Published online Nov 28, 2013. doi: 10.5412/wjsp.v3.i3.37
Revised: September 3, 2013
Accepted: November 1, 2013
Published online: November 28, 2013
Processing time: 218 Days and 1.1 Hours
AIM: To compare our ten year results for thyroidectomy for cervico-mediastinal goiters with the best surgical treatment reported in the literature.
METHODS: From January 2000 to December 2009, of 1530 patients who underwent thyroidectomy in our department, we selected 105 cases of cervico-mediastinal goiter. In the majority of cases, the cervical approach is the standard procedure and only occasionally sternotomy or thoracotomy is necessary. The indications for surgery are generally related to a progressive increase of the thyroid mass into the anterior mediastinum with compression and dislocation of the trachea or esophagus and the possibility of an unknown malignancy.
RESULTS: In 98 (93.3%) of our 105 patients, the standard surgical approach was anterior cervicotomy followed by total thyroidectomy. In three cases, total sternotomy was performed and in the remaining four patients, a partial split sternotomy was effective to remove the intrathoracic mass. Post-operative complications included transient recurrent laryngeal nerve palsy in 6 patients (5.7%) which only became permanent in 2 patients (1.9%). The transient hypoparathyroidism rate was 22% but 2 mo after surgery permanent hypoparathyroidism was confirmed in only 2% of our selected group. No patients required temporary tracheostomy following surgery related to a possible bilateral nerve palsy. Patients received a single prophylactic antibiotic dose preoperatively and wound infections were not significant. There was no mortality in our selected group and most patients showed a significant improvement of dyspnea and other correlated symptoms postoperatively.
CONCLUSION: The majority of cervico mediastinal goiters can be completely removed through a cervical incision. In selected cases, generally malignancies with local infiltration of mediastinal soft tissues and adhesions to large vessels, split sternotomy may be a safer approach to not increase morbidity.
Core tip: The majority of cervico-mediastinal goiters can be completely removed through a cervical incision. Volume reduction by a vascular peduncle ligature can facilitate the extraction of big goiters, with the result that sternotomy or thoracotomy is seldom necessary. Care must be taken to avoid recurrent laryngeal nerve injuries.
- Citation: Magistrelli P, D’Ambra L, Bonfante P, Francone E, Leoncini R, Cappagli M, Falco E. Treatment of cervico-mediastinal goiters. World J Surg Proced 2013; 3(3): 37-40
- URL: https://www.wjgnet.com/2219-2832/full/v3/i3/37.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v3.i3.37
Cervico-mediastinal goiters are a common pathology and their incidence may reach 15% of patients undergoing thyroidectomy[1]. There is agreement that in the majority of cases, cervical approach is the standard procedure and only occasionally sternotomy or thoracotomy is necessary[2]. The indications for surgery are generally related to a progressive increase of the thyroid mass into the anterior mediastinum with compression and dislocation of the trachea or esophagus and the possibility of an unknown malignancy.
In the past, medical treatment based on thyroxine was considered the first option to reduce the size of the gland. Now, surgery is also considered an appropriate treatment as negative intrathoracic pressure and retrosternal space tend to facilitate the migration of the goiter into the chest[3]. We retrospectively reviewed our ten year experience to evaluate the choice of surgical approach, notes of surgical technique and range of complications with the aim to compare our results with the best surgical treatment reported in the literature.
Cervico-mediastinal goiter is defined as a thyroid mass extending into the mediastinum in the prevascular or retrovascular space, reaching at least the level of the aortic arch. Surgical therapy considers extrathoracic enucleation of the thyroid mass. In this study, we excluded multinodular goiters with minimal or limited substernal extension.
From January 2000 to December 2009, of 1530 cases who underwent thyroidectomy in our department, we selected 105 patients operated on for cervico-mediastinal goiter. A total of 71 patients were women and 34 men, with a mean age of 61 years (range 22-80). All patients were referred to our unit by specialists and preoperative work up included blood examination and functional thyroid tests, chest X ray and a computed tomography (CT) scan to evaluate intrathoracic extension of the goiter. Only 23 of 105 patients underwent fine needle aspiration because of suspected nodules. The most frequent clinical symptoms are indicated in Table 1. Predominantly, patients reported a history of mild or severe dyspnea, although a considerable proportion (12 patients, 11.4%) had no palpable mass in the neck. In 5 cases (4.7%), the compression and dislocation of the trachea was masked by other conditions such as obstructive chronic diseases and asthma.
| Symptoms | No. of patients |
| Dyspnea | 75 (71) |
| Dysphagia | 17 (16) |
| Neck mass | 86 (82) |
| Hoarseness | 14 (13) |
In 98 (93.3%) of our 105 patients, the standard surgical approach was anterior cervicotomy followed by total thyroidectomy. In three cases, total sternotomy was performed and in the remaining four patients, a partial split sternotomy was effective in removing the intrathoracic mass.
The combined approach was performed in the five cases of malignancy (3 papillary and 2 medullary carcinoma) and in two patients in which the inveterate multinodular goiters had established important adhesions with the mediastinal surrounding soft tissues.
Over the last five years, consolidation of our experience has avoided performing sternotomy even in cases of cervico-mediastinal goiters with development in the retrovascular space. The vast majority of patients were discharged in the second post-operative day. Two patients needed a re-exploration for wound hematoma and another three required further checks of blood calcium level.
Post-operative complications included transient recurrent laryngeal nerve palsy in 6 patients (5.7%) which only became permanent in 2 patients (1.9%). The transient hypoparathyroidism rate was 22% but 2 mo after surgery permanent hypoparathyroidism was confirmed in only 2% of our selected group. No patients required temporary tracheostomy following surgery related to a possible bilateral nerve palsy. Patients received a single prophylactic antibiotic dose preoperatively and wound infections were not significant. Definitive histology of the specimens is indicated in Table 2.
| Histology | n (%) |
| Benign multinodular disease | 86 (8.2) |
| Papillary carcinoma | 12 (11.5) |
| Follicular carcinoma | 5 (4.8) |
| Medullary carcinoma | 2 (1.9) |
There was no mortality in our selected group and most patients showed a significant improvement of dyspnea and other correlated symptoms postoperatively.
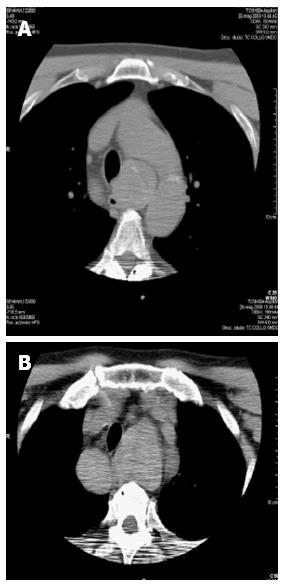
Our selected group of patients was composed of cases with a prevalent anterior development of the cervical mass (Figure 1) and cases with dominant extension into the anterior mediastinum (Figure 2A). Development in the retrosternal space is favored by negative intrathoracic pressure and by gravity mechanisms. At first examination, the chest X-ray indicates the right or left dislocation of the trachea and this radiological evidence requires a CT scan for further definition of intrathoracic goiter (Figure 2).
In case of difficult oral intubation, evaluated preoperatively by the anesthesiologist, a fiber optic bronchoscopy guide was considered to facilitate the procedure.
The standard surgical approach to perform total thyroidectomy was cervicotomy. Sternotomy has to be considered a selective option in cases of malignancy with soft tissue infiltration and/or gross mediastinal masses and lymphadenopathies which require a more aggressive surgery[4,5]. We needed to execute total sternotomy only in the past decade. Nowadays, we perform split sternotomy in cases of invasive malignancy to avoid hemorrhage originating from mediastinal vessel laceration and malignant tumor relapses. Other factors that can influence the likelihood of sternotomy are posterior mediastinal and ectopic goiters. In these cases, gentle handle maneuvres do not permit a sufficient traction for enucleation[6]. A mediastinal CT scan may be an important predictive factor. The presence of a clear plane around the intrathoracic nodule may be an indicator for a successful cervical approach[1].
Our surgical strategy is based on two principles: (1) the section of superior thyroid peduncles and (2) clear evidence of recurrent laryngeal nerve course.
As a priority, we section superior vascular pedicles to reduce thyroid vascularization and consequently volume and tension of the gland. The further step is cervical enucleation of the mediastinal mass by using careful hand maneuvres.
Once the goiter is reduced, it is necessary to identify recurrent laryngeal nerves and following their course up to the larynx to avoid possible damage to a dislocated or compressive nerve caused by the thyroid mass (Figure 3). We do not section any structure until there is clear identification of the nerves and we emphasize this procedure because the recurrent laryngeal branches may reach the larynx with extreme variability through the tracheoesophageal groove.
Recently, a new technique based on nerve monitoring during surgery has been considered a good option that reduces but does not eliminate the risk of laryngeal nerve palsy. This electromyography, which is becoming a standard procedure in the United States, is becoming accepted in Europe, especially for legal medical reasons[7].
At the moment, we are only considering nerve monitoring technique in cases of large relapsing goiters and this is because we systematically identify the nerves before any tissue section. However, the reported risk of nerve palsy using the monitoring technique is still around 1%[7]. It must be emphasized that the complications of thyroid surgery need to be avoided for the important functional impact on the life quality of patients. There is agreement that this type of surgery needs to be performed by dedicated specialist surgeons. The majority of cervico-mediastinal goiters can be completely removed through a cervical incision.
In very selected cases, generally for malignancies with local infiltration of mediastinal soft tissues and adhesions to large vessels, split sternotomy may be a safer approach without increasing morbidity. Regular and systematic bilateral identification of recurrent laryngeal nerves and their variations is a priority to avoid complications. Our results are similar to the experiences reported by several specialized center series.
The cervico-mediastinal goiter rate is about 15% of patients who undergoing thyroidectomy. Common agreement exists that in the majority of cases, the surgical cervical approach is the standard procedure and only occasionally sternotomy or thoracotomy is necessary. The indications for surgery are generally related to a progressive increase of the thyroid mass into the anterior mediastinum with compression and dislocation of the trachea or esophagus and the possibility of an unknown malignancy. In very selected cases, generally malignancies with local infiltration of mediastinal soft tissues and adhesions to large vessels, split sternotomy may be a safer approach without increasing morbidity.
The standard surgical approach to perform total thyroidectomy is cervicotomy. Sternotomy has to be considered a selective option in case of cervico-mediastinal goiters and malignancy with soft tissue infiltration and/or gross mediastinal masses and lymphadenopathies which require a more aggressive surgery. The majority of cervico-mediastinal goiters can be completely removed through a cervical incision.
During thyroidectomy, identification of recurrent laryngeal nerves is mandatory to avoid possible injuries. Lately, a new technique based on nerve monitoring during surgery has been considered a valid option. In the authors’ experience, a nerve monitoring technique is used only in cases of large relapsing goiters because the nerves are usually identified before any tissue section. However, the reported risk of nerve palsy using a monitoring technique is still around 1%.
The authors compare their ten year results in a surgical approach for thyroidectomy for cervico-mediastinal goiters with the best surgical treatment reported in the literature.
The authors describe their experience of a cervicotomy approach for cervico-mediastinal goiters, focusing on a nerve preserving technique and also highlighting the feasibility of the above-mentioned surgical procedure in a giant thyroid.
P- Reviewer: Coskun A S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Zhang DN
| 1. | Cohen JP. Substernal goiters and sternotomy. Laryngoscope. 2009;119:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Cichoń S, Anielski R, Konturek A, Baczyński M, Cichoń W, Orlicki P. Surgical management of mediastinal goiter: risk factors for sternotomy. Langenbecks Arch Surg. 2008;393:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Ahmed ME, Ahmed EO, Mahadi SI. Retrosternal goiter: the need for median sternotomy. World J Surg. 2006;30:1945-198; discussion 1949. [PubMed] |
| 4. | Ríos A, Rodríguez JM, Galindo PJ, Torres J, Canteras M, Balsalobre MD, Parrilla P. Results of surgical treatment in multinodular goiter with an intrathoracic component. Surg Today. 2008;38:487-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Ben Nun A, Soudack M, Best LA. Retrosternal thyroid goiter: 15 years experience. Isr Med Assoc J. 2006;8:106-109. [PubMed] |
| 6. | Vadasz P, Kotsis L. Surgical aspects of 175 mediastinal goiters. Eur J Cardiothorac Surg. 1998;14:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 62] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Chiang FY, Lee KW, Chen HC, Chen HY, Lu IC, Kuo WR, Hsieh MC, Wu CW. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg. 2010;34:223-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 188] [Article Influence: 12.5] [Reference Citation Analysis (0)] |