Published online Mar 31, 2023. doi: 10.5412/wjsp.v13.i1.1
Peer-review started: November 25, 2022
First decision: January 17, 2023
Revised: February 16, 2023
Accepted: March 17, 2023
Article in press: March 17, 2023
Published online: March 31, 2023
Processing time: 125 Days and 11.4 Hours
Ossifying fibroma is a type of benign fibro-osseous lesion. Most lesions affect the mandible region, particularly the molar and pre-molar areas. It predominantly affects females between the second to fourth decades of life. Larger ossifying fibroma tumors require more extensive resection.
A 39-year-old female complained of occasional pain and tumor enlargement on her left jaw for the 3 years prior to presentation. Intraoral examination revealed a firm swelling on her left lower gum. Extraoral examination revealed swelling on the left mandible body with no erythema and superficial ulcer. Computed tomography scan revealed a circular-shaped lesion on the patient’s left mandible body with a well-defined radiolucent border, sized 3.2 cm × 2.8 cm × 0.9 cm. The tumor was removed by marginal mandibulectomy. Biopsy from the resected tumor suggested cemento-ossifying fibroma (COF).
COF is often unnoticed, but this slow-growing tumor can cause significant symptoms regarding its distortion into adjacent structures.
Core Tip: Ossifying fibroma is a benign fibro-osseous lesion that predominantly affects the craniofacial region. It is considered a rare tumor, with most lesions affecting the mandible region, particularly the molar and pre-molar areas. It is asymptomatic in most cases, but it can slowly grow until it is involved with the adjacent structures, leading to symptoms. The treatment is surgical excision, and it can be safely performed due to its well-demarcated nature. Recurrences can be avoided by extensive removal of the tumor. This case highlighted a case of a rare tumor with surgical excision and a good outcome.
- Citation: Christian INWS, Michael, Setiawan K. Cemento-ossifying fibroma of the left mandible: A case report. World J Surg Proced 2023; 13(1): 1-6
- URL: https://www.wjgnet.com/2219-2832/full/v13/i1/1.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v13.i1.1
Ossifying fibroma is a benign fibro-osseous lesion based on Waldron’s classification, which predominantly affects the craniofacial region[1]. It is considered a rare tumor, with most lesions affecting the mandible region, particularly the molar and pre-molar areas. It predominantly affects females with an incidence of 5:1 ratio compared to males and is commonly encountered between the second to fourth decade of life. It has characteristics of a slow-growing tumor, sometimes asymptomatic and expansive, which if left untreated may lead to signs and symptoms caused by an enlarged mass and significant involvement to the adjacent vital structures[2]. During its early stage, the tumor may appear small and well-demarcated, which can be safely enucleated. However, larger tumors require more extensive resection, in which reconstructions are sometimes needed[3]. In this study, we reported the clinical presentation of a cemento-ossifying fibroma (COF) on the patient’s left mandible, which was treated with lip-splitting incision and tumor excision through marginal mandibulectomy. This study aimed to share our experience with mandible COF and associated surgical approach.
A 39-year-old female patient complained of occasional pain in her left jaw for the 3 years prior to presentation. Shortly after, the patient noticed a small tumor on her gum, precisely below the first pre-molar tooth on her left mandible.
The tumor was slowly growing in size, and the pain frequency had increased more than before. The patient had no other comorbidities. The patient had undergone a panoramic radiographic examination, which revealed a singular, well-demarcated, circle-shaped lesion in the left mandible body below the second molar and first pre-molar teeth. Based on patient’s perspective, she felt that the tumor did not increase in size since her latest visit to the dentist.
The patient had no history of trismus and difficulty in masticating, although pain occasionally emerged during eating.
The patient did not have any previous medical conditions or other family history.
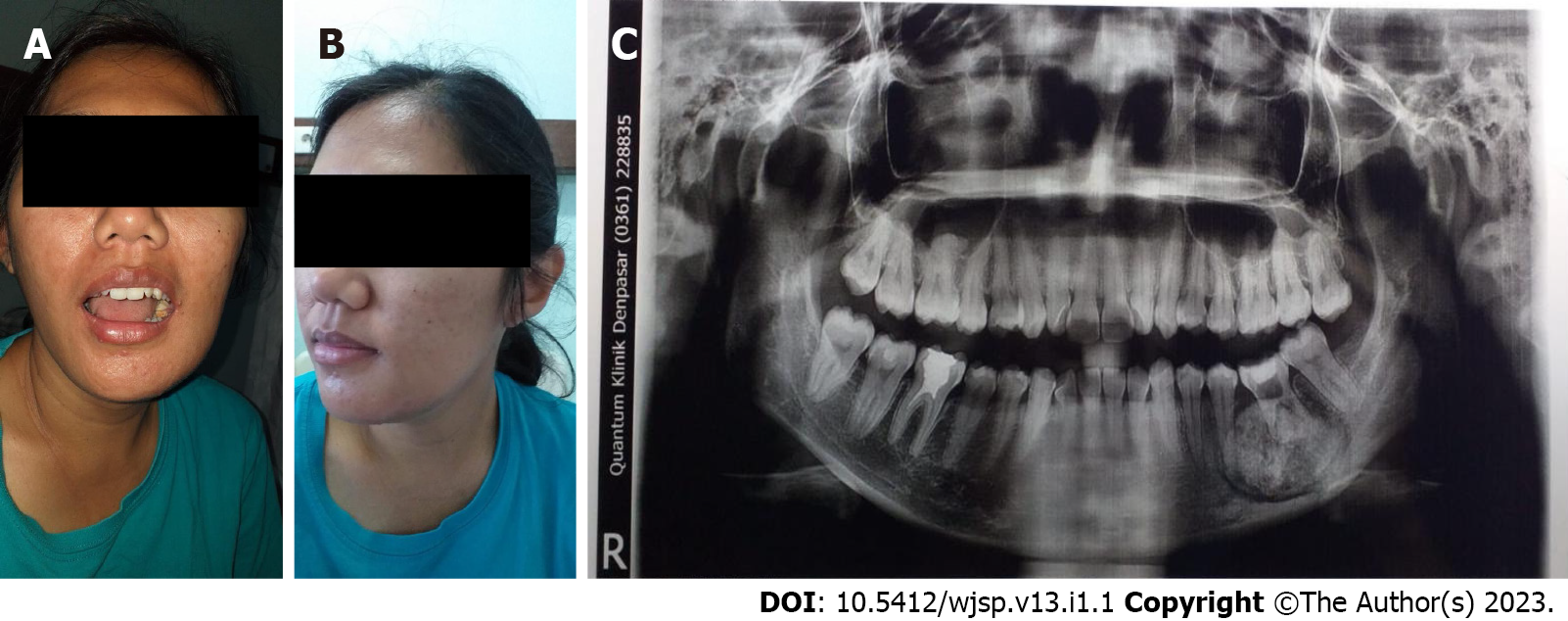
Intraoral examination revealed a firm swelling on her left lower gum, precisely below her previously drilled first pre-molar tooth. Mild tenderness was observed on percussion, but no tooth mobility was encountered. There was minimal swelling on the left mandible body with no erythema, superficial ulcer, and no other facial asymmetry on the extraoral examination. When palpated, the tumor was fixated with hard consistency, similar to bone (Figure 1).
A routine blood test was performed, and the results were within normal limits.
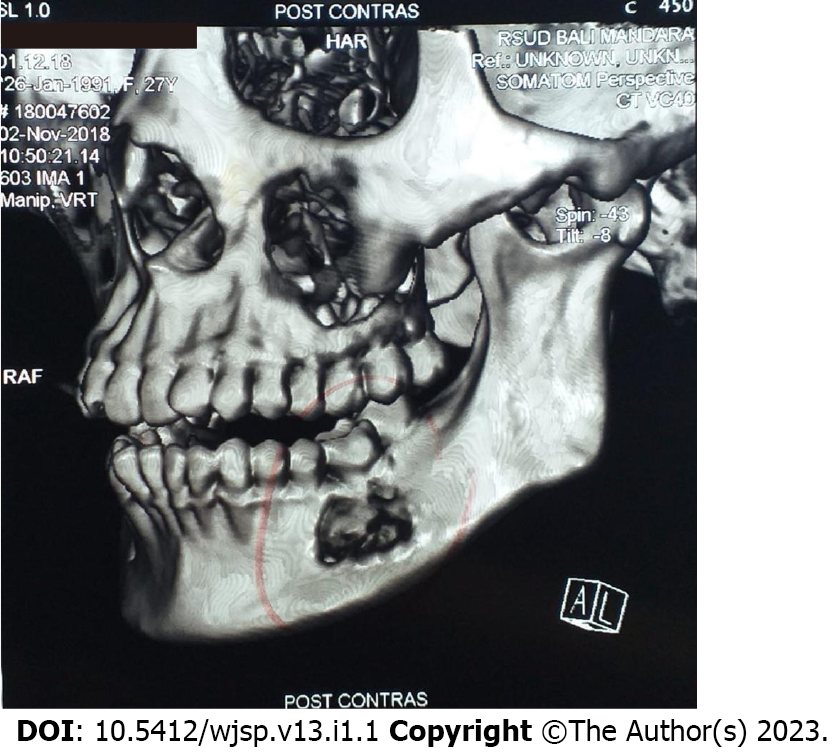
A computed tomography (CT) scan with 3D reconstruction revealed a circular-shaped lesion on the patient’s left mandible body with a well-defined radiolucent border between the lesion and surrounding normal bone, sized 3.2 cm × 2.8 cm × 0.9 cm (Figure 2). Fine-needle aspiration biopsy from the tumor suggested COF of the mandible. Based on these results, the patient was scheduled to undergo tumor removal with marginal mandibulectomy.
The final diagnosis of the presented case was COF of the mandible.
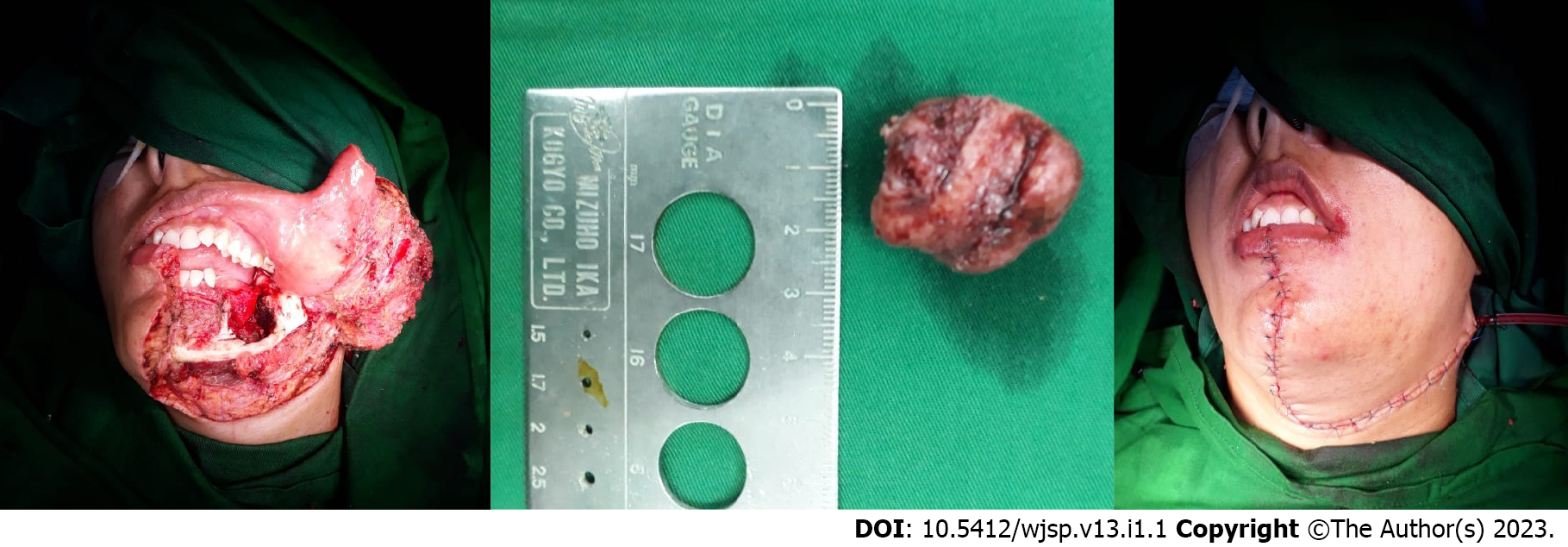
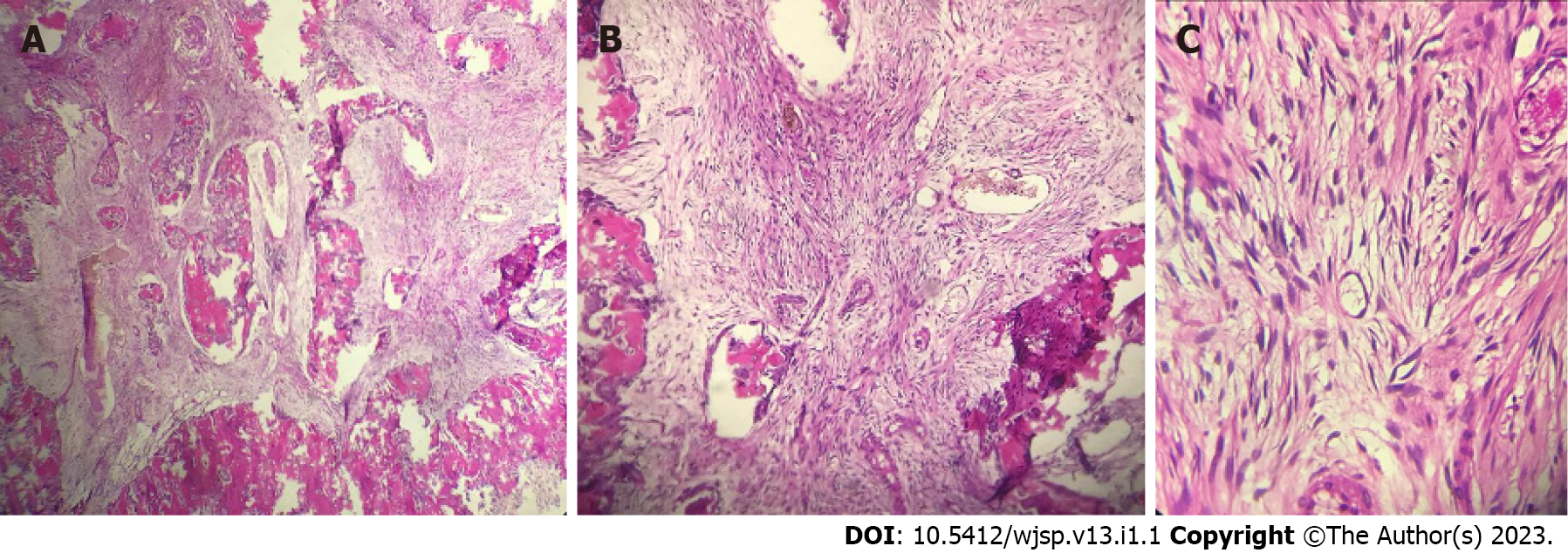
The patient was then admitted 2 d prior to the elective surgical procedure. On the operation day, the patient was positioned supine with her head slightly tilted to the opposite side. The patient then underwent general anesthesia with nasotracheal intubation. Lip-splitting incision was performed and extended towards the patient’s left angulus mandibulae. After the left mandible and the bony tumor were completely exposed, marginal mandibulectomy was performed. Marginal mandibulectomy was the preferred option in order to achieve 0.5 cm tumor margins. The periosteum was preserved to naturally construct the bone defects. Therefore, reconstruction will not be necessary in the future. Mandible plate fixation was not performed, as we maintained the integrity of the remaining mandible bone. Therefore, it will not cause soft tissue collapse, which we observed in the follow-up examinations. The wound was then washed with normal saline solution, minor bleeding was controlled, and drain insertion and wound closure using a subplatysmal flap were performed (Figure 3). The excised tumor was sent for pathology examination and described as an ossifying fibroma. From × 10 magnification, it showed the bone trabecular component and fibrous connective tissues along with fibroblast cell proliferation. From × 40 magnification, it showed spindle-shaped cells with cigar-shaped nuclei, eosinophilic cytoplasm, and smooth chromatin (Figure 4).
The patient had an uneventful postoperative clinical course with no postoperative complications. The drain was removed 3 d postoperative and showed no further rebleeding. At a follow-up visit 3 mo after the surgery, the pain was resolved, and she was asymptomatic. Panoramic radiographs were performed every 6 mo, and CT scan with 3D images were taken 1 year after surgery with satisfactory results without any recurrent lesions.
COF is a benign neoplasm that primarily affect the mandible and other craniofacial areas. COF consists of fibrous tissue, bone, and cementum in different proportions[1]. COF is one out of three variants of ossifying fibroma; the other variants are juvenile trabecular ossifying fibroma and juvenile psammomatoid ossifying fibroma[2]. These other variants reflect different demographics, their tendency to progress into malignant lesions, and their overall prognosis. The World Health Organization classifies COF as one of the fibro-osseous neoplasms, part of non-odontogenic tumors originating from periodontal ligament mesenchymal blast cells. It can progress into fibrous tissue, bone, cementum, or a combination of all three, as mentioned before[3]. However, this theory is still debatable, pointing to recent microscopic studies of COF arising from frontal, sphenoid, temporal, and ethmoid bones[4].
COF is asymptomatic in most cases, starting as a small unidentified tumor but slowly grows until it becomes noticeable as a swelling on the patient’s face and causes symptoms associated with its disturbance towards other structures. Due to its well-demarcated nature, enucleation and curettage of this lesion can be safely performed. However, larger lesions require more radical approaches, and inadequate surgical excision may result in recurrences[5]. One case report in 2021 by Guddadararangiah et al[6] presented a large mandible COF infiltrating parapharyngeal and infratemporal spaces, which required a hemi-mandibulectomy procedure. Another report in 2015 presented COF in a similar area to our case report but larger in size and treated with segmental mandibulectomy[7].
COF predominantly affects the mandible and commonly occurs in the molar and pre-molar areas. However, there were cases of COF found elsewhere other than the mandible area, such as in maxilla and orbital and ethmoidal regions. From a case series of 16 COF cases, 50% of these cases were found in the maxilla and the other 50% in the mandible region. There was 1 case of COF found in the right zygoma region with clinical presentation of diffuse swelling extending toward the upper vestibule[8]. Some COF cases in the maxilla region can cause facial deformities, sinus obstruction, and intraorbital and intracranial discomfort due to their involvement in adjacent structures. A recent report in 2020 presented a large, neglected COF of the maxilla region with a complaint of significant pressure on her left eye[4].
COF, regardless of its variant, location, and size, is a neoplasm that requires surgical excision. Depending on its size and location, treatment can be divided into conservative or radical surgery. While some authors reported no significant outcome between conservative and radical excision, others had suggested extensively removing the tumor, particularly aggressive lesions, to avoid any recurrences[5]. We preferred to extensively remove the tumor to avoid any recurrences in the future. A marginal mandibulectomy was a suitable option to remove the tumor adequately and safely. Lip-split incision was also preferred as a method of choice to expose the mandible adequately, as there are no significant differences in postoperative complications compared with the visor approach based on a retrospective review in 2018[9]. Marginal mandibulectomy was considered a feasible procedure, as the tumor had approached the mandible without infiltration toward tooth sockets and dental rehabilitation was not planned after surgery[10].
In other studies, all mandible COFs were treated locally. Kaur et al[8] in 2019 reviewed 16 maxillofacial COF cases, half of them affecting the mandible region. They found that 10 out of 16 cases were treated with enucleation and curettage, 5 cases were resected locally, and 1 case was resected en bloc with other involved structures. No patients developed any recurrences during follow-up observation. There were other studies in which the cases were managed extensively either by segmental or hemimandibulectomy due to massive size, and mandible plate reconstructions were performed[4-7]. One study reported a similar approach to our study, in which the tumor was safely excised with preservation of the inferior mandible border and without any reconstruction. Unfortunately, the outcome and follow-up reports were not mentioned[11].
One study interestingly preserved the mandible periosteum after large COF enucleation. They used periosteum osteogenesis potential to induce bone regeneration with a satisfactory result and no COF recurrence after 3 years of follow-up. It was based on the ability of the periosteum to act as a barrier to prevent soft tissue migration. Periosteum bone cells and its rich vascular supplies support adequate bone growth. With periosteum preservation, we can expect a bone restoration process from the post-excision defect area in our patient and reconstruction will not be necessary. However, Shirafkan et al[12] did reconstruct with mandible plate and screws.
COF is a benign neoplasm, usually asymptomatic, and predominantly affecting the mandible with a molar and pre-molar tooth as its predilected site. It is often unnoticed, but this slow-growing tumor can cause significant symptoms regarding its distortion into the adjacent structures. COF requires surgical excision, and larger tumors require a more extensive approach. Recurrences after removal are usually rare.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li JM, China; Mahmoudinezhad SS, Iran S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang H
| 1. | Balaji SM, Balaji P. Comparison of Midface Advancement by External and Internal Craniofacial Distraction Osteogenesis. Ann Maxillofac Surg. 2018;8:200-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Nelson BL, Phillips BJ. Benign Fibro-Osseous Lesions of the Head and Neck. Head Neck Pathol. 2019;13:466-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Darío SLJ, Paolo C, Miguel PP, Fernando M, Ismael R. Denosumab Related Osteonecrosis of the Jaws as Consequence of Osteoporosis Treatment-A Case Series. Saudi J Oral Dent Res. 2017;2:215-219. [DOI] [Full Text] |
| 4. | Aburas S, Bandura P, Al-Ibraheem A, Berger S, Meier M, Turhani D. A large maxillary cemento-ossifying fibroma superimposed with solitary bone cyst documented over 18 years: A case report. Int J Surg Case Rep. 2020;68:257-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 5. | Katti G, Khan MM, Chaubey SS, Amena M. Cemento-ossifying fibroma of the jaw. BMJ Case Rep. 2016;2016: bcr2015214327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Guddadararangiah S, Ram Shetty S, Al-Bayatti S, Narasimhan S. Large cemento-ossifying fibroma of the mandible involving the infratemporal and parapharyngeal spaces. Heliyon. 2021;7:e07594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | da Silveira DT, Cardoso FO, E Silva BJ, E Alves Cardoso CA, Manzi FR. Ossifying fibroma: report on a clinical case, with the imaging and histopathological diagnosis made and treatment administered. Rev Bras Ortop. 2015;51:100-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Kaur T, Dhawan A, Bhullar RS, Gupta S. Cemento-Ossifying Fibroma in Maxillofacial Region: A Series of 16 Cases. J Maxillofac Oral Surg. 2021;20:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Cohen LE, Morrison KA, Taylor E, Jin J, Spector JA, Caruana S, Rohde CH. Functional and Aesthetic Outcomes in Free Flap Reconstruction of Intraoral Defects With Lip-Split Versus Non-Lip-Split Incisions. Ann Plast Surg. 2018;80 (Suppl 4):S150-S155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Shah JP, Singh B, Patel SG, Wong RJ. Oral Cavity. In: Shah JP, Singh B, Patel SG, Wong RJ. Jatin Shah’s Head and Neck Surgery and Oncology. 5th ed. Edinburg: Elsevier; 2020: 256-257. |
| 11. | Bala TK, Soni S, Dayal P, Ghosh I. Cemento-ossifying fibroma of the mandible. A clinicopathological report. Saudi Med J. 2017;38:541-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Shirafkan S, Gholamian M, Rohani A, Mahmoudinezhad SS, Razavi M, Moradi K. Complete Spontaneous Bone Regeneration following Surgical Enucleation of a Mandibular Cemento-Ossifying Fibroma. Case Rep Dent. 2022;2022:7902602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |