Copyright
©The Author(s) 2025.
World J Crit Care Med. Sep 9, 2025; 14(3): 102577
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.102577
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.102577
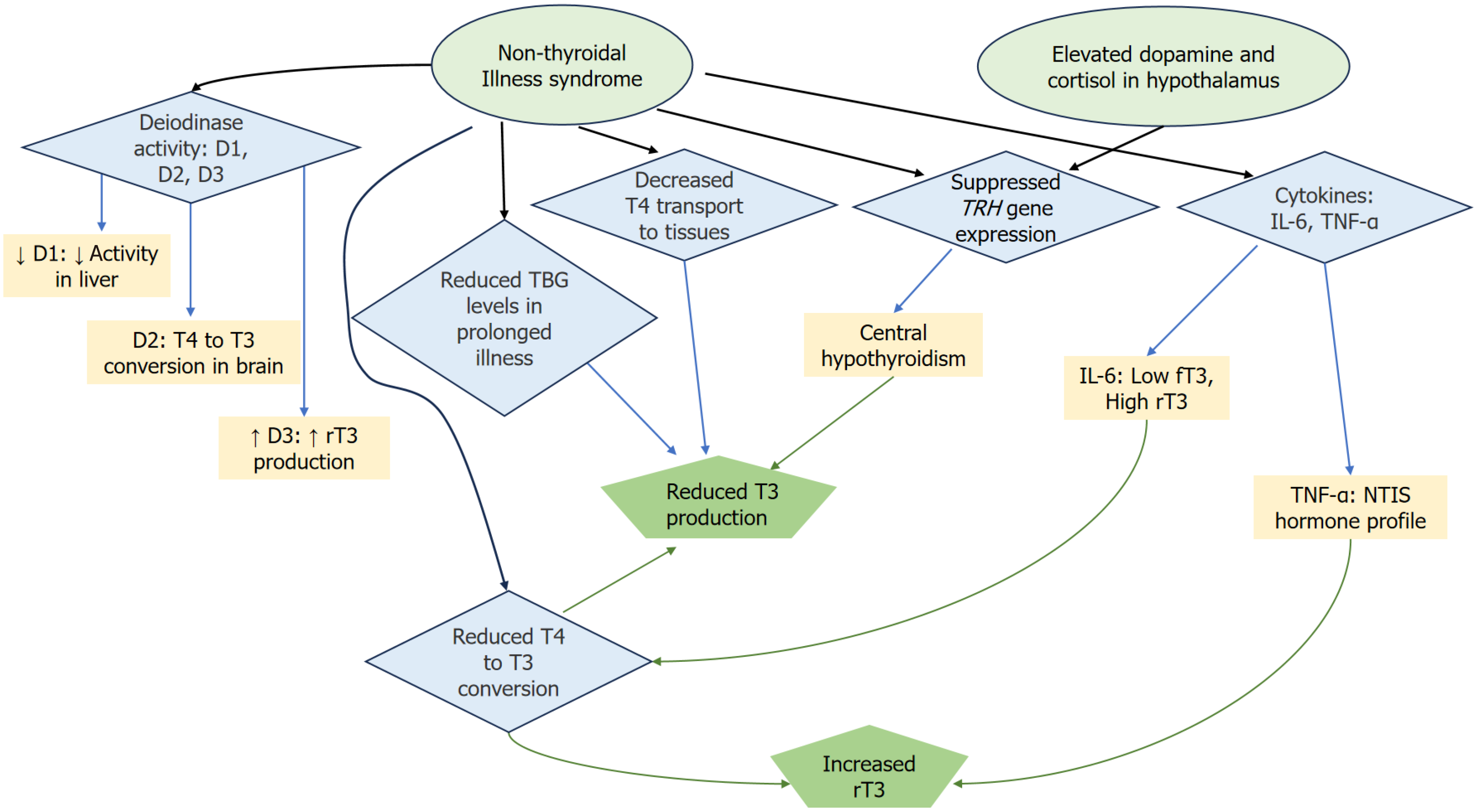
Figure 1 Outline of the pathophysiology of nonthyroidal illness syndrome, focusing on the interactions between deiodinases, cytokines, and hormonal regulation.
Reduced D1 activity in the liver leads to decreased thyroxine (T4) to triiodothyronine (T3) conversion, while D3 increases the production of reverse T3 (rT3). However, D2 in the brain remains active, allowing local T4 to T3 conversion and maintaining brain T3 levels, despite systemic disruptions. Elevated levels of dopamine and cortisol in the hypothalamus lead to the suppression of TRH gene expression, which in turn contributes to central hypothyroidism. The diagram also highlights the role of cytokines, particularly interleukin (IL)-6 and tumor necrosis factor-alpha (TNF-α), in disrupting thyroid hormone metabolism. IL-6 negatively correlates with free T3 and positively with rT3 levels, while TNF-α reproduces the typical hormone profile of NTIS when introduced into healthy individuals. Additionally, a reduction in T4 transport to tissues and lowered thyroxine-binding globulin levels (reduced T4 and T3 transport, impaired hormone availability) further exacerbate the hormonal imbalance during prolonged illness. Together, these mechanisms contribute to the complex hormonal dysregulation seen in nonthyroidal illness syndrome. rT3: Reverse T3; IL: Interleukin; TNF-α: Tumor necrosis factor-alpha; NTIS: Nonthyroidal illness syndrome.
- Citation: Savvidis C, Ragia D, Kallistrou E, Kouroglou E, Tsiama V, Proikaki S, Belis K, Ilias I. Critical illness-implications of non-thyroidal illness syndrome and thyroxine therapy. World J Crit Care Med 2025; 14(3): 102577
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/102577.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.102577