Copyright
©The Author(s) 2016.
World J Immunol. Nov 27, 2016; 6(3): 126-130
Published online Nov 27, 2016. doi: 10.5411/wji.v6.i3.126
Published online Nov 27, 2016. doi: 10.5411/wji.v6.i3.126
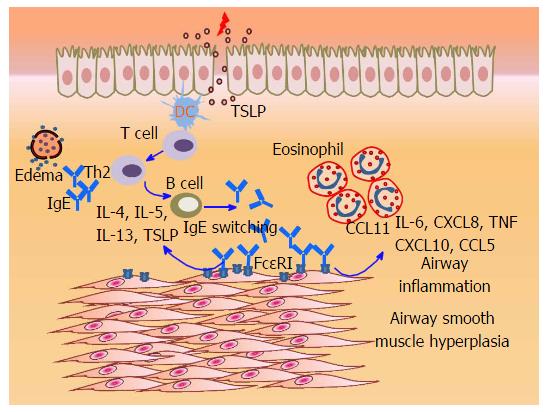
Figure 1 IgE sensitization-induced alterations in airway smooth muscle function.
Owing to edema or local IgE class switching in airway mucosa, IgE likely gains access to the sub-epithelial region where smooth muscle resides. In addition to other sources (T cells, epithelium), IgE stimulates the production of key Th2 cytokines (IL-4, -5, and -13) and thymic stromal lymphopoietin in ASM that may promote Th2-biased immune response within the airways. In addition, IgE-induced production of chemokines facilitates the recruitment of inflammatory cells including eosinophils. Most importantly, IgE stimulates ASM proliferation (hyperplasia), ultimately contributing to the airway wall thickness observed in allergic asthma. Notably, anti-IgE such as Omalizumab (not shown) has been shown to limit IgE-induced ASM synthetic and proliferative responses. TSLP: Thymic stromal lymphopoietin; TNF: Tumor necrosis factor; ASM: Airway smooth muscle.
- Citation: Redhu NS, Gounni AS. IgE regulates airway smooth muscle phenotype: Future perspectives in allergic asthma. World J Immunol 2016; 6(3): 126-130
- URL: https://www.wjgnet.com/2219-2824/full/v6/i3/126.htm
- DOI: https://dx.doi.org/10.5411/wji.v6.i3.126