study aimed to establish a theoretical foundation for psychological interventions among patients undergoing MHD, enabling the implementation of effective strategies to boost social support levels and enhance their overall QOL.
The primary objective of this study was to investigate the influence of social support on dysphoria, despondency, and QOL in patients undergoing MHD. Additionally, it aimed to assess the mediating role of social support by constructing a mediating effect model that incorporated social support, dysphoria, despondency, and QOL. The ultimate goal was to enhance the level of social support for patients undergoing MHD, thereby mitigating the effects of dysphoria and despondency and ultimately improving their overall QOL.
This cross-sectional study included 289 patients from our hospital. The Social support rating scale, Self-rating anxiety scale, Self-rating depression scale, and Life quality scale were used to collect data. Correlation analysis was used to examine the associations between social support, dysphoria, despondency, and the QOL in patients undergoing MHD. Furthermore, the bootstrap method was employed to assess the mediating effect of social support on the relationships among dysphoria, despondency, and QOL in these patients.
The study revealed several key findings: (1) Social support was positively correlated with QOL and negatively correlated with dysphoria and despondency; (2) Dysphoria and despondency had a negative impact on the QOL of patients undergoing maintenance hemodialysis; (3) The negative impact of dysphoria and despondency on QOL decreased in the presence of social support; and (4) Social support played a significant mediating role in the relationship between dysphoria, despondency, and QOL. These findings provide valuable insights for healthcare professionals and offer a basis for the targeted treatment and improved care of patients undergoing MHD.
This study demonstrated that social support plays a mediating role in the relationship between dysphoria, despondency, and QOL in patients undergoing MHD. This study addressed the gap in the understanding of how social support influences the interplay between dysphoria, despondency, and QOL in patients undergoing MHD, providing a valuable theoretical foundation for future studies in this area.
Future research in this area should consider expanding the sample size and incorporating multi-regional samples to gain a more comprehensive understanding of the relationships among social support, dysphoria, despondency, and QOL in patients undergoing MHD. Additionally, longitudinal studies could provide valuable insights into the evolution of these factors over time in patients undergoing MHD.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Sousa RAL, Brazil; Marques A, Portugal S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Ma SJ, Wang WJ, Tang M, Chen H, Ding F. Mental health status and quality of life in patients with end-stage renal disease undergoing maintenance hemodialysis. Ann Palliat Med. 2021;10:6112-6121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Al Naamani Z, Gormley K, Noble H, Santin O, Al Maqbali M. Fatigue, anxiety, depression and sleep quality in patients undergoing haemodialysis. BMC Nephrol. 2021;22:157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Zhang H, Zhao Q, Cao P, Ren G. Resilience and Quality of Life: Exploring the Mediator Role of Social Support in Patients with Breast Cancer. Med Sci Monit. 2017;23:5969-5979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 121] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 4. | Gonzalez-Saenz de Tejada M, Bilbao A, Baré M, Briones E, Sarasqueta C, Quintana JM, Escobar A; CARESS-CCR Group. Association between social support, functional status, and change in health-related quality of life and changes in anxiety and depression in colorectal cancer patients. Psychooncology. 2017;26:1263-1269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Fleischman EK, Connelly CD, Calero P. Depression and Anxiety, Stigma, and Social Support Among Women in the Postpartum Period. Nurs Womens Health. 2022;26:95-106. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 6. | Pineda CN, Naz MP, Ortiz A, Ouano EL, Padua NP, Paronable JJ, Pelayo JM, Regalado MC, Torres GCS. Resilience, Social Support, Loneliness and Quality of Life during COVID-19 Pandemic: A Structural Equation Model. Nurse Educ Pract. 2022;64:103419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 7] [Reference Citation Analysis (0)] |
| 7. | Rao Q, Zeng J, Wang S, Hao J, Jiang M. Chronic Pain and Quality of Life in Maintenance Hemodialysis Patients in China: A Multicenter, Cross-Sectional Study. J Pain Res. 2022;15:147-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Ravindran A, Sunny A, Kunnath RP, Divakaran B. Assessment of Quality of Life among End-Stage Renal Disease Patients Undergoing Maintenance Hemodialysis. Indian J Palliat Care. 2020;26:47-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Najafi A, Keihani S, Bagheri N, Ghanbari Jolfaei A, Mazaheri Meybodi A. Association Between Anxiety and Depression With Dialysis Adequacy in Patients on Maintenance Hemodialysis. Iran J Psychiatry Behav Sci. 2016;10:e4962. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Shimizu U, Aoki H, Sakagami M, Akazawa K. Walking ability, anxiety and depression, significantly decrease EuroQol 5-Dimension 5-Level scores in older hemodialysis patients in Japan. Arch Gerontol Geriatr. 2018;78:96-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 277] [Cited by in F6Publishing: 584] [Article Influence: 146.0] [Reference Citation Analysis (0)] |
