Copyright
©The Author(s) 2025.
World J Crit Care Med. Sep 9, 2025; 14(3): 101462
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.101462
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.101462
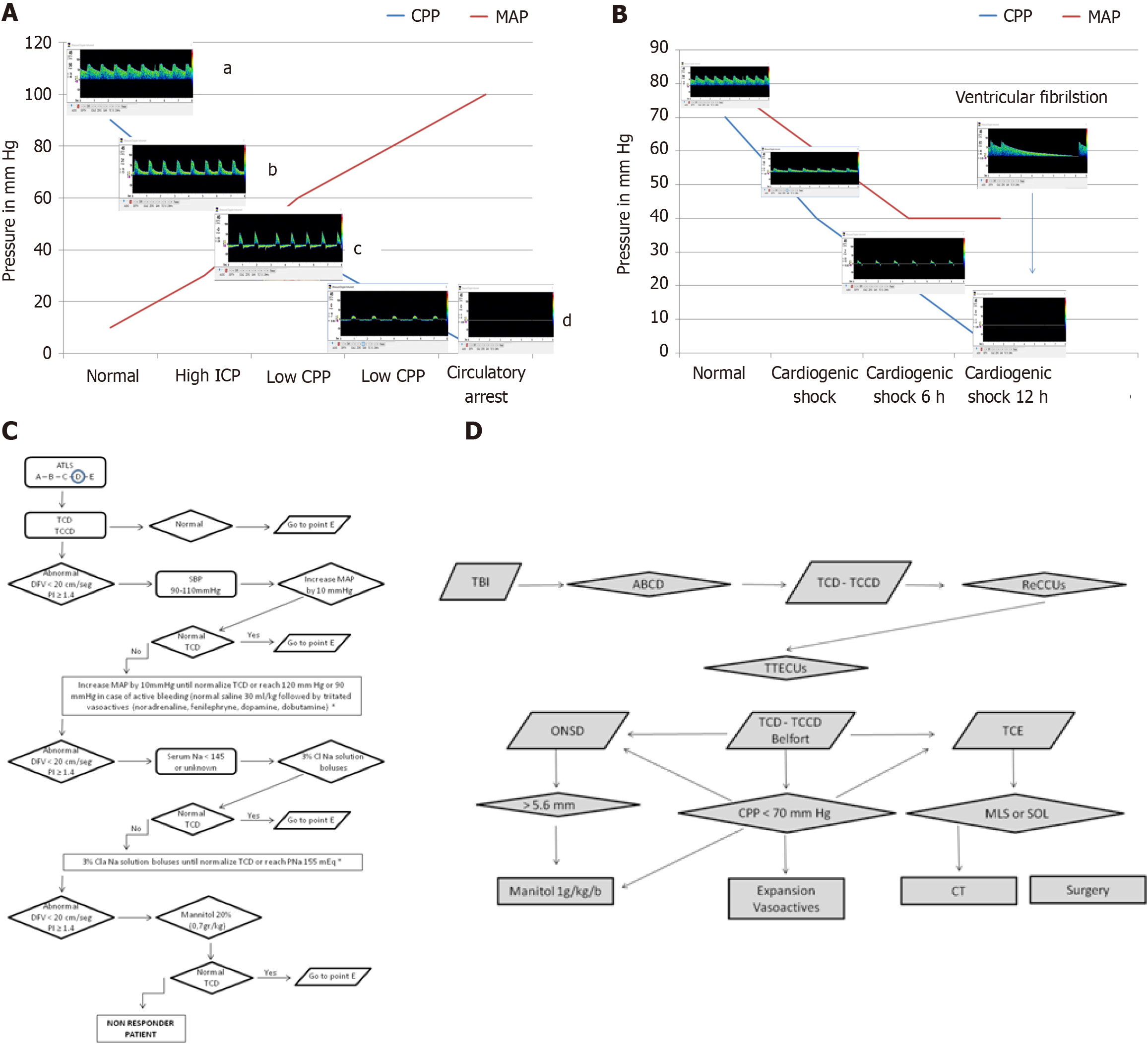
Figure 7 Cardio-cerebral coupling in health and disease.
A: Changes in flow velocities as cerebral perfusion pressures (CPP) decreases due to increasing intracranial pressure (ICP). aNormal flow: CPP at 90 mmHg and ICP at 10 mmHg ensures adequate cerebral perfusion with normal diastolic flow velocity (DFV) and pulsatility index. bHigh ICP: An increase in cerebral vascular resistance due to elevated ICP leads to compromised DFV and elevated pulsatility index. cLow CPP: Further increases in cerebral vascular resistance, coupled with low CPP, progress to reverberant flow. If sustained, this can evolve into small systolic spikes or complete flow absence. dCerebral circulatory arrest (CCA): The presence of reverberant flow or systolic spikes for more than 30 minutes is indicative of CCA, as defined by most brain death criteria; B: Changes in flow velocities as cardiogenic shock progresses. Early phase: Cardiogenic shock leads to a gradual decrease in all flow velocities, with a more pronounced reduction in DFV. Reverberant flow: After 6 hours, the typical pattern of reverberant flow emerges, characterized by oscillating flow without effective forward perfusion. CCA: Sustained reverberant flow or the appearance of complete flow absence (total CCA) is observed. Prolonged ventricular fibrillation can also result in this pattern. The presence of reverberant flow for more than 30 minutes is a reliable indicator of CCA, as defined by most brain death legislations; C: The ultrasound-guided cardio-cerebral resuscitation protocol. The Advanced Trauma Life Support® systematic approach includes airway, breathing, circulation, disability, and exposure; D: The ultrasound-guided brain injury treatment protocol. Following initial resuscitation using the ultrasound-guided brain injury treatment protocol, CPP is assessed using Belfort’s formula, ICP is estimated via optic nerve sheath diameter, and brain morphology is evaluated using B-mode transcranial ultrasound. If CPP < 70 mmHg, fluid expansion and vasoactive agents are immediately initiated. Simultaneously, optic nerve sheath diameter is measured. If ICP is elevated, a mannitol bolus is administered. If transcranial ultrasound reveals a midline shift or space-occupying lesion, the patient is immediately transferred to the computed tomography suite for surgical evaluation. This protocol ensures a systematic, ultrasound-guided approach to managing traumatic brain injury and optimizing cerebral perfusion. CPP: Cerebral perfusion pressures; ICP: Intracranial pressure; ATLS: Advanced Trauma Life Support®; TCD: Transcranial Doppler; TCCD: Transcranial color-coded Doppler; DFV: End-diastolic flow velocity; PI: Pulsatility index; SBP: Systolic blood pressure; MAP: Mean arterial pressure; TBI: Traumatic brain injury; ReCCUs: Ultrasound-guided cardio-cerebral resuscitation protocol; TTECUs: Ultrasound-guided brain injury treatment protocol; ONSD: Optic nerve sheath diameter; TCE: B-mode transcranial ultrasound; MLS: Midline shift; SOL: Space-occupying lesion; CT: Computed tomography.
- Citation: Previgliano IJ, Aboumarie HS, Tamagnone FM, Merlo PM, Sosa FA, Feijoo J, Carruega MC. Point of care ultrasound evaluation of cardio-cerebral coupling. World J Crit Care Med 2025; 14(3): 101462
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/101462.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.101462