Copyright
©The Author(s) 2025.
World J Crit Care Med. Sep 9, 2025; 14(3): 101462
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.101462
Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.101462
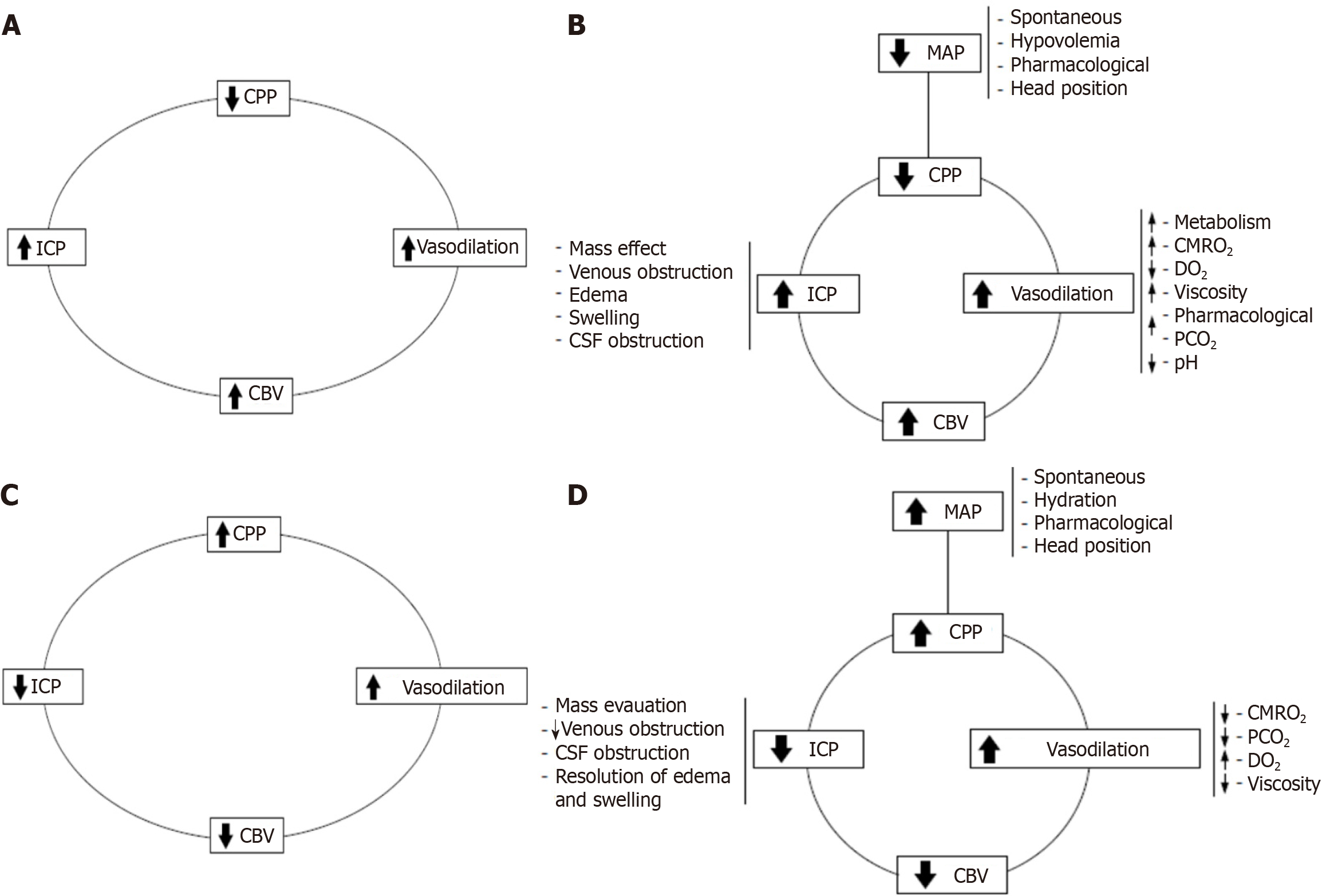
Figure 3 The vasodilator and vasoconstrictor cascades.
A: Vasodilator cascade. A decrease in cerebral perfusion pressures (CPP) triggers vasodilation as a compensatory mechanism to maintain cerebral blood flow. It is evident that vasodilation increases cerebral blood volume, which, according to the Monro-Kellie doctrine, raises intracranial pressure (ICP). This rise in ICP further reduces CPP, creating a self-perpetuating vicious cycle; B: Complex vasodilator cascade. This framework helps clarify many seemingly contradictory events and illustrates how the cycle can be initiated by any of its primary components; C: Vasoconstrictor cascade. With constant levels of partial carbon dioxide pressure, cerebral metabolic rate of oxygen consumption, and related variables, an increase in CPP induces vasoconstriction, which reduces cerebral blood volume and ICP, thereby enhancing CPP. This mechanism is effective only if the patient is within or near their autoregulatory range; D: Complex vasoconstrictor cascade. Management strategies can target any single component of the cascade or employ a combination of multiple components for optimal effect. CPP: Cerebral perfusion pressures; ICP: Intracranial pressure; CBV: Cerebral blood volume; MAP: Mean arterial pressure; CSF: Cerebrospinal fluid; CMRO2: Cerebral metabolic rate of oxygen; PCO2: Partial carbon dioxide pressure; DO2: Oxygen delivery.
- Citation: Previgliano IJ, Aboumarie HS, Tamagnone FM, Merlo PM, Sosa FA, Feijoo J, Carruega MC. Point of care ultrasound evaluation of cardio-cerebral coupling. World J Crit Care Med 2025; 14(3): 101462
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/101462.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.101462