| 12. | Zhang H, Cui N, Chen D, Zou P, Shao J, Wang X, Zhang Y, Du J, Du C, Zheng D. Social support, anxiety symptoms, and depression symptoms among residents in standardized residency training programs: the mediating effects of emotional exhaustion. BMC Psychiatry. 2021;21:460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Xu J, Chen P, Ma X. The relationship among preconception depression, anxiety, and social support of the reproductive-aged women in China. Arch Womens Ment Health. 2018;21:429-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Lam CL, Tse EY, Gandek B, Fong DY. The SF-36 summary scales were valid, reliable, and equivalent in a Chinese population. J Clin Epidemiol. 2005;58:815-822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 15. | Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903-912. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1606] [Cited by in F6Publishing: 1651] [Article Influence: 63.5] [Reference Citation Analysis (0)] |
| 16. | Lin Y, Yu Y, Zeng J, Zhao X, Wan C. Comparing the reliability and validity of the SF-36 and SF-12 in measuring quality of life among adolescents in China: a large sample cross-sectional study. Health Qual Life Outcomes. 2020;18:360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 17. | Qiu Y, Huang Y, Wang Y, Ren L, Jiang H, Zhang L, Dong C. The Role of Socioeconomic Status, Family Resilience, and Social Support in Predicting Psychological Resilience Among Chinese Maintenance Hemodialysis Patients. Front Psychiatry. 2021;12:723344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Feroze U, Martin D, Kalantar-Zadeh K, Kim JC, Reina-Patton A, Kopple JD. Anxiety and depression in maintenance dialysis patients: preliminary data of a cross-sectional study and brief literature review. J Ren Nutr. 2012;22:207-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Ye W, Wang L, Wang Y, Wang C, Zeng J. Depression and anxiety symptoms among patients receiving maintenance hemodialysis: a single center cross-sectional study. BMC Nephrol. 2022;23:417. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 20. | Meng Y, Wu HT, Niu JL, Zhang Y, Qin H, Huang LL, Zhang XJ, Yu L, Yu HY, Yan T, Zhao JR. Prevalence of depression and anxiety and their predictors among patients undergoing maintenance hemodialysis in Northern China: a cross-sectional study. Ren Fail. 2022;44:933-944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Alexopoulou M, Giannakopoulou N, Komna E, Alikari V, Toulia G, Polikandrioti M. The effect of perceived social support on hemodialysis patients' quality of life. Mater Sociomed. 2016;28:338-342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Alshraifeen A, Al-Rawashdeh S, Alnuaimi K, Alzoubi F, Tanash M, Ashour A, Al-Hawamdih S, Al-Ghabeesh S. Social support predicted quality of life in people receiving haemodialysis treatment: A cross-sectional survey. Nurs Open. 2020;7:1517-1525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Al-Nashri F, Almutary H. Impact of anxiety and depression on the quality of life of haemodialysis patients. J Clin Nurs. 2022;31:220-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 24. | Hoang VL, Green T, Bonner A. Examining social support, psychological status and health-related quality of life in people receiving haemodialysis. J Ren Care. 2022;48:102-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Wang X, Xia F, Wang G. Mediating effect of anxiety and depression between family function and hope in patients receiving maintenance hemodialysis: a cross-sectional study. BMC Psychol. 2023;11:130. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 26. | Shang F, Kaniasty K, Cowlishaw S, Wade D, Ma H, Forbes D. The impact of received social support on posttraumatic growth after disaster: The importance of both support quantity and quality. Psychol Trauma. 2022;14:1134-1141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Shukri M, Mustofai MA, Md Yasin MAS, Tuan Hadi TS. Burden, quality of life, anxiety, and depressive symptoms among caregivers of hemodialysis patients: The role of social support. Int J Psychiatry Med. 2020;55:397-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Peng L, Ye Y, Wang L, Qiu W, Huang S, He F, Deng L, Lin J. Chain Mediation Model of Perceived Stress, Resilience, and Social Support on Coping Styles of Chinese Patients on Hemodialysis During COVID-19 Pandemic Lockdown. Med Sci Monit. 2022;28:e935300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Liu YM, Chang HJ, Wang RH, Yang LK, Lu KC, Hou YC. Role of resilience and social support in alleviating depression in patients receiving maintenance hemodialysis. Ther Clin Risk Manag. 2018;14:441-451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |