Revised: October 6, 2013
Accepted: November 15, 2013
Published online: February 6, 2014
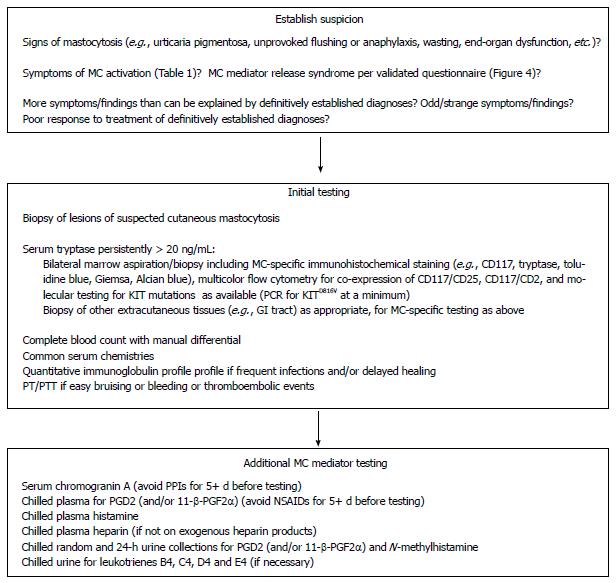
As recognition of mast cell (MC) involvement in a range of chronic inflammatory disorders has increased, diagnosticians’ suspicions of MC activation disease (MCAD) in their chronically mysteriously inflamed patients have similarly increased. It is now understood that the various forms of systemic mastocytosis - diseases of inappropriate activation and proliferation of MCs seemingly driven by a small set of rare, usually constitutively activating mutations in assorted MC regulatory elements - comprise merely the tip of the MCAD iceberg, whereas the far larger and far more clinically heterogeneous (and thus more difficult to recognize) bulk of the iceberg consists of assorted forms of MC activation syndrome (MCAS) which manifest little to no abnormal MC proliferation and may originate from a far more heterogeneous set of MC mutations. It is reasonable to suspect MCAD when symptoms and signs of MC activation are present and no other diagnosis better accounting for the full range of findings is present. Initial laboratory assessment should include not only routine blood counts and serum chemistries but also a serum total tryptase level, which helps direct further evaluation for mastocytosis vs MCAS. Appropriate tissue examinations are needed to diagnose mastocytosis, while elevated levels of relatively specific mast cell mediators are sought to support diagnosis of MCAS. Whether assessing for mastocytosis or MCAS, testing is fraught with potential pitfalls which can easily yield false negatives leading to erroneous rejection of diagnostic consideration of MCAD in spite of a clinical history highly consistent with MCAD. Efforts at accurate diagnosis of MCAD are worthwhile, as many patients then respond well to appropriately directed therapeutic efforts.
Core tip: Mast cell activation disease (MCAD) is characterized by accumulation of genetically altered mast cells and/or abnormal release of these cells’ mediators, affecting functions in potentially every organ system, often without causing abnormalities in routine laboratory or radiologic testing. Recent data suggest a high prevalence of MCAD. Thus, MCAD should be considered routinely in the differential diagnosis of patients with chronic multisystem polymorbidity of a generally inflammatory theme or patients in whom established diagnoses do not well account for the patient’s presentation of symptoms consistent with mast cell mediator release. Mediator testing can be challenging but typically is manageable. Diagnostic efforts are worthwhile, as diagnosis often leads to effective therapy.
- Citation: Afrin LB, Molderings GJ. A concise, practical guide to diagnostic assessment for mast cell activation disease. World J Hematol 2014; 3(1): 1-17
- URL: https://www.wjgnet.com/2218-6204/full/v3/i1/1.htm
- DOI: https://dx.doi.org/10.5315/wjh.v3.i1.1
Of hematopoietic origin, mast cells (MCs) are found in all human tissues, especially at the environmental interfaces and perivascular/perineural sites[1]. They serve largely as sentinels of environmental change and bodily insults and respond by releasing large and variable assortments of molecular mediators which directly and indirectly influence behavior in other local and distant cells and tissues to respond to changes and insults so as to maintain, or restore, homeostasis.
MCs and the related rare cutaneous disease urticaria pigmentosa (UP) were first discovered in the latter half of the 19th century[2,3], and the existence of seemingly even rarer systemic MC disease first became apparent in the middle of the 20th century[4,5]. For several decades it was thought that virtually all MC diseases were neoplastic, with symptoms resulting principally from accompanying inappropriate mediator release. Nearly a quarter century ago, the recurring somatic D816V mutation was discovered[6] in the dominant MC regulatory element, transmembrane tyrosine kinase receptor KIT[7], in a high proportion of patients with systemic mastocytosis (SM)[8,9]. This constitutively activating mutation has since been found to drive many features of SM including aberrant aggregation and spindled morphology of MCs in SM, tryptase and histamine overexpression, and aberrant MC surface co-expression of CD25[10-12]. Several other KIT mutations, also quite rare, have since been found in other cases of SM, mostly in KIT’s kinase domain 1 at or near codon 816 or in the juxtamembrane region of KIT[11]. Recently, evidence has emerged that the KITD816V mutation induces the above-mentioned immunohistochemical and morphological changes in affected MCs but seems not to be solely responsible for the clinical symptoms of the MC disease[13,14]. This finding fits well with previous reports in healthy people bearing the KITD816V mutation in their peripheral blood leukocytes[15].
Around the same time as the discovery of KITD816V, though, the notion was first advanced that some portion of MC disease might be due to inappropriate mediator release with little to no accompanying MC proliferation[16]. This theory appeared validated when the first recognized cases of what is now called MC activation syndrome (MCAS) were published recently[17,18]. Although not yet independently confirmed, there soon followed provocative, repeated findings from one group of a very wide array of (presumably mostly constitutively activating) mutations scattered across all domains of KIT in small cohorts of MCAS patients[19,20]. Many of these patients appeared to bear multiple mutations in MC KIT, with no apparent recurring patterns. Similar mutational complexity has been found, too, across the spectrum of chronic myeloproliferative neoplasms (MPNs) within which the MC disorders reside[21], and in advanced mastocytosis itself[22].
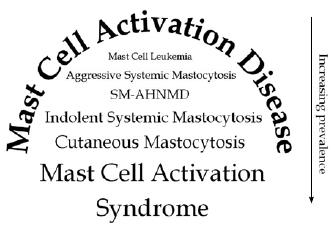
In recognition of the fact that all MC disease is, first and foremost, disease of inappropriate MC activation, Akin et al[23] have proposed a new umbrella term of MC activation disease (MCAD) to describe the full spectrum of MC disease (Figure 1). MCAS is estimated to be more prevalent[13,24], but also more difficult to recognize, than other diseases traditionally ascribed to MC dysfunction. It also has been proposed that the various systemic MCAD variants and clinical phenotypes represent not distinct disease entities but rather varying presentations of a common generic root process of mast cell dysfunction[13]. The various forms of mastocytosis (principally cutaneous and systemic) may be the tip of a proverbial MCAD iceberg, fairly readily recognizable (in spite of their rarity) because of their defined unique immunohistochemical and relatively uniform clinical presentations, while the bulk of the iceberg - hidden below the waterline of easy clinical recognizability - may be a far larger, and far more heterogeneous, collection of variants of MCAS, some specifically named (e.g., idiopathic anaphylaxis[18], cryopyrin-associated periodic syndrome[25]) but most not[23,26]. It seems logical that marked mutational heterogeneity would drive the marked heterogeneity of aberrant mediator expression and clinical presentation which are observed in MCAD and which can easily confound the diagnostician. For example, although MCAD can readily impact any or all systems in the body, cases have been described of MCAS causing hematologic presentations as diverse as pure red cell aplasia[27], erythrocytosis[28], and agranulocytosis[29].
Limited familial studies performed to date interestingly show high familial loading of MCAD despite a typical absence of germline mutations[24]; instead, most of the few families carefully studied show distinct sets of somatic mutations in the affected members with correspondingly varying clinical presentations. Clinical correlation suggests acquisition of the initial disease-causing mutations occurs relatively early in life, but additional mutations may develop in subclones over time. Efforts to reconcile the apparent dichotomy of high familial loading of MCAD with absence of apparent germline genetic mutations in affected families have led to thoughts that certain epigenetic alterations (GJM, unpublished data) may confer a state of genetic fragility which, upon interaction with varying biochemical milieus induced by assorted stressors (e.g., infection), in turn induces MCAD-causing mutations in MC regulatory elements.
Diagnosticians willing to pursue the possibility of MCAD in their patients whose chronic multisystem polymorbidity (often, but not always, of a generally inflammatory theme) has defied extensive prior diagnostic efforts (typically focused on subspecialty-oriented symptom subsets rather than broad multisystem considerations) currently face many challenges including controversies in precise diagnostic criteria (particularly for MCAS), uncertainty regarding the utility of various diagnostic tests, and difficulties properly managing specimens for such testing. Whether assessing for mastocytosis or MCAS, testing is fraught with potential pitfalls which can easily yield erroneous conclusions that MCAD is not present and thereby potentially add yet much more time and cost to the very long and expensive path most patients with MCAD (particularly MCAS) require to establish diagnosis, let alone effective therapy. We describe here in detail our thoughts regarding current proposals for diagnostic criteria for MCAD and our approach to diagnostic testing for MCAD, i.e., both mastocytosis and MCAS.
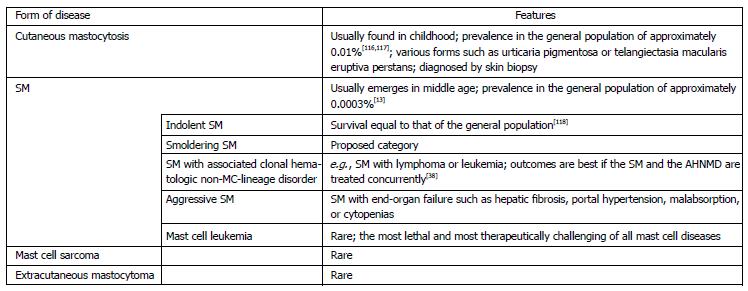
Classification systems and diagnostic criteria for mastocytosis were first proposed in the 1980s[30,31]. Since 2001 the World Health Organization (WHO) consensus criteria have guided classification and diagnosis globally[32]. The latest revision of these criteria, published in 2008[33], divide mastocytosis broadly into cutaneous and systemic forms as well as the even rarer solid MC tumors of MC sarcoma and extracutaneous mastocytoma (Figure 2).
The WHO 2008 consensus diagnostic criteria for SM are shown in Figure 2. Given that it is now understood that MC KIT codon 816 mutations (a minor criterion) drive MC aggregation (a major criterion) and certain other minor criteria including MC spindling, tryptase overexpression, and CD25 co-expression, reorganization of the WHO diagnostic criteria for SM may be in order.
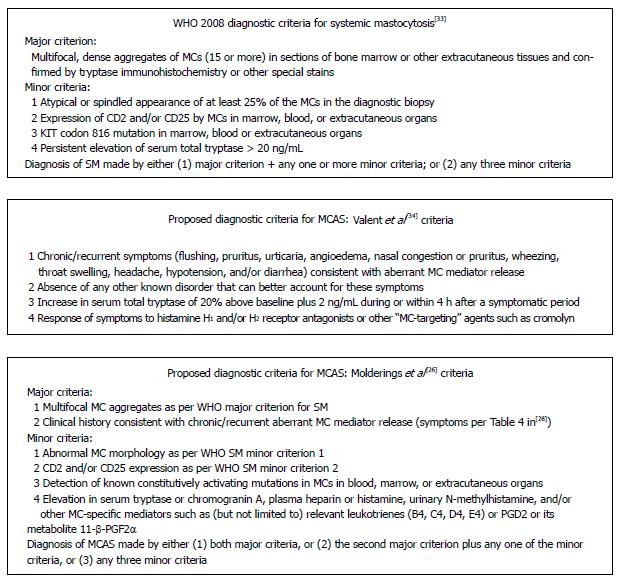
Recognition of the need for an alternative, MCAS-like diagnosis came about in part because of the discovery of patients whose clinical presentation was highly consistent with SM but who did not satisfy the major SM diagnostic criterion and only satisfied one or two of the minor criteria. In particular, many patients significantly affected by aberrant MC activation previously have been denied diagnosis of, and treatment for, MCAD because of a serum tryptase level < 20 ng/mL. Presently there are two principal proposals for diagnostic criteria for MCAS (Figure 3). Potential problems with the Valent et al[34] criteria include (1) non-recognition of many of the symptoms[28] that can result from MC activation; (2) lack of published validation that the described tryptase increase reliably distinguishes ordinary baseline fluctuation of tryptase from fluctuation induced by aberrant MC activation; (3) practical difficulties in providing/obtaining a specimen for serum total tryptase within 4 h of onset of an exacerbation of symptoms; and (4) practical difficulties in many patients in finding - in such a heterogeneous disease - MC-targeting agents that can effect at least partial response. Thus, for example, patients whose aberrant MC activation causes substantial muscle/joint/bone aching, constipation and abdominal pain, paresthesias, adenitis, and cognitive dysfunction but not the symptoms listed in these criteria would not qualify for the diagnosis. Similarly, a rise in serum tryptase (whose normal range typically is approximately 0.5 to 11 ng/mL) from 2.0 ng/mL to 4.2 ng/mL would be considered “20% + 2 ng/mL” evidence of aberrant MC activation, but a rise to 4.1 ng/mL would not. Furthermore, patients often are sufficiently disabled during a flare of symptoms that they cannot easily get to a medical center, and those who do travel to an urgent care facility or emergency department often encounter providers resistant to pursuing tests not needed for immediate care of the presenting symptoms. Such resistance often persists even when the patient presents a prescription from a MC disease specialist specifically requesting MC mediator testing at times of such flares. Finally, in concert with the observed marked heterogeneity of the clinical presentation of MCAS (perhaps due to underlying marked mutational heterogeneity), some MCAS patients benefit little from the first few or several MC-targeting therapies tried, risking premature rejection of the diagnosis.
A potential problem with the Molderings et al[26] criteria for diagnosis of MCAS is the lack of mention of excluding other diagnoses (including mastocytosis) better accounting for the full range of findings in the patient, but such an exclusion would seem to be implicit. In practice, this scheme most often leads to diagnosis of MCAS by pairing of the second major criterion with the last of the minor criteria, and it appears to permit applying the diagnosis of MCAS - and therefore also pursuing therapy for MCAS - in a wider population of otherwise mysteriously chronically multi systemically ill patients, possibly increasing risk of misdiagnosis.
There have been no studies of the diagnostic accuracy or efficiency of these two diagnostic schemes. Also, at present there are no “gold standards” distinguishing levels of MC mediators seen in normal MC activation/reaction from levels seen in aberrant MC activation. We believe such distinctions will be difficult to develop, therefore also making it difficult to perform comparative studies of accuracy of different diagnostic schemes. Routine use of MC whole exome/genome sequencing and mutational analysis in patients with clinical histories suspicious for MCAD may become the most efficient route to definitively diagnosing MCAD, but currently the specific polymerase chain reaction (PCR) assay for KITD816V (found often in SM but seldom in MCAS) is the only mutational analysis routinely available in most clinics. At present, though, it is worth noting that in view of the demonstrated great mutational complexity across the MPN spectrum, it may be premature to declare any given MCAS patient’s disease as “non-clonal” based on negative clonality evaluations less complete than whole KIT sequencing. The term “uncertain clonality” may be more accurate.
Given the very limited mutational and clonality testing for MCAD presently available in most clinics, laboratory evaluation for MCAS will continue, at least for the near future, to depend far more on demonstration of elevated levels of MC-specific mediators.
Accurate diagnosis of any condition begins with inclusion of the correct diagnosis in the considered differential diagnosis. Despite its rarity, development of clinical suspicion for mastocytosis is somewhat easier than for MCAS given the often flagrant nature of the clinical presentation, either with classic appearance of UP or telangiectasia macularis eruptiva perstans (TMEP) in cutaneous mastocytosis or with classic appearance of recurrent unprovoked flushing and/or anaphylaxis in systemic mastocytosis.
Initial suspicion of MCAS is more challenging due to its heterogeneity and, often, lack of flagrant acute presentation. Diagnosticians need to be cognizant that MCAD can affect every system, usually affects multiple systems, and usually manifests symptoms in a subacute or chronic waxing/waning or episodic fashion, though episodes also can arise acutely, i.e., the so-called “flares” or “attacks” or “spells” that many patients have of one symptom set or another. Many symptoms often are categorized as inflammatory in nature (e.g., pain, diarrhea), though non-inflammatory symptoms (or at least symptoms not traditionally thought to be inflammatory in nature) are prevalent, too (e.g., fatigue, paresthesias).
Another clue that MCAD may be present is simply the oddity or unexpectedness of certain clinical events or findings in the patient. Given the very large array of mediators normally produced and released by the MC[35] and therefore potentially abnormally expressed in MCAD, with each mediator causing a unique, and usually wide, range of direct and indirect, local and distant effects, the potential for the disease to manifest “odd”, “weird”, “strange”, “inexplicable” and “bizarre” clinical presentations is substantial. Such descriptors often are found throughout MCAD patients’ charts for years prior to diagnosis. Especially when seen in the context of pre-existing chronic multisystem inflammatory illness, the appearance in the patient of “unusual” new clinical phenomena should provoke consideration of MCAD. (Of course, the diagnostician is abetted in such recognition by remaining abreast of the steadily enlarging scope of the chronic inflammatory diseases. For example, diabetes mellitus type 2, obesity, and atherosclerotic vascular disease have been recognized as chronic inflammatory diseases only relatively recently.)
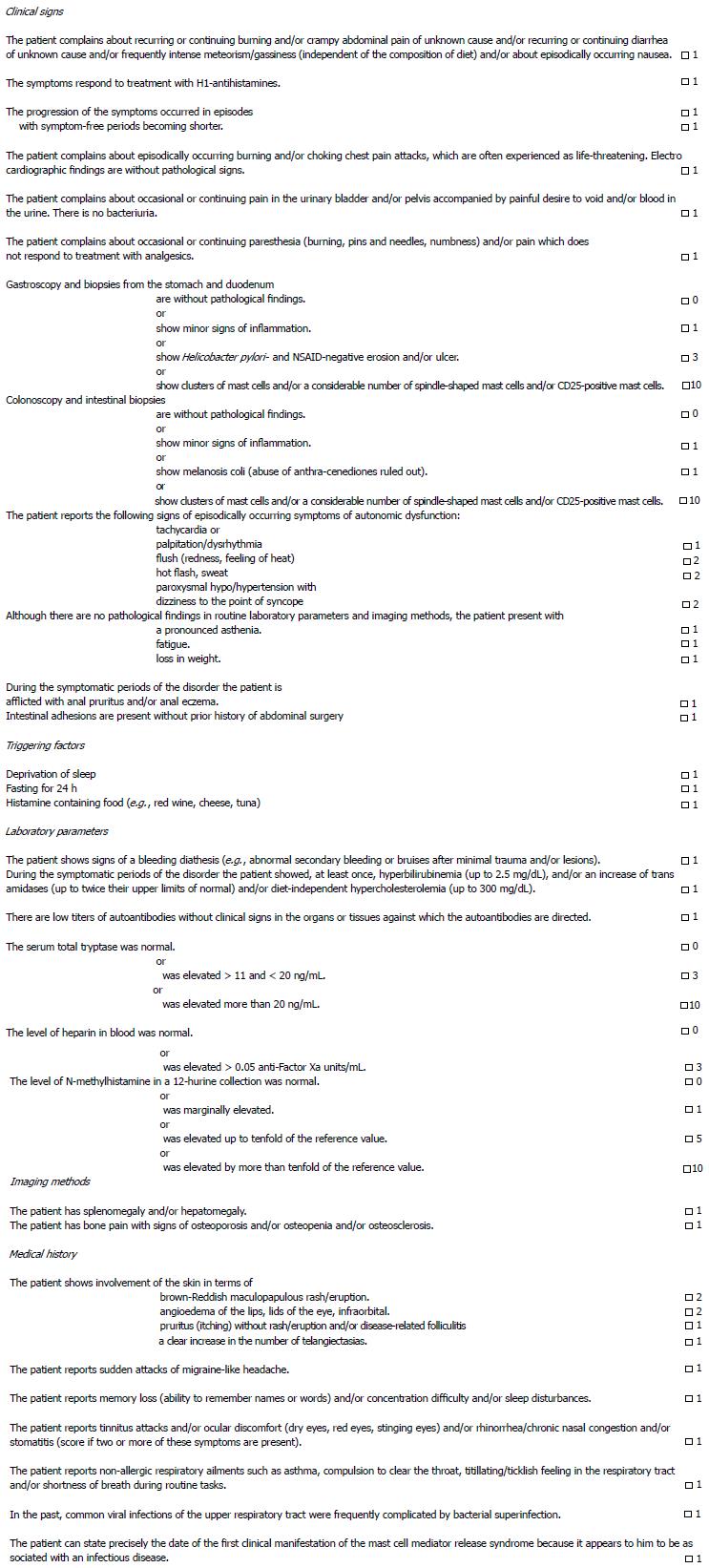
By the time MCAD is diagnosed, most patients have seen many providers, have undergone extensive testing (often frustratingly yielding normal or non-specifically/minimally abnormal results), and have been assigned many diagnoses (often with less than a full measure of confidence) which explain assorted subsets of findings but do not well account for the full range of findings, including chronicity often dating back decades. Treatments for these preliminary diagnoses sometimes help somewhat but often do not help at all, further perplexing the diagnostician. It is reasonable to suspect MCAD when at least several symptoms and signs of MC activation are present (Table 1)[26,28,36,37] and no other diagnosis better accounting for the full range of findings is present. In particular, presence of a definitively diagnosed condition (e.g., lymphoma) which does not well account for all symptoms and findings (e.g., presyncope, erythrocytosis, etc.), or poor response of a definitively diagnosed condition to standard treatment for that condition, should raise suspicion for the presence of either a significant independent diagnosis or an alternative underlying ailment better accounting for the full range of symptoms and findings. In such cases, definitive diagnosis of a comorbid (and potentially even underlying) MCAD permits dual-directed therapy[38] which may lead to improved outcomes. Standardized detection of a MC mediator release syndrome can be achieved by a validated questionnaire (Figure 4). Although routine complete blood counts (CBCs) and metabolic panels often are confoundingly normal in MCAD patients, it is also the case that abnormalities in these and other common blood tests in these patients are commonly seen and are typically modest and stable. Frequent, though not necessarily constant, relative or absolute monocytosis, eosinophilia, basophilia, and/or reactive lymphocytosis, typically to just modest degrees, can be seen along with similar patterns of abnormality in routine chemistries such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (AP) (LBA and GJM, unpublished data), hyperbilirubinemia, and diet-independent hypercholesterolemia and hypertriglyceridemia[39]. Viewed in encounter-specific isolation, such abnormalities often raise no concern and garner no further attention, but trend analysis made easy by electronic medical record systems can quickly highlight the persistence of these abnormalities and permit expansion of the considered differential diagnosis to include entities such as MCAD which can account for these additional findings.
| System | Potential manifestations of MCAD (most are chronic, low-grade; some are persistent, but many are either episodic or fluctuant) |
| Constitutional | Fatigue, malaise, asthenia, “chronic fatigue syndrome”, subjective and/or objective hyperthermia and/or hypothermia, “sense of feeling cold much of the time”, sweats/diaphoresis (not always nocturnal), flushing, plethora or pallor, increased or decreased appetite, early satiety, weight gain or loss, pruritus, chemical and/or physical environmental sensitivities (often odd) |
| Dermatologic/ integument | Rashes and lesions of many sorts (classic urticaria pigmentosa, “freckles”, telangiectatic/angiomatous lesions, xerosis, warts, tags, folliculitis, ulcers, dyshidrotic eczema, diffusely migratory but sometimes focally persistent patchy macular erythema), pruritus (often diffusely migratory, sometimes aquagenic), flushing, angioedema, striae, dermatographism, hair thinning and alopecia, onychodystrophy (brittle nails, longitudinal ridges), poor healing |
| Ophthalmologic | Irritated eyes, increased or decreased lacrimation, suffusion, conjunctivitis, episodic difficulty focusing, lid tremor/tic (blepharospasm), solar sensitivity, infectious or sterile inflammation |
| Otologic/osmic | Infectious or sterile otitis externa and/or media, hearing loss or hyperacusis, tinnitus, otosclerosis, dysosmia, coryza, congestion |
| Oral/oropharyngeal | Pain or irritation (sometimes “burning”), leukoplakia, fibrosis, lichen planus, ulcers, sores, angioedema, dental decay, dysgeusia, throat tickle/discomfort/irritation/pain, post-nasal drip |
| Lymphatic | Adenopathy, usually sub-pathologic and often waxing/waning in size, sometimes asymptomatic but not uncommonly tender, sometimes focal, sometimes migratory, pathology usually shows reactive lymphocytosis or sometimes an atypical non-specific lymphoproliferative disorder; left upper quadrant discomfort (likely from release of mediators from splenic mast cells with or without detectable splenomegaly) |
| Pulmonary | Rhinitis, sinusitis, pharyngitis, laryngitis, bronchitis, pneumonitis (often confused with infectious pneumonia), cough, dyspnea (often low-grade, inconstant, “I just can’t catch a deep breath” despite normal pulmonary function tests), wheezing, obstructive sleep apnea, pulmonary hypertension |
| Cardiovascular | Presyncope (lightheadedness, weakness, dizziness, vertigo) and/or syncope (patients may have been diagnosed with postural orthostatic tachycardia syndrome or neurocardiogenic syncope), hypertension and/or hypotension, palpitations, dysrhythmias, chest discomfort or pain (usually non-anginal in character), coronary and peripheral arterial atherosclerosis/spasm/infarction, idiopathic acute or chronic heart failure (e.g., takotsubo), aneurysms, hemorrhoids, varicosities, aberrant angiogenesis (hemangiomas, arteriovenous malformations, telangiectasias), migratory edema (often non-dependent and with normal cardiac and renal function) |
| Gastrointestinal | Aerophagia, angioedema in any segment of the luminal tract, dysphagia (often proximal, possibly due to pharyngeal angioedema), bloating/gas, pain/inflammation (often migratory) in one or more segments of the luminal tract (from esophagitis to proctitis) and/or one or more solid organs (e.g., hepatitis, pancreatitis), queasiness, nausea, vomiting (sometimes “cyclical”), diarrhea and/or constipation (often alternating), malabsorption (more often selective micronutrient malabsorption than general protein-calorie malabsorption), ascites either from portal hypertension and/or peritoneal serositis; gastroesophageal reflux disease (often “treatment-refractory”) and inflammatory/irritable bowel syndrome are common pre-existing diagnoses |
| Genitourinary | Inflammation (often migratory) in one or more segments of the luminal tracts (ureteritis, cystitis, urethritis, vaginitis, vestibulitis) and/or one or more solid organs (e.g., nephritis, prostatitis), chronic kidney disease, endometriosis, chronic low back pain or flank pain or abdominal pain, hydronephrosis (likely from ureteral angioedema), infertility, erectile dysfunction, decreased libido; in the appropriate setting of multisystem morbidity, miscarriages should prompt consideration of antiphospholipid antibody syndrome potentially due to MCAD |
| Musculoskeletal | Clinical myositis, often diffusely migratory (fibromyalgia is a common pre-existing diagnosis), subclinical myositis (i.e., asymptomatic elevated creatine kinase not otherwise explained), arthritis (typically migratory), joint laxity/hypermobility (patients may have been diagnosed with Ehlers-Danlos Syndrome Type III), osteoporosis/osteopenia, osteosclerosis, sometimes mixed osteoporosis/osteopenia/osteosclerosis; MCAD-driven musculoskeletal pain not uncommonly is poorly responsive to non-steroidal anti-inflammatory drugs and narcotics |
| Neurologic | Headache (esp. migraine), presyncope and/or syncope, peripheral (usually distal) sensory and/or motor neuropathies including paresthesias, tics, tremors (typically resting), chronic inflammatory demyelinating polyneuropathy, seizure disorders (can be “treatment-refractory”), pseudoseizures, dysautonomia |
| Psychiatric | Mood disturbances (e.g., anger, depression), bipolar affective disorder, attention deficit-hyperactivity disorder, post-traumatic stress disorder, anxiety and panic, psychoses, memory difficulties, word-finding difficulties, other cognitive dysfunction, wide variety of sleep disruptions |
| Endocrinologic/meta-bolic | Abnormal electrolytes (including magnesium) and liver function tests, delayed puberty, dysmenorrhea, endometriosis, osteosclerosis and/or osteoporosis, hypothyroidism, hyperthyroidism, dyslipidemia, hyperferritinemia, selective vitamin and/or other micronutrient deficiencies, weight change, possibly diabetes mellitus |
| Hematologic/coagu-lopathic | Polycythemia or anemia (may be macrocytic, normocytic, or microcytic), leukocytosis or leukopenia, chronic (usually mild) monocytosis or eosinophilia or basophilia, thrombocytosis or thrombocytopenia, arterial and/or venous thromboembolic disease, “easy” bruising/bleeding; in mast cell activation syndrome the marrow usually does not show increased (or even flow-cytometrically aberrant) mast cells; marrow histology often read as normal or as unspecified myelodysplastic/myeloproliferative syndrome; standard cytogenetic studies are almost always normal or show culture failure |
| Immunologic | Type I, II, III and IV hypersensitivity reactions, increased risk for malignancy, autoimmunity, impaired healing, increased susceptibility to infection, elevated or decreased levels of one or more isotypes of immunoglobulin; modest monoclonal gammopathy of undetermined significance not uncommon |
It is now understood that the serum total tryptase level much more reflects the total body MC load than the total body MC activation state[40-42]. As such, serum tryptase is expected to be elevated in mastocytosis but usually is elevated little to none in MCAS. “Spillover” into blood circulation of tryptase and other MC mediators initially released in the tissues can be influenced by many factors. Hence, a normal value for a mediator in blood or other bodily fluid does not rule out its unregulated release in tissue. In fact, about 20% of SM patients present with serum tryptase < 20 ng/mL[37,43,44], but such patients rarely harbor the more advanced forms of SM [aggressive SM (ASM) and MC leukemia (MCL)] which require therapeutic approaches different from those used for the more common indolent SM and MCAS. Marrow aspiration/biopsy, an uncomfortable procedure for some patients, is warranted in cases of suspected mastocytosis but seldom yields diagnostic findings in cases of MCAS not already manifesting significant hematologic abnormalities (LBA and GJM, unpublished data). Therefore, a serum tryptase persistently elevated to > 20 ng/mL in two or more specimens facilitates an initial decision whether to evaluate further for SM with biopsies as appropriate including at least marrow, and possibly also skin, upper and lower gastrointestinal (GI) tract mucosa, and potentially other tissues, especially those at the environmental interfaces. An initial serum tryptase < 20 ng/mL makes SM (especially ASM and MCL) much less likely, and since the prognosis of, and therapeutic approach toward, indolent SM and MCAS are presently indistinguishable, there appear to be no adverse consequences if the clinician initially misdiagnoses the uncommon low-tryptase SM as MCAS.
Tryptase has been well established as a highly specific MC mediator[45]. Its biology is complex; many isoforms with different behaviors and functions have been elucidated[46]. It is heat-labile[47,48] and has a relatively short half-life in vivo (from 6-8 min in healthy subjects to 1.5-2.3 h in patients with hypersensitivity reactions), longer (approximately 4 d) in separated serum[34,49]. The WHO 2008 diagnostic criteria for mastocytosis call only for the measurement of total serum tryptase, setting a threshold of 20 ng/mL as the minimum level consistent with a diagnosis of SM[33]. It is unclear whether measurement of specific isoforms of tryptase would be beneficial in diagnosing MCAD in any form, and thus at present only the measurement of total serum tryptase can be recommended in the evaluation of a patient suspected of having MCAD. Although the serum total tryptase usually is not elevated in MCAS[20,26], an elevated level (though almost always < 20 ng/mL) can be found in a minority of MCAS patients, and any elevation at all can help buttress a diagnostician’s suspicions of the involvement of MC activation in the patient’s illness.
If the serum tryptase persistently exceeds 20 ng/mL, or if other clinical features of the presentation are characteristic for SM (e.g., initial onset of symptoms in middle age, MCs observed in the peripheral blood smear, etc.), then further evaluation for SM is warranted. Marrow aspiration/biopsy is a standard part of such evaluation, and given both the patchy distribution of the disease in involved tissues and the observation that unilateral marrow biopsies are non-diagnostic in one-sixth of patients ultimately diagnosed with SM[50], bilateral aspirations/biopsies are preferred. Core biopsies should undergo routine staining as well as MC-targeted immuno/histochemical staining (e.g., CD117, CD25, CD2, tryptase, Giemsa, toluidine blue, Alcian blue, etc.). There is no particular subset of these stains which has been established as a standard initial assessment. It has been proposed that CD30, too, be routinely examined when assessing for MCAD[38]. Also, CD68 - more classically associated with macrophages - can be displayed by MCs and thus may be useful in diagnosing MCAD[51]. All of the above having been said, MCs express surface CD117 (the extracellular portion of c-kit) roughly an order of magnitude more brightly than any other CD117-expressing cell, so often only CD117 staining is needed to estimate MC density and to characterize aggregation. Each aspirate should be sent for standard cytogenetic analysis as well as multi-color flow cytometric assessment for co-expression of cell-surface doublets CD117/CD25 and CD117/CD2; occasionally even the triplet of CD117/CD25/CD2 is seen[52]. These flow cytometric signatures are widely considered to be pathognomonic for monoclonal MC disease. Each aspirate should be subjected to the full extent of MC mutational analysis available at the time, though at present this typically is limited to PCR analysis for the KITD816V mutation. If leukocytosis, erythrocytosis, or thrombocytosis is present, assessment is also warranted for the Janus kinase 2 (JAK2) mutations often found in the MPNs (and perhaps the MPLW515L/K mutation, too, in cases of leukocytosis or thrombocytosis without erythrocytosis which might signal the presence of essential thrombocythemia or myelofibrosis). Similarly, if prominent eosinophilia is observed, tyrosine kinases platelet-derived growth factor receptor alpha (PDGFRα), PDGFRβ, and fibroblast growth factor receptor 1 should be assessed for mutations as recently reviewed elsewhere[53].
The presence of skin lesions characteristic of UP or TMEP warrants biopsy of one or more such lesions, to be immediately processed with routine staining and the above-noted immunohistochemical staining plus assessment for clonality with flow cytometry. As solid tissue flow cytometry requires fresh tissue but PCR mutation analysis does not, it may be reasonable to defer PCR of skin lesion biopsies until other testing finds at least some evidence suggestive of MC disease.
Spontaneously appearing/disappearing, diffusely migratory macular erythematous patchy rashes are common in MCAS, as are scatterings of small ulcerative lesions, too. In the authors’ experience, though, biopsies of such sites rarely reveal increased or otherwise aberrant MC populations, suggesting such lesions may be merely the end result of aberrant release of mediators from distantly located MCs.
If clinical suspicion for SM persists (whether due to serum tryptase persistently > 20 ng/mL or other factors) but two or more marrow biopsies (and possibly also biopsies of suspect skin lesions) are negative, upper and lower endoscopic examination of the gastrointestinal tract is reasonable. Biopsies should be performed of any macroscopically apparent lesions, but blind biopsies of macroscopically normal mucosa should be pursued, too, at multiple points along the tract. All such biopsies should be processed as described above for skin biopsies. Several studies have reported that mast cell counts in GI or genitourinary (GU) tract mucosal biopsies normally number fewer than 20 per high power field[54-58]. However, cut-offs between “normal” and “abnormal” numbers of non-aggregated mast cells are not addressed in either of the two currently proposed diagnostic schemes for MCAS. Furthermore, it is important to remember that the diagnosis of any form of MCAD rests in meeting a set of criteria, so an isolated finding of “increased” tissue mast cells does not establish the diagnosis regardless of the cut-off used to define “increased”, and especially when such cells are not tightly clustered. In the context of other data meeting diagnostic criteria, though, a finding of “increased” tissue mast cells lends additional credence to the diagnosis.
MCs are highly pleomorphic. On routine hematoxylin and eosin (H and E) staining, MCs can be indistinguishable from lymphocytes, plasma cells, macrophages, histiocytes, or spindle cells[59,60]. Thus, in MC disease, not all “lymphocytes” seen with H and E staining are necessarily lymphocytes, and immuno/histochemical staining is required in cases of suspected MCAD. Not infrequently, because of their chronic idiopathic (and often treatment-refractory) gastrointestinal symptoms, patients being evaluated for MCAD have previously undergone GI tract endoscopies with biopsies. Thus, simple reassessment of archived tissue with MC-targeted immuno/histochemical staining may be sufficient to demonstrate that the “benign mucosa” or “mild chronic inflammation” previously seen with H and E staining actually harbors increased MCs. As PCR testing can be performed on preserved tissue, positive immuno/histochemical findings on archived tissue should lead, if sufficient tissue remains, to mutation analysis as possible.
Clinical judgment is required as to whether respiratory or GU tract biopsies are warranted in particularly diagnostically challenging cases, but if pursued, such tissues should be processed as for skin and GI tract biopsies.
Newly or persistently pathologically enlarged (> 1 cm) lymph nodes require biopsy to rule out malignant lymphoproliferative and granulomatous disorders (regardless of whether such disorders can be proven to be independent of, or consequent to, MCAD). However, diffusely migratory, spontaneously waxing/waning adenopathy and/or adenitis is common in MCAD and far more often is a reactive rather than malignant process, though the reactive patterns seen on biopsy can be bizarre (e.g., sinus histiocytosis) and can have the pathologist on the verge of declaring a malignancy. In patients diagnosed with MCAD (or being evaluated for suspected MCAD) who have a longstanding history of spontaneous enlargement of nodes to pathologic size soon followed by spontaneous regression of such adenopathy, the new appearance of a modestly pathologically enlarged lymph node can be watched closely without reflexively proceeding to biopsy, but persistence or progression of adenopathy beyond the range, or outside of the pattern, the patient has usually experienced may warrant biopsy. Node biopsies should be excisional whenever possible and should be submitted not only for the above-noted analyses for MC disease but also for routine analyses for lymphoproliferative disorders and perhaps even - in appropriate clinical settings - specific plasma cell dyscrasias or granulomatous diseases such as amyloidosis, Castleman’s disease, or sarcoidosis.
In addition to checking a serum tryptase, other initial laboratory assessment for MCAD (whether suspected to be mastocytosis or MCAS) should include a variety of common tests as listed in Figure 5. As MCAD commonly causes osteolysis (and, less commonly, osteosclerosis - and occasionally even both processes at different sites in the same patient), it is appropriate to establish a baseline for bone densitometry after the diagnosis of MCAD has been established, as the finding of osteopenia or osteoporosis has therapeutic implications. MCAD can drive erythropenia or erythrocytosis (either of which may be macrocytic, normocytic, or microcytic, engendering appropriate differential diagnostic considerations of secondary processes), leukopenia or leukocytosis, and/or thrombocytopenia or thrombocytosis, but there are no findings in the CBC that are specific for MCAD (other than significant numbers of circulating mast cells signaling mast cell leukemia). Also, as previously noted, certain subtle abnormalities are not uncommonly seen in the leukocyte differential, but often the differential is as normal as the CBC. Indeed, it is a confounding point for hematologists that this disease of fundamentally hematologic classification often presents with not a single abnormality in the CBC or differential. However, many MCAD patients - with either mastocytosis or MCAS - do manifest subtle to gross abnormalities in one or more elements of the CBC, providing the diagnostician important opportunities to consider alternative diagnoses. Of note, though, gross abnormalities in the CBC in advanced mastocytosis may be due more to marrow replacement by MCs, while gross abnormalities in the CBC in less advanced mastocytosis and MCAS are likely due more to MC mediator-driven interference with normal hematopoiesis.
Many MCAD patients also manifest abnormalities in the common serum chemistries, again typically modest in degree but providing the diagnostician opportunities to consider alternative diagnoses regardless of whether they may have risen independently of, or consequent to, MCAD.
Both hypergammaglobulinemia (usually a polyclonal inflammatory phenomenon but occasionally a monoclonal gammopathy of undetermined significance or more advanced clonal plasma cell dyscrasia) and hypogammaglobulinemia can be seen in MCAD[61]; patients sometimes have been previously diagnosed with common variable immunodeficiency. Markedly IgG-deficient patients (< 400 mg/dL) who have suffered major infections or substantial healing complications may be candidates for prophylactic immune globulin therapy.
Histories of “easy” bruising and/or bleeding are frequent amongst MCAD patients. Multiple mechanisms are possible (and not necessarily mutually exclusive) including coagulation factor deficiencies, antiphospholipid antibodies, and/or MC release into the local tissues of (antithrombin-activating) heparin. However, fibrinolysis (as stimulated by heparin release[62] and other fibrinolytic mediators such as tissue plasminogen activator[63]) appears likely to be the dominant cause, explaining why antifibrinolytics such as tranexamic acid can be helpful in controlling MCAD-driven bleeding. The prothrombin time (PT) and activated partial thromboplastin time (aPTT) remain reasonable screening tests in patients with suspected MCAD who report histories of easy bruising/bleeding, but the diagnostician should be aware that local MC release of mediators with sufficient direct or indirect anticoagulant effect to cause local bleeding usually do not provoke systemic anticoagulant effect sufficient to cause rises in PT or aPTT to abnormal levels. Thus, measurement of fibrinolytic mediators[63], as proximate to the onset of bleeding as possible, may be required to prove fibrinolysis if felt clinically important. Otherwise inexplicable prolongations in PT or aPTT should prompt appropriate further evaluation for clotting factor deficiencies. Also, assessment for antiphospholipid antibodies may not be unreasonable in suspected MCAD patients with otherwise inexplicable abnormalities (high or low) in either PT or aPTT and histories of not only easy bruising/bleeding but also thromboembolism or miscarriage.
If not already performed, a careful evaluation for known hypercoagulable disorders should be performed in the patient with suspected MCAD and a history of idiopathic thromboembolism. Such evaluation should include, among other considerations, determination of the plasma level of Factor VIII (produced by various sources including the MC[64] and associated with hypercoagulability[65]) and, with a history of portal/splanchnic vein thrombosis, assessment for the JAK2V617F mutation which might suggest the occult presence of an MPN[66]. Testing for inborn hypercoagulable disorders may not be warranted in cases of initial thromboembolism at ages above 40.
Most patients presenting for evaluation of MCAD have been chronically unwell and have undergone extensive diagnostic evaluation, but the diagnostician considering MCAD nevertheless must carefully review past evaluations and ensure other diagnostic considerations potentially fitting the patient’s unique course have been excluded (e.g., hypothyroidism, celiac sprue, Epstein-Barr virus disease, carcinoid, amyloidosis, porphyria, sarcoidosis, etc.). Even if the root cause of the patient’s multisystem unwellness is MCAD, identification of specific secondary phenomena (e.g., autoimmunity, infection, malignancy, etc.) may permit better outcomes via dual-directed therapy.
If the serum tryptase is < 20 ng/mL and there are no other clinical hints that SM is more likely than MCAS, then an initial laboratory survey of other MC mediators should be pursued in patients clinically suspected of having MCAS. In the authors’ opinion, such an initial mediator survey for evidence of MCAS should include serum chromogranin A; chilled plasma for prostaglandin D2 (PGD2) (and/or 11-β-PGF2α); chilled plasma histamine; chilled plasma heparin (in patients not on exogenous heparin products); and chilled random and 24-h urine collections for PGD2 (and/or 11-β-PGF2α) and N-methylhistamine[26]. In some situations (see below), urinary levels of leukotrienes B4, C4, D4 and E4 may also be worth pursuing[26,67].
Although specimen collection as soon as possible following an acute flare of symptoms is ideal, there is no need to wait for such an event when initially assessing the patient with longstanding baseline symptoms consistent with aberrant MC mediator release. However, if the initial laboratory assessment in a patient with a history suspicious for MCAD is negative, repeat testing is usually warranted but preferably should be deferred until the presentation of an acute flare. If possible, hourly determinations of serum tryptase, plasma PGD2 and histamine, and spot urinary PGD2 and N-methylhistamine should be pursued at baseline and over the next 2-3 h as a flare evolves.
Chromogranin A (CgA) is another known MC product[35,68] which appears quite heat-stable[69] and was found elevated in the serum in 17% (21 out of 122) of a cohort of MCAD patients investigated (LBA, unpublished data). Elevated serum levels of CgA can be helpful toward diagnosing MCAS, but other potential causes of such elevations (heart failure, renal insufficiency, proton pump inhibitor (PPI) use, and neuroendocrine cancer) should be excluded. Changes in serum CgA level in response to initiation or cessation of PPI therapy are fairly reliable and rapid (within 5 d[70]) but highly variable in magnitude[71,72], likely due to multiple mechanisms including pharmacogenomic polymorphisms (largely in cytochrome p450 isoenzyme 2C19[73]) and increase in density of CgA-secreting enterochromaffin cells (especially in gastric tissue) in response to gastric acid reduction[74]. Cessation of PPI therapy at least 5 days prior to submission of a serum sample for CgA assessment should permit an accurate gauge of the baseline CgA level.
Although it was the first MC mediator to be discovered[75,76] and is a highly sensitive and specific indicator of MC activity[16,63], the plasma heparin level is difficult to measure accurately in the clinical setting. The metabolism of heparin is complex[77], but it is clear that it has a short half-life (generally less than one hour) and decomposes rapidly even at chilled temperatures[63]. Seidel et al[63] reported an upper limit of normal plasma heparin of 0.02 anti-Factor Xa units/mL, but the utility of assessing the plasma heparin level for evidence of MCAS may be constrained by the fact that most of the commercially available assays have a lower limit of detectability of 0.05 or 0.10 anti-Factor Xa units/mL since such assays are used far more to assess anticoagulant adequacy of therapeutic heparinization than to assess endogenous heparin levels. However, about 50% of MCAD patients will manifest a plasma heparin level exceeding 0.05 anti-Factor Xa units/mL on commercially available assays (105 out of 202 MCAD patients in a current study; unpublished data), and in such patients whose detectable plasma heparin levels cannot be attributed to therapeutic heparin or to the only other known endogenous source of heparin in humans (basophils), MC activation almost certainly is the source.
Like heparin, histamine is slightly less specific for MC disease than tryptase in that histamine is also released by basophils. Unlike heparin, histamine is not particularly heat-labile[78] but nevertheless has a short half-life in vivo[79,80] (estimates have ranged from 1 min to 1 h and may vary based on increased histaminase activity during anaphylaxis[81]). Histamine appears to be stable in separated plasma at room temperature for at least 48 h[82]. However, because histamine assays often must be performed at distant reference laboratories (requiring specimen storage and transport exceeding 48 h), plasma specimens for histamine levels should be kept continuously chilled at all stages of handling. Histamine’s major metabolite, N-methylhistamine, has a longer half-life in vivo[80] and may be a preferable measure over histamine, especially when a sample cannot be collected during a flare of symptoms or when other constraints preclude measurement of both molecules.
Although also produced in macrophages[83-86], Langerhans cells[87], liver endothelium[86], platelets[88], Th2 helper T cells[89], stimulated osteoblasts[90], and possibly adipocytes[91], PGD2 appears to be far dominantly produced in MCs[92,93], yielding attractive specificity for clinical detection of MCAD. In patients with MC activation producing increases in urinary N-methylhistamine, the fold increase in urinary PGD2 is substantially greater than seen for the histamine metabolite[94]. However, PGD2 appears to have an even shorter half-life than histamine (on the order of 1-30 min in various studies)[95-97]. In fact, PGD2 is metabolized so rapidly that its measured levels may substantially underestimate its total production[98]. Some PGD2 metabolites, though, are more stable than the parent compound (e.g., 9α,11β-PGF2α[92]), leading some to preferentially test such metabolites over PGD2. Of note, though, far more PGF2α comes from reduction of PGH2, and even some from PGE2, which are produced by a range of other types of cells[99], making the value of PGF2α as a marker for MC activity less clear). Assays of levels of histamine and prostaglandin metabolites are further complicated by the need of many clinical laboratories to ship samples to a reference laboratory for measurement. Care must be taken by the patient and laboratory staff to maintain the samples (particularly for heparin and PGD2) in chilled condition throughout collection, storage, and transport until final processing. It is unclear whether urinary PGD2 is exclusively a product of the kidneys[100] or dominantly a filtering of plasma PGD2[92]. If the former is true, a low urinary PGD2 could be due to chronic kidney disease (CKD), though certainly patients with CKD due to activated MCs can manifest elevated urinary PGD2 levels. Therefore, CKD is not a reason to forego testing of the urinary PGD2 level.
Ideally, a 24-h urine collection is preferred over a spot/random collection given that the evanescence of mediator flares and the short half-lives of many mediators make spot urine collections and plasma assays less likely to catch elevated levels of mediators. However, from an efficiency perspective, testing both 24-h and random specimens at the same time may not be unreasonable in patients whose mysterious chronic illness has already consumed extensive resources.
Non-steroidal anti-inflammatory drugs (NSAIDs), which inhibit cyclooxygenase and thus limit prostaglandin production, can result in low PGD2 levels in the blood and urine. Similar to the precaution with PPI therapy when assessing for serum CgA elevation, the patient’s history of use of NSAIDs, in both prescription and over-the-counter products, should be reviewed when planning the laboratory assessment for prostaglandin levels. Like most PPIs, some NSAIDs have long half-lives permitting daily dosing, and thus patients should be cautioned to abstain, if possible, from all NSAIDs for at least 5 d prior to specimen collection for assessment of prostaglandins.
Given the heterogeneity of MCAD and the above-noted challenges in detecting elevated levels of MC mediators, it should not be surprising that some patients present not only with histories which are classic for MCAS but also with initial screenings for the most sensitive and specific MC mediators which are normal. When repeated efforts to identify aberrant MC activation using the above-described screening approach all fail, consideration can be given to screening for aberrant expression of less specific MC mediators such as Factor VIII[64,101], plasma free norepinephrine[102], tumor necrosis factor alpha[103-111] and interleukin-6[103]. Plasma free norepinephrine is often ordered as part of a plasma free catecholamine profile; in many MCAS patients a pattern of elevated norepinephrine, low-normal or low epinephrine, and sometimes elevated dopamine is seen (LBA and GJM, unpublished data).
Although commercial testing (whether through local or reference laboratories) is not yet widely available, levels of MC mediators leukotriene B4 and cysteinyl leukotrienes C4, D4 and E4 have been reported to be elevated in patients with SM as compared to healthy controls[67]. Plasma and urinary leukotrienes also increase with acute attacks of asthma[112], a disease increasingly suspected to involve aberrantly active MCs[113]. However, leukotriene expression has not been specifically studied in the MCAS population. Furthermore, leukotrienes are synthesized in a variety of myeloid cells (and epithelial cells as well)[114,115], so the specificity of elevated leukotriene metabolite levels for MCAD is unclear and may depend substantially on the presence of a clinical history compatible with MCAD. Whether elevated leukotriene levels are related more to MC load or to MC activity remains to be determined. However, if the clinical history is best explained by MC activation but abnormal levels of the previously discussed biochemical markers cannot be identified, it would not be unreasonable to also examine levels of plasma and urinary leukotriene metabolites if commercial assays of such are accessible.
The short half-lives and thermolability of many MC mediators require continuous specimen chilling throughout collection, storage, and transport. Particularly with regard to 24-h urine collections for MC mediator testing, patients should be carefully educated to pre-chill the collection container overnight before beginning the collection and then to keep the container continuously chilled while following an otherwise standard 24-h urine collection protocol; the container should be removed from the refrigerator or ice chest only when imminently needed and should be returned to chilling as soon as possible. Patients should also be cautioned to maintain the container in a chilled environment throughout transport. We recommend the container be placed in a bag filled with ice and sealed, with the bag then placed in an ice chest filled with ice and sealed for transport to the accessioning lab, whereupon the bag can be removed from the chest and provided to the technician with a reminder of the criticality of keeping the specimen chilled.
Laboratory staff often are unfamiliar with MC mediator testing, previously a rarely undertaken endeavor. Consideration should be given by the diagnostician to sharing with laboratory personnel the ultimate clinical goal of such testing and the importance of maintaining thermal integrity of these specimens at all times, including at the time of initial accessioning as well as when packing specimens for transport to reference laboratories that may be thousands of miles distant, transits that may involve long periods sitting in unventilated cargo containers on hot tarmacs. Use of well-insulated containers, and liberal placement of cold packs in the insulated container, should be de rigueur when packing such specimens for long-distance transport.
If PGD2 (or 11-β-PGF2α) levels below the lower limit of normal are determined and the patient denies any recent use of NSAIDs, or if “normal” MC mediator levels are repeatedly seen despite specimens being accessioned at particularly symptomatic times, it may be useful to ask the patient about his observations, while at the lab, as to whether the laboratory staff maintained the specimen in a chilled environment. Aside from NSAID use, loss of thermal integrity is the most common reason for low PGD2 levels in the authors’ experience.
With growing appreciation of the prevalence of MCAD (particularly MCAS), there is a growing need to pursue diagnostic evaluation for MCAD outside of the few centers specializing in this area. An understanding of the spectrum of MCAD and the similarities and differences amongst the various forms of the disease is helpful in guiding the approach to testing. Especially if MCAS is confirmed to usually be a clonal disease, the rise of personal genomics may come to obviate many of the present challenges in diagnosing MCAD, but with appropriate collaboration amongst the diagnostician, patient, other relevant clinicians, and laboratory staff, today’s challenges can be surmounted. Especially given that the majority of the MCAD iceberg seems likely to be MCAS and that significantly helpful therapy can be found for most MCAD patients (including most MCAS patients), efforts to smooth the path toward diagnosis of MCAD are worthwhile.
P- Reviewers: Fozza C, Imashuku S, Takahashi M S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
| 1. | Kalesnikoff J, Galli SJ. New developments in mast cell biology. Nat Immunol. 2008;9:1215-1223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 564] [Cited by in RCA: 549] [Article Influence: 32.3] [Reference Citation Analysis (1)] |
| 2. | von Recklinghausen F. Ueber Eiter - und Bindegewebskörperchen. Virchows Arch. 1863;28:157-197. [RCA] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 93] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Unna P. Beiträge zur Anatomie und Pathogenese der Urticaria simplex und pigmentosa. Monatschrift der praktischen Dermatologie. 1887;6:9-18. |
| 4. | Ellis JM. Urticaria pigmentosa; a report of a case with autopsy. Arch Pathol (Chic). 1949;48:426-435. [PubMed] |
| 5. | Efrati P, Klajman A, Spitz H. Mast cell leukemia? Malignant mastocytosis with leukemia-like manifestations. Blood. 1957;12:869-882. [PubMed] |
| 6. | Furitsu T, Tsujimura T, Tono T, Ikeda H, Kitayama H, Koshimizu U, Sugahara H, Butterfield JH, Ashman LK, Kanayama Y. Identification of mutations in the coding sequence of the proto-oncogene c-kit in a human mast cell leukemia cell line causing ligand-independent activation of c-kit product. J Clin Invest. 1993;92:1736-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 618] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 7. | Akin C, Metcalfe DD. The biology of Kit in disease and the application of pharmacogenetics. J Allergy Clin Immunol. 2004;114:13-19; quiz 20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 94] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Nagata H, Worobec AS, Oh CK, Chowdhury BA, Tannenbaum S, Suzuki Y, Metcalfe DD. Identification of a point mutation in the catalytic domain of the protooncogene c-kit in peripheral blood mononuclear cells of patients who have mastocytosis with an associated hematologic disorder. Proc Natl Acad Sci USA. 1995;92:10560-10564. [PubMed] |
| 9. | Garcia-Montero AC, Jara-Acevedo M, Teodosio C, Sanchez ML, Nunez R, Prados A, Aldanondo I, Sanchez L, Dominguez M, Botana LM. KIT mutation in mast cells and other bone marrow hematopoietic cell lineages in systemic mast cell disorders: a prospective study of the Spanish Network on Mastocytosis (REMA) in a series of 113 patients. Blood. 2006;108:2366-2372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 378] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 10. | D'Ambrosio C, Akin C, Wu Y, Magnusson MK, Metcalfe DD. Gene expression analysis in mastocytosis reveals a highly consistent profile with candidate molecular markers. J Allergy Clin Immunol. 2003;112:1162-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Orfao A, Garcia-Montero AC, Sanchez L, Escribano L. Recent advances in the understanding of mastocytosis: the role of KIT mutations. Br J Haematol. 2007;138:12-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 158] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Mayerhofer M, Gleixner KV, Hoelbl A, Florian S, Hoermann G, Aichberger KJ, Bilban M, Esterbauer H, Krauth MT, Sperr WR. Unique effects of KIT D816V in BaF3 cells: induction of cluster formation, histamine synthesis, and early mast cell differentiation antigens. J Immunol. 2008;180:5466-5476. [PubMed] |
| 13. | Haenisch B, Nöthen MM, Molderings GJ. Systemic mast cell activation disease: the role of molecular genetic alterations in pathogenesis, heritability and diagnostics. Immunology. 2012;137:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Broesby-Olsen S, Kristensen T, Vestergaard H, Brixen K, Møller MB, Bindslev-Jensen C. KIT D816V mutation burden does not correlate to clinical manifestations of indolent systemic mastocytosis. J Allergy Clin Immunol. 2013;In press. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Lawley W, Hird H, Mallinder P, McKenna S, Hargadon B, Murray A, Bradding P. Detection of an activating c-kit mutation by real-time PCR in patients with anaphylaxis. Mutat Res. 2005;572:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Roberts LJ, Oates JA. Biochemical diagnosis of systemic mast cell disorders. J Invest Dermatol. 1991;96:19S-24S; discussion 24S-25S; 60S-65S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Sonneck K, Florian S, Müllauer L, Wimazal F, Födinger M, Sperr WR, Valent P. Diagnostic and subdiagnostic accumulation of mast cells in the bone marrow of patients with anaphylaxis: Monoclonal mast cell activation syndrome. Int Arch Allergy Immunol. 2007;142:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Akin C, Scott LM, Kocabas CN, Kushnir-Sukhov N, Brittain E, Noel P, Metcalfe DD. Demonstration of an aberrant mast-cell population with clonal markers in a subset of patients with “idiopathic” anaphylaxis. Blood. 2007;110:2331-2333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 178] [Article Influence: 9.9] [Reference Citation Analysis (1)] |
| 19. | Molderings GJ, Kolck UW, Scheurlen C, Brüss M, Homann J, Von Kügelgen I. Multiple novel alterations in Kit tyrosine kinase in patients with gastrointestinally pronounced systemic mast cell activation disorder. Scand J Gastroenterol. 2007;42:1045-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Molderings GJ, Meis K, Kolck UW, Homann J, Frieling T. Comparative analysis of mutation of tyrosine kinase kit in mast cells from patients with systemic mast cell activation syndrome and healthy subjects. Immunogenetics. 2010;62:721-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Kralovics R. Genetic complexity of myeloproliferative neoplasms. Leukemia. 2008;22:1841-1848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Schwaab J, Schnittger S, Sotlar K, Walz C, Fabarius A, Pfirrmann M, Kohlmann A, Grossmann V, Meggendorfer M, Horny HP. Comprehensive mutational profiling in advanced systemic mastocytosis. Blood. 2013;122:2460-2466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 194] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 23. | Akin C, Valent P, Metcalfe DD. Mast cell activation syndrome: Proposed diagnostic criteria. J Allergy Clin Immunol. 2010;126:1099-1104.e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 248] [Cited by in RCA: 238] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 24. | Molderings GJ, Haenisch B, Bogdanow M, Fimmers R, Nöthen MM. Familial occurrence of systemic mast cell activation disease. PLoS One. 2013;8:e76241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Nakamura Y, Kambe N, Saito M, Nishikomori R, Kim YG, Murakami M, Núñez G, Matsue H. Mast cells mediate neutrophil recruitment and vascular leakage through the NLRP3 inflammasome in histamine-independent urticaria. J Exp Med. 2009;206:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 150] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 26. | Molderings GJ, Brettner S, Homann J, Afrin LB. Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options. J Hematol Oncol. 2011;4:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 27. | Afrin LB. Mast cell activation disorder masquerading as pure red cell aplasia. Int J Hematol. 2010;91:907-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Afrin LB. Polycythemia from mast cell activation syndrome: lessons learned. Am J Med Sci. 2011;342:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Afrin LB. Mast cell activation syndrome masquerading as agranulocytosis. Mil Med. 2012;177:113-117. [PubMed] |
| 30. | Travis WD, Li CY, Bergstralh EJ, Yam LT, Swee RG. Systemic mast cell disease. Analysis of 58 cases and literature review. Medicine (Baltimore). 1988;67:345-368. [PubMed] |
| 31. | Travis WD, Li CY, Yam LT, Bergstralh EJ, Swee RG. Significance of systemic mast cell disease with associated hematologic disorders. Cancer. 1988;62:965-972. [PubMed] |
| 32. | Valent P, Horny HP, Escribano L, Longley BJ, Li CY, Schwartz LB, Marone G, Nuñez R, Akin C, Sotlar K. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001;25:603-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 777] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 33. | Horny HP, Metcalfe DD, Bennett J, Bain BJ, Akin C, Escribano L, Valent P. Mastocytosis. WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues (4th edition.). Lyon, France: International Agency for Research and Cancer 2008; 54–63. |
| 34. | Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, Castells M, Escribano L, Hartmann K, Lieberman P. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157:215-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 452] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 35. | Ibelgaufts H; Mast Cells (In: COPE: Cytokines and Cells Online Pathfinder Encyclopaedia, 2013, Sept 3). Avalible from: URL: http: //www.copewithcytokines.de/cope.cgi?key=mast cells. . |
| 36. | Afrin L. Presentation, Diagnosis, and Management of Mast Cell Activation Syndrome. Mast Cells: Phenotypic Features, Biological Functions, and Role in Immunity. Happauge, NY: Nova Science Publishers 2013; 155-231. |
| 37. | Hermine O, Lortholary O, Leventhal PS, Catteau A, Soppelsa F, Baude C, Cohen-Akenine A, Palmérini F, Hanssens K, Yang Y. Case-control cohort study of patients’ perceptions of disability in mastocytosis. PLoS One. 2008;3:e2266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 124] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 38. | Valent P, Sperr WR, Akin C. How I treat patients with advanced systemic mastocytosis. Blood. 2010;116:5812-5817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 39. | Alfter K, von Kügelgen I, Haenisch B, Frieling T, Hülsdonk A, Haars U, Rolfs A, Noe G, Kolck UW, Homann J. New aspects of liver abnormalities as part of the systemic mast cell activation syndrome. Liver Int. 2009;29:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 40. | Schwartz LB, Sakai K, Bradford TR, Ren S, Zweiman B, Worobec AS, Metcalfe DD. The alpha form of human tryptase is the predominant type present in blood at baseline in normal subjects and is elevated in those with systemic mastocytosis. J Clin Invest. 1995;96:2702-2710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 250] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 41. | Borer-Reinhold M, Haeberli G, Bitzenhofer M, Jandus P, Hausmann O, Fricker M, Helbling A, Müller U. An increase in serum tryptase even below 11.4 ng/mL may indicate a mast cell-mediated hypersensitivity reaction: a prospective study in Hymenoptera venom allergic patients. Clin Exp Allergy. 2011;41:1777-1783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 42. | Sperr WR, Jordan JH, Fiegl M, Escribano L, Bellas C, Dirnhofer S, Semper H, Simonitsch-Klupp I, Horny HP, Valent P. Serum tryptase levels in patients with mastocytosis: correlation with mast cell burden and implication for defining the category of disease. Int Arch Allergy Immunol. 2002;128:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 145] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 43. | Alvarez-Twose I, González de Olano D, Sánchez-Muñoz L, Matito A, Esteban-López MI, Vega A, Mateo MB, Alonso Díaz de Durana MD, de la Hoz B, Del Pozo Gil MD. Clinical, biological, and molecular characteristics of clonal mast cell disorders presenting with systemic mast cell activation symptoms. J Allergy Clin Immunol. 2010;125:1269-1278.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 225] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 44. | van Doormaal JJ, van der Veer E, van Voorst Vader PC, Kluin PM, Mulder AB, van der Heide S, Arends S, Kluin-Nelemans JC, Oude Elberink JN, de Monchy JG. Tryptase and histamine metabolites as diagnostic indicators of indolent systemic mastocytosis without skin lesions. Allergy. 2012;67:683-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 45. | Schwartz LB, Metcalfe DD, Miller JS, Earl H, Sullivan T. Tryptase levels as an indicator of mast-cell activation in systemic anaphylaxis and mastocytosis. N Engl J Med. 1987;316:1622-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 533] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 46. | Hallgren J, Pejler G. Biology of mast cell tryptase. An inflammatory mediator. FEBS J. 2006;273:1871-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 47. | Schwartz LB, Bradford TR. Regulation of tryptase from human lung mast cells by heparin. Stabilization of the active tetramer. J Biol Chem. 1986;261:7372-7379. [PubMed] |
| 48. | Fajardo I, Pejler G. Human mast cell beta-tryptase is a gelatinase. J Immunol. 2003;171:1493-1499. [PubMed] |
| 49. | Goldstein SM, Wintroub BU. Mast cell proteases. The Mast Cell in Health and Disease. New York: Marcel Dekker 1993; 343-380. |
| 50. | Butterfield JH, Li CY. Bone marrow biopsies for the diagnosis of systemic mastocytosis: is one biopsy sufficient? Am J Clin Pathol. 2004;121:264-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Horny HP, Valent P. Diagnosis of mastocytosis: general histopathological aspects, morphological criteria, and immunohistochemical findings. Leuk Res. 2001;25:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 162] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 52. | Escribano L, Orfao A, Díaz-Agustin B, Villarrubia J, Cerveró C, López A, Marcos MA, Bellas C, Fernández-Cañadas S, Cuevas M. Indolent systemic mast cell disease in adults: immunophenotypic characterization of bone marrow mast cells and its diagnostic implications. Blood. 1998;91:2731-2736. [PubMed] |
| 53. | Havelange V, Demoulin JB. Review of current classification, molecular alterations, and tyrosine kinase inhibitor therapies in myeloproliferative disorders with hypereosinophilia. J Blood Med. 2013;4:111-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 54. | Yeom JS, Choi MB, Seo JH, Park JS, Lim JY, Park CH, Woo HO, Youn HS, Ko GH, Baik SC. Relationship between headache and mucosal mast cells in pediatric Helicobacter pylori-negative functional dyspepsia. Cephalalgia. 2013;33:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 55. | Zare-Mirzaie A, Lotfi M, Sadeghipour A, Haghi-Ashtiani MT. Analysis of colonic mucosa mast cell count in patients with chronic diarrhea. Saudi J Gastroenterol. 2012;18:322-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 56. | Martínez C, Lobo B, Pigrau M, Ramos L, González-Castro AM, Alonso C, Guilarte M, Guilá M, de Torres I, Azpiroz F. Diarrhoea-predominant irritable bowel syndrome: an organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2013;62:1160-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 209] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 57. | Vivinus-Nébot M, Dainese R, Anty R, Saint-Paul MC, Nano JL, Gonthier N, Marjoux S, Frin-Mathy G, Bernard G, Hébuterne X. Combination of allergic factors can worsen diarrheic irritable bowel syndrome: role of barrier defects and mast cells. Am J Gastroenterol. 2012;107:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 58. | Bassotti G, Villanacci V, Nascimbeni R, Cadei M, Manenti S, Sabatino G, Maurer CA, Cathomas G, Salerni B. Colonic mast cells in controls and slow transit constipation patients. Aliment Pharmacol Ther. 2011;34:92-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 59. | Brunning RD, McKenna RW, Rosai J, Parkin JL, Risdall R. Systemic mastocytosis. Extracutaneous manifestations. Am J Surg Pathol. 1983;7:425-438. [PubMed] |
| 60. | Swieter M, Lee TD, Stead RH, Fujimaki H, Befus D. Mast cell pleomorphism: properties of intestinal mast cells. Adv Exp Med Biol. 1987;216A:613-623. [PubMed] |
| 61. | Worobec AS, Semere T, Nagata H, Metcalfe DD. Clinical correlates of the presence of the Asp816Val c-kit mutation in the peripheral blood mononuclear cells of patients with mastocytosis. Cancer. 1998;83:2120-2129. [PubMed] |
| 62. | Upchurch GR, Valeri CR, Khuri SF, Rohrer MJ, Welch GN, MacGregor H, Ragno G, Francis S, Rodino LJ, Michelson AD. Effect of heparin on fibrinolytic activity and platelet function in vivo. Am J Physiol. 1996;271:H528-H534. [PubMed] |
| 63. | Seidel H, Molderings GJ, Oldenburg J, Meis K, Kolck UW, Homann J, Hertfelder HJ. Bleeding diathesis in patients with mast cell activation disease. Thromb Haemost. 2011;106:987-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 64. | Kindblom LG. Factor VIII related antigen and mast cells. Acta Pathol Microbiol Immunol Scand A. 1982;90:437-439. [PubMed] |
| 65. | Kyrle PA, Minar E, Hirschl M, Bialonczyk C, Stain M, Schneider B, Weltermann A, Speiser W, Lechner K, Eichinger S. High plasma levels of factor VIII and the risk of recurrent venous thromboembolism. N Engl J Med. 2000;343:457-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 520] [Cited by in RCA: 498] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 66. | Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S, Cazals-Hatem D, Plessier A, Garcia-Pagan JC, Darwish Murad S. The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood. 2008;111:4922-4929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 219] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 67. | Raithel M, Zopf Y, Kimpel S, Naegel A, Molderings GJ, Buchwald F, Schultis HW, Kressel J, Hahn EG, Konturek P. The measurement of leukotrienes in urine as diagnostic option in systemic mastocytosis. J Physiol Pharmacol. 2011;62:469-472. [PubMed] |
| 68. | Prasad P, Yanagihara AA, Small-Howard AL, Turner H, Stokes AJ. Secretogranin III directs secretory vesicle biogenesis in mast cells in a manner dependent upon interaction with chromogranin A. J Immunol. 2008;181:5024-5034. [PubMed] |
| 69. | Takiyyuddin MA, Cervenka JH, Hsiao RJ, Barbosa JA, Parmer RJ, O’Connor DT. Chromogranin A. Storage and release in hypertension. Hypertension. 1990;15:237-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 70. | Pregun I, Herszényi L, Juhász M, Miheller P, Hritz I, Patócs A, Rácz K, Tulassay Z. Effect of proton-pump inhibitor therapy on serum chromogranin a level. Digestion. 2011;84:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 71. | Sanduleanu S, Stridsberg M, Jonkers D, Hameeteman W, Biemond I, Lundqvist G, Lamers C, Stockbrügger RW. Serum gastrin and chromogranin A during medium- and long-term acid suppressive therapy: a case-control study. Aliment Pharmacol Ther. 1999;13:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | Fossmark R, Jianu CS, Martinsen TC, Qvigstad G, Syversen U, Waldum HL. Serum gastrin and chromogranin A levels in patients with fundic gland polyps caused by long-term proton-pump inhibition. Scand J Gastroenterol. 2008;43:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 73. | Furuta T, Shirai N, Sugimoto M, Ohashi K, Ishizaki T. Pharmacogenomics of proton pump inhibitors. Pharmacogenomics. 2004;5:181-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 104] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 74. | Sanduleanu S, De Bruïne A, Stridsberg M, Jonkers D, Biemond I, Hameeteman W, Lundqvist G, Stockbrügger RW. Serum chromogranin A as a screening test for gastric enterochromaffin-like cell hyperplasia during acid-suppressive therapy. Eur J Clin Invest. 2001;31:802-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 75. | Holmgren H, Wilander O. Beiträge zur Kenntnis der Chemie and Funktion der Ehrlichschen Mastzellen. Z Mikroskop Anat Forsch. 1937;42:242-278. |
| 76. | Jorpes E, Holmgren H, Wilander O. Über das Vorkommen von Heparin in den Gefässwänden und in den Augen. Z Mikroskop Anat Forsch. 1937;42:279-300. |
| 77. | Hirsh J, Anand SS, Halperin JL, Fuster V. Guide to anticoagulant therapy: Heparin : a statement for healthcare professionals from the American Heart Association. Circulation. 2001;103:2994-3018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 375] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 78. | Emborg J, Laursen BG, Dalgaard P. Significant histamine formation in tuna (Thunnus albacares) at 2 degrees C--effect of vacuum- and modified atmosphere-packaging on psychrotolerant bacteria. Int J Food Microbiol. 2005;101:263-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 116] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 79. | Laroche D, Vergnaud MC, Sillard B, Soufarapis H, Bricard H. Biochemical markers of anaphylactoid reactions to drugs. Comparison of plasma histamine and tryptase. Anesthesiology. 1991;75:945-949. [PubMed] |
| 80. | Takeda J, Ueda E, Takahashi J, Fukushima K. Plasma N-methylhistamine concentration as an indicator of histamine release by intravenous d-tubocurarine in humans: preliminary study in five patients by radioimmunoassay kits. Anesth Analg. 1995;80:1015-1017. [PubMed] |
| 81. | Lake AM, Kagey-Sobotka A, Jakubowicz T, Lichtenstein LM. Histamine release in acute anaphylactic enteropathy of the rat. J Immunol. 1984;133:1529-1534. [PubMed] |
| 82. | Laroche D, Dubois F, Gérard JL, Lefrançois C, André B, Vergnaud MC, Dubus L, Bricard H. Radioimmunoassay for plasma histamine: a study of false positive and false negative values. Br J Anaesth. 1995;74:430-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 83. | Meyers CD, Liu P, Kamanna VS, Kashyap ML. Nicotinic acid induces secretion of prostaglandin D2 in human macrophages: an in vitro model of the niacin flush. Atherosclerosis. 2007;192:253-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 84. | Hsueh W. Prostaglandin biosynthesis in pulmonary macrophages. Am J Pathol. 1979;97:137-148. [PubMed] |
| 85. | Decker K. Biologically active products of stimulated liver macrophages (Kupffer cells). Eur J Biochem. 1990;192:245-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 628] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 86. | Kuiper J, Zijlstra FJ, Kamps JA, van Berkel TJ. Identification of prostaglandin D2 as the major eicosanoid from liver endothelial and Kupffer cells. Biochim Biophys Acta. 1988;959:143-152. [PubMed] |
| 87. | Maciejewski-Lenoir D, Richman JG, Hakak Y, Gaidarov I, Behan DP, Connolly DT. Langerhans cells release prostaglandin D2 in response to nicotinic acid. J Invest Dermatol. 2006;126:2637-2646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 150] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 88. | Ali M, Cerskus AL, Zamecnik J, McDonald JW. Synthesis of prostaglandin D2 and thromboxane B2 by human platelets. Thromb Res. 1977;11:485-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 89. | Tanaka K, Ogawa K, Sugamura K, Nakamura M, Takano S, Nagata K. Cutting edge: differential production of prostaglandin D2 by human helper T cell subsets. J Immunol. 2000;164:2277-2280. [PubMed] |
| 90. | Gallant MA, Samadfam R, Hackett JA, Antoniou J, Parent JL, de Brum-Fernandes AJ. Production of prostaglandin D(2) by human osteoblasts and modulation of osteoprotegerin, RANKL, and cellular migration by DP and CRTH2 receptors. J Bone Miner Res. 2005;20:672-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 91. | Jowsey IR, Murdock PR, Moore GB, Murphy GJ, Smith SA, Hayes JD. Prostaglandin D2 synthase enzymes and PPARgamma are co-expressed in mouse 3T3-L1 adipocytes and human tissues. Prostaglandins Other Lipid Mediat. 2003;70:267-284. [PubMed] |
| 92. | Bochenek G, Nizankowska E, Gielicz A, Swierczyńska M, Szczeklik A. Plasma 9alpha,11beta-PGF2, a PGD2 metabolite, as a sensitive marker of mast cell activation by allergen in bronchial asthma. Thorax. 2004;59:459-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 90] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 93. | Dahlén SE, Kumlin M. Monitoring mast cell activation by prostaglandin D2 in vivo. Thorax. 2004;59:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 94. | Morrow JD, Guzzo C, Lazarus G, Oates JA, Roberts LJ. Improved diagnosis of mastocytosis by measurement of the major urinary metabolite of prostaglandin D2. J Invest Dermatol. 1995;104:937-940. [PubMed] |
| 95. | Suzuki F, Hayashi H, Hayaishi O. Transport of prostaglandin D2 into brain. Brain Res. 1986;385:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 96. | Maclouf J, Corvazier E, Wang ZY. Development of a radioimmunoassay for prostaglandin D2 using an antiserum against 11-methoxime prostaglandin D2. Prostaglandins. 1986;31:123-132. [PubