Published online May 8, 2017. doi: 10.5409/wjcp.v6.i2.118
Peer-review started: May 3, 2016
First decision: July 27, 2016
Revised: October 23, 2016
Accepted: November 21, 2016
Article in press: November 22, 2016
Published online: May 8, 2017
Processing time: 384 Days and 2.3 Hours
To determine the true prevalence of thrombocytosis in children less than 2 years of age with bronchiolitis, its association with risk factors, disease severity and thromboembolic complications.
A retrospective observational medical chart review of 305 infants aged two years or less hospitalized for bronchiolitis. Clinical outcomes included disease severity, duration of hospital stay, admission to pediatric intensive care unit, or death. They also included complications of thrombocytosis, including thromboembolic complications such as cerebrovascular accident, acute coronary syndrome, deep venous thrombosis, pulmonary embolus, mesenteric thrombosis and arterial thrombosis and also hemorrhagic complications such as bleeding (spontaneous hemorrhage in the skin, mucous membranes, gastrointestinal, respiratory, or genitourinary tracts).
The median age was 4.7 mo and 179 were males (59%). Respiratory syncytial virus was isolated in 268 (84%), adenovirus in 23 (7%) and influenza virus A or B in 13 (4%). Thrombocytosis (platelet count > 500 × 109/L) occurred in 88 (29%; 95%CI: 24%-34%), more commonly in younger infants with the platelet count declining with age. There was no significant association with the duration of illness, temperature on admission, white blood cell count, serum C-reactive protein concentration, length of hospital stay or admission to the intensive care unit. No death, thrombotic or hemorrhagic events occurred.
Thrombocytosis is common in children under two years of age admitted with bronchiolitis. It is not associated with disease severity or thromboembolic complications.
Core tip: This is as a retrospective observational study of platelet counts in 305 infants aged two years or less who were hospitalized for bronchiolitis. Thrombocytosis (platelet count > 500 × 109/L) was frequent, occurring in 88 (29%; 95%CI: 24%-34%), more commonly in younger infants with the platelet count declining with age. There was no significant association with the duration of illness, temperature on admission, white blood cell count, serum C-reactive protein concentration, length of hospital stay, admission to the intensive care unit, death, thrombotic or hemorrhagic complications.
- Citation: Al Shibli A, Alkuwaiti N, Hamie M, Abukhater D, Noureddin MB, Amri A, Al Kaabi S, Al Kaabi A, Harbi M, Narchi H. Significance of platelet count in children admitted with bronchiolitis. World J Clin Pediatr 2017; 6(2): 118-123
- URL: https://www.wjgnet.com/2219-2808/full/v6/i2/118.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v6.i2.118
Bronchiolitis is a common viral infection in young children, usually caused by respiratory syncytial virus (RSV), adenovirus infections or influenza. Thrombocytosis is uncommon and its incidence and etiology are age-dependent[1]. It is rare in childhood, especially the primary form, which is of hemopoietic nature. More common is the secondary form or reactive thrombocytosis, which is often asymptomatic, transient, occurring during the course of a viral infectious illness, mainly respiratory, and it is often considered to be an acute phase reactant response to cytokines production during the infection. Other causes of reactive thrombocytosis include inflammation, anemia, hypoxia and some medications[2-6]. Cytokines [interleukins (IL)-6, IL-8, IL-11] and thrombopoietin have been implicated it its pathogenesis[7,8].
Thrombocytosis has only occasionally been reported in viral bronchiolitis with a prevalence ranging from as low as 8.4% up to 38.6%, with higher platelet counts observed in RSV positive infections[9,10]. This has led to the suggestion that RSV infection should strongly be suspected when thrombocytosis occurs in a child with a respiratory infection[11,12]. Although platelets play an important role in anti-microbial host defense, in the induction of inflammation and tissue repair, the significance of thrombocytosis during an infection is not fully clarified, as it may be caused by both disease aggressiveness and a higher capacity for host defense. For example, in adult patients hospitalized for community- acquired pneumonia, a high platelet count, is associated with a significant increase risk of mortality[13]. Likewise, in children with human immunodeficiency virus infection, thrombocytosis correlates with severe disease[14].
Reactive thrombocytosis in children is usually benign and does not cause thromboembolic or hemorrhagic complications, except if it occurs secondary to splenectomy or if there is underlying disease with additional thrombotic risk factors such as thalassemia[15,16] especially when complicated by cardiomyopathy, diabetes, hepatopathy and portal hypertension[17]. Neonatal thrombocytosis carries a higher thrombo-embolic risk in the presence of risk factors like maternal diabetes and antiphospholipid syndrome, septicemia, intrauterine growth retardation or in the presence of cyanotic cardiac malformation[18].
None of the few reports of thrombocytosis in children with bronchiolitis has looked at its association with risk factors, disease severity or thromboembolic complications. We therefore undertook this study to ascertain the prevalence of thrombocytosis in a cohort of children with bronchiolitis admitted to a general pediatric ward and analyze the risk factors associated with it. We also looked for thromboembolic complications and analyzed if elevated platelet count was associated with, and therefore a marker of bronchiolitis severity.
The study was a retrospective observational medical chart review of all infants aged two years or less who were hospitalized for bronchiolitis in the pediatric departments of Tawam hospital from 1st November 2008 to 30th June 2012. Indications for admission included worsening of the respiratory status, decreased oral intake, requirement for oxygen or parenteral therapy. The diagnosis of bronchiolitis was clinical and was made by the physician on admission based on the presence of an upper respiratory tract infection (either by history or by cough or rhinorrhea on physical examination), tachypnea, hypoxia, cough, subcostal or intercostal retractions, nasal flaring, grunting, with wheezing and/or crackles on auscultation. The management of admitted children was left to the discretion of the attending physician.
Excluded from the study were children with a bacterial co-infection, chronic disease, immune deficiencies, splenectomy, congenital cyanotic heart disease with polycythemia, presence of intravascular lines, treatment with medications associated with thrombocytosis, or with a personal or family history of thrombophilia.
Data for each infant were extracted through review of emergency department case files and admission notes. Demographic data (gender, age, weight at birth, and gestational age), duration of illness before admission and clinical features at the time of admission including basic observations were recorded. Maximal temperature was defined as the highest rectal temperature recorded in the emergency department or at the time of admission to the pediatric department and fever was defined as a temperature > 38 °C. Nasopharyngeal aspirates were obtained on admission and sent for enzyme-linked immunoassay rapid antigen detection of RSV (Tru RSV®, Meridian Bioscience, INC), and adenovirus, influenza A and B, parainfluenza 1, 2 and 3 viruses (LIGHT DIAGNOSTICS™ SimulFluor® Respiratory Screen, EMD Millipore). Platelet count was measured by CELL - DYN Sapphire (Abbot). Thrombocytosis was defined as a platelet count of more than 500 × 109/L. Counts of > 500 and ≤ 700 × 109/L were considered mild thrombocytosis, levels of > 700 and ≤ 900 × 109/L as moderate thrombocytosis, and levels of > 900 × 109/L as severe thrombocytosis[9]. For the purpose of the study only the first platelet count taken upon admission was used. Serum C-reactive protein (CRP) was measured with the Beckman Coulter DXB-800, with values < 8 mg/L defined as normal.
Clinical outcomes included disease severity as judged by duration of hospital stay, admission to pediatric intensive care unit (PICU), or death. They also included complications of thrombocytosis, including thromboembolic complications such as cerebrovascular accident, acute coronary syndrome, deep venous thrombosis, pulmonary embolus, mesenteric thrombosis and arterial thrombosis[19-21] and also hemorrhagic complications such as bleeding (spontaneous hemorrhage in the skin, mucous membranes, gastrointestinal, respiratory, or genitourinary tracts).
The prevalence of thrombocytosis was calculated with 95% confidence intervals (CI). Proportions were compared with the χ2 test, or the Fisher exact test if the number of observations was less than 5. The Student t-test was used to compare the means of Normally distributed variables between two groups. Analysis of variance was used to compare the means of normally distributed continuous variables amongst more than 2 groups, with Bonferroni adjustment for multiple comparisons. The odds and odds ratio of the association of thrombocytosis with the type and number of isolated viruses were calculated with 95%CI. For all statistical analyses, a 2-tailed P value was considered statistically significant if < 0.05.
Approval was granted by the Institutional Review Board (IRB 296/13) and the requirement for consent was waived as it was a retrospective study and patient anonymity was preserved.
During the study period there were 305 children admitted for acute bronchiolitis (n = 179 males, 59%). Their median age was 4.7 mo (mean ± SD 6.5 ± 0.2 mo, range 7 d to 1.9 years) and 49 (18%) were born preterm (< 38 completed weeks of gestation) with a median gestational age 40 of weeks (mean 39, range 23 to 42 wk) and a median birth weight of 3000 g (median 2.9, range 870 to 4600 g). The median duration of symptoms prior to admission was three days (mean ± SD 2.8 ± 1.2, range 0 to 6 d) and 203 children (68%) were febrile on presentation. Mild to moderate dehydration was present in 131 children (43%).
Virology studies were performed on all. Infection with a single virus occurred in 291 children (95%). RSV was isolated in 255 children (84%), adenovirus in 23 (7%) and influenza virus A or B in 13 (4%). Co-infection of RSV infection with adenovirus occurred in 8 (3%) and with influenza in six (2%).
The mean ± SD platelet count was 431 ± 141 × 109/L (median 421 × 109/L and range 51 to 1000 × 109/L). The platelet count was normal in 213 children (70%). Thrombocytosis occurred in 88 children (prevalence 29%; 95%CI 24% to 34%) and it was mild in 78 children (89%), moderate in 9 (10%) and severe in one (1%). The mean ± SD of blood white cell count were 3.4 ± 1.0 × 109/L and for serum CRP 1.4 ± 1.2 mg/L.
Forty children (1.3%) required admission to PICU: 25 (63%) required continuous positive airway pressure, mechanical ventilation was required in nine (22%) and six children (15%) only required additional oxygen administration. No death occurred. The mean ± SD duration of hospital stay was 4.2 ± 5.2 d (median 3, range 1 to 54 d). No thrombotic or hemorrhagic events were observed and no treatment for thrombocytosis was initiated for any of the affected children.
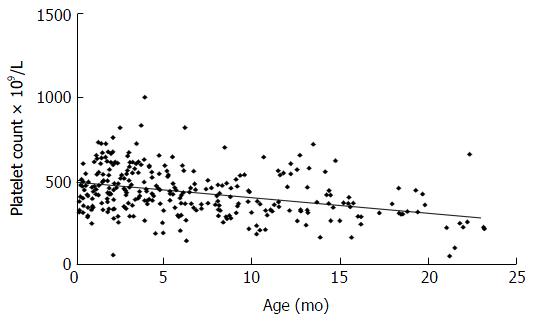
Thrombocytosis occurred significantly more commonly in younger infants (mean age 4.8 mo) (Table 1). The platelet level significantly declined with advancing age (Figure 1) with a slope of -8.9 in a linear regression model (P < 0.001) resulting in a decrease of approximately 9 × 109/L in the platelet count for each month of increase in age.
| Platelet count (× 109/L) n (%) or mean ± SD | P value | ||
| > 500 | < 500 | ||
| Children | 217 (71) | 88 (29) | |
| Age (mo) | 7.3 ± 5.8 | 4.8 ± 4.1 | < 0.0011 |
| Males | 132 (74) | 47 (26) | 0.22 |
| Born < 38 wk gestation | 32 (65) | 17 (35) | 0.32 |
| Duration of illness before admission (d) | 2.9 ± 1.2 | 2.7 ± 1.4 | 0.31 |
| Fever (> 38 °C) on admission | 148 (73) | 55 (27) | 0.32 |
| Blood white cell count (× 109/L) | 3.5 ± 1.1 | 3.2 ± 0.5 | 0.81 |
| Nasopharyngeal aspirate isolate | |||
| RSV | 189 (74) | 66 (26) | |
| Adenovirus | 13 (57) | 10 (43) | |
| Influenza | 6 (46) | 7 (54) | 0.09 |
| RSV + Adenovirus | 5 (62) | 3 (38) | |
| RSV + Influenza | 3 (50) | 3 (50) | |
| Serum CRP (mg/L) | 1.4 ± 1.3 | 1.5 ± 1.2 | 0.51 |
| Duration of hospitalization (d) | 4 ± 5.5 | 4.4 ± 4.2 | 0.61 |
| Admitted to intensive care | 25 (62) | 15 (37) | 0.22 |
There was no significant difference in platelet count between genders, history of prematurity, duration of illness prior to admission, temperature on admission, blood white blood cell count or serum CRP concentration (Table 1). No association with dehydration was observed (P = 0.06). The severity of thrombocytosis was not significantly associated with disease severity as judged by length of hospital stay or admission to the pediatric intensive care unit (Table 2).
| No. of virus isolated | Total | Thrombocytosis n (%) | Odds | OR (95%CI) | P value |
| One | 291 | 82 (28) | 0.4 | 1.0 (reference) | 0.2 |
| Two | 14 | 6 (43) | 0.75 | 1.9 (0.6-5.7) |
There was no significant difference in platelet count amongst the viruses identified in nasopharyngeal aspirates (Table 1), nor between infection with a single or more viruses (Table 3). Similarly, no significant difference in the prevalence of thrombocytosis (P = 0.5) was found between the children with RSV-positive infection (39%) and all those who were RSV-negative (41%).
The prevalence of thrombocytosis in children under the age of two years admitted for bronchiolitis was 29% (95%CI: 24%-34%). This contrasts sharply with a reported prevalence of 8% in a previous report[11]. The reason might be that the previous study included all respiratory infections, including measles infection, and not only bronchiolitis. In addition, as older children (up to nine years) were enrolled in that review, the lower prevalence of thrombocytosis is not surprising because it occurs less commonly in older children[1,22,23]. Another study reported a much higher prevalence (38%) of thrombocytosis in infants with bronchiolitis, but it enrolled only infants younger than four months where thrombocytosis is more prevalent[12]. We confirms the findings of previous reports that thrombocytosis in children with bronchiolitis is more common in the very young and declines steadily with age[22,23].
Although it is known that reactive thrombocytosis during childhood infections peaks during the second week of the illness[24], we deliberately chose to examine the platelet count on admission because the great majority of children with bronchiolitis are likely to be asymptomatic or discharged from hospital during the second week of the infection. We found no association of thrombocytosis with the duration of illness prior to admission, perhaps because platelet counts are often higher in patients with long duration of illness prior to admission[4] and children are usually admitted early in the course of bronchiolitis. We acknowledge, however, that firm conclusions regarding the timing of thrombocytosis in bronchiolitis cannot be drawn because only one platelet value was recorded in each patient and there were no serial measurements. Our findings corroborate previous reports, which showed that the secondary thrombocytosis is common and occurs early in RSV infection[11].
In our study, thrombocytosis occurred less commonly in RSV infections compared to other viruses. This contrasts with the results of a previous study which found it more common in RSV infections and even suggested that thrombocytosis should be considered as an early laboratory marker of RSV infection in childhood; however it included not only bronchiolitis, but all types of respiratory infections, including measles, and also enrolled much older children, up to 9 years of age[11,15]. Another report found a higher prevalence of thrombocytosis in RSV positive compared to RSV negative infections; however, the enrolled children were much younger, under four months of age, and no comparison with other viruses was performed[12]. Another possible explanation for the different results obtained in our study is that, unlike viral culture and polymerase chain reaction, the rapid antigen detection method that we have used does not have high sensitivity for the detection of viruses other than RSV and influenza.
Unlike earlier reports, thrombocytosis on admission was not associated with the severity of inflammation which we defined as the presence of fever, leukocytosis or elevated serum CRP level. It has already been established that, in the first week of acute infections, serum CRP, IL-6 and thrombopoeitin levels start to rise while the platelet count is still normal. The platelet count peaks later, in the second and third weeks when CRP and IL-6 levels are decreasing[8]. This, however, does not explain our findings because all admissions for bronchiolitis occurred within one week of the onset of symptoms, when fever and serum CRP are expected to be still elevated and the platelet count have not yet started to rise. The exact explanation for that discrepancy remains therefore elusive.
We did not find that disease severity, as defined by length of hospital stay or admission to the intensive care unit, was associated with the presence of thrombocytosis nor its severity. This is in contrast with a previous report that found thrombocytosis to predict mortality, but the cause for the difference is likely to be that, unlike our study in children with viral bronchiolitis, it had enrolled elderly adults with community-acquired pneumonia presumably of bacterial origin[19].
The absence of thromboembolic or hemorrhagic complications observed in our study confirms previous reports of reactive thrombocytosis[25,26]. In accordance with published guidelines, no treatment for thrombocytosis was initiated for any of the children in this study as none had intravascular lines, or congenital cyanotic heart disease associated with thrombosis, or medications associated with thrombocytosis, or a personal or a family history of thrombophilia[3,27].
The study has some limitations. The bronchiolitis score was not used as an index of disease severity, nor was the platelet count measured serially throughout the stay in hospital. Similarly, cytokines and thrombopoietin measurements were not performed. These limitations should be addressed in future studies.
In conclusion, secondary thrombocytosis is common in children under two years of age admitted with bronchiolitis, affecting 29% of them. It is not associated with a severe course for bronchiolitis or with thromboembolic complications.
Bronchiolitis is a common viral infection in young children, usually caused by respiratory syncytial virus (RSV), influenza or adenovirus infections. Secondary or reactive thrombocytosis may occur and is considered to be an acute phase reactant response to thrombopoietin or cytokines production during the infection [interleukins (IL)-6, IL-8, IL-11]. Its prevalence in bronchiolitis may range from 8.4% to 38.6%, with higher platelet counts observed in RSV positive infections. It usually does not result in thromboembolic or hemorrhagic complications.
None of the few reports of thrombocytosis in children with bronchiolitis has looked at its association with risk factors, disease severity or thromboembolic complications. The authors therefore undertook this study to ascertain the prevalence of thrombocytosis in a cohort of children with bronchiolitis admitted to a general pediatric ward and analyze the risk factors associated with it. They also looked for thromboembolic complications and analyzed if elevated platelet count was associated with, and therefore a marker of bronchiolitis severity.
In this retrospective observational study of platelet counts in 305 infants aged two years or less who were hospitalized for bronchiolitis, thrombocytosis (platelet count > 500 × 109/L) was frequent, occurring in 88 (29%; 95%CI: 24%-34%), more commonly in younger infants with the platelet count declining with age. There was no significant association with the duration of illness, temperature on admission, white blood cell count, serum C-reactive protein concentration, length of hospital stay, admission to the intensive care unit, death, thrombotic or hemorrhagic complications.
Thrombocytosis is common in children under two years of age admitted with bronchiolitis. It is not associated with disease severity or thromboembolic complications.
Thrombocytosis is defined as a platelet count of more than 500 × 109/L. Counts of > 500 and ≤ 700 × 109/L are considered mild thrombocytosis, levels of > 700 and ≤ 900 × 109/L as moderate thrombocytosis, and levels of > 900 × 109/L as severe thrombocytosis.
The article is well written and interesting.
Manuscript source: Unsolicited manuscript
Specialty type: Pediatrics
Country of origin: United Arab Emirates
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Urganci N, Trovato GM S- Editor: Kong JX L- Editor: A E- Editor: Li D
| 1. | Matsubara K, Fukaya T, Nigami H, Harigaya H, Hirata T, Nozaki H, Baba K. Age-dependent changes in the incidence and etiology of childhood thrombocytosis. Acta Haematol. 2004;111:132-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Dame C, Sutor AH. Primary and secondary thrombocytosis in childhood. Br J Haematol. 2005;129:165-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Harrison CN, Bareford D, Butt N, Campbell P, Conneally E, Drummond M, Erber W, Everington T, Green AR, Hall GW. Guideline for investigation and management of adults and children presenting with a thrombocytosis. Br J Haematol. 2010;149:352-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 208] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 4. | Mantadakis E, Tsalkidis A, Chatzimichael A. Thrombocytosis in childhood. Indian Pediatr. 2008;45:669-677. [PubMed] |
| 5. | Schafer AI. Thrombocytosis. N Engl J Med. 2004;350:1211-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 258] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | Sutor AH. Thrombocytosis in childhood. Semin Thromb Hemost. 1995;21:330-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 7. | Matsubara K, Baba K, Nigami H, Harigaya H, Ishiguro A, Kato T, Miyazaki H. Early elevation of serum thrombopoietin levels and subsequent thrombocytosis in healthy preterm infants. Br J Haematol. 2001;115:963-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Ishiguro A, Suzuki Y, Mito M, Shimbo T, Matsubara K, Kato T, Miyazaki H. Elevation of serum thrombopoietin precedes thrombocytosis in acute infections. Br J Haematol. 2002;116:612-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Akaboshi I, Fugita K, Abe A, Tanaka T. An unusual case of thrombocytosis associated with concurrent cytomegalovirus and respiratory syncytial virus infection in an immunocompetent infant: possible roles of thrombopoietin and interleukin-6. J Infect. 2005;51:e97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Mammas I, Koutsaftiki C, Tapaki-Papadopoulou G, Myriokefalitakis N. Respiratory syncytial virus (RSV) bronchiolitis and excessive thrombocytosis. Acta Paediatr. 2010;99:489-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Kubota M, Maeda H, Yoshimoto J, Kobayashi K, Usami I, Yamaoka K. Thrombocytosis at an early stage of respiratory tract viral infection. Acta Paediatr. 2005;94:364-366. [PubMed] |
| 12. | Bilavsky E, Yarden-Bilavsky H, Shouval DS, Fisch N, Garty BZ, Ashkenazi S, Amir J. Respiratory syncytial virus-positive bronchiolitis in hospitalized infants is associated with thrombocytosis. Isr Med Assoc J. 2010;12:39-41. [PubMed] |
| 13. | Mirsaeidi M, Peyrani P, Aliberti S, Filardo G, Bordon J, Blasi F, Ramirez JA. Thrombocytopenia and thrombocytosis at time of hospitalization predict mortality in patients with community-acquired pneumonia. Chest. 2010;137:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 95] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Ellaurie M. Thrombocytosis in pediatric HIV infection. Clin Pediatr (Phila). 2004;43:627-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Shebl SS, el-Sharkawy HM, el-Fadaly NH. Haemostatic disorders in nonsplenectomized and splenectomized thalassaemic children. East Mediterr Health J. 1999;5:1171-1177. [PubMed] |
| 16. | Sutor AH. Screening children with thrombosis for thrombophilic proteins. Cui bono? J Thromb Haemost. 2003;1:886-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Borgna Pignatti C, Carnelli V, Caruso V, Dore F, De Mattia D, Di Palma A, Di Gregorio F, Romeo MA, Longhi R, Mangiagli A. Thromboembolic events in beta thalassemia major: an Italian multicenter study. Acta Haematol. 1998;99:76-79. [PubMed] |
| 18. | Edstrom CS, Christensen RD. Evaluation and treatment of thrombosis in the neonatal intensive care unit. Clin Perinatol. 2000;27:623-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Harrison CN, Gale RE, Machin SJ, Linch DC. A large proportion of patients with a diagnosis of essential thrombocythemia do not have a clonal disorder and may be at lower risk of thrombotic complications. Blood. 1999;93:417-424. [PubMed] |
| 20. | Pearson TC. The risk of thrombosis in essential thrombocythemia and polycythemia vera. Semin Oncol. 2002;29:16-21. [PubMed] |
| 21. | Vannucchi AM, Barbui T. Thrombocytosis and thrombosis. Hematology Am Soc Hematol Educ Program. 2007;363-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Vora AJ, Lilleyman JS. Secondary thrombocytosis. Arch Dis Child. 1993;68:88-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Yohannan MD, Higgy KE, al-Mashhadani SA, Santhosh-Kumar CR. Thrombocytosis. Etiologic analysis of 663 patients. Clin Pediatr (Phila). 1994;33:340-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Cecinati V, Brescia L, Esposito S. Thrombocytosis and infections in childhood. Pediatr Infect Dis J. 2012;31:80-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Chan KW, Kaikov Y, Wadsworth LD. Thrombocytosis in childhood: a survey of 94 patients. Pediatrics. 1989;84:1064-1067. [PubMed] |
| 26. | Griesshammer M, Bangerter M, Sauer T, Wennauer R, Bergmann L, Heimpel H. Aetiology and clinical significance of thrombocytosis: analysis of 732 patients with an elevated platelet count. J Intern Med. 1999;245:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 183] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 27. | Denton A, Davis P. Extreme thrombocytosis in admissions to paediatric intensive care: no requirement for treatment. Arch Dis Child. 2007;92:515-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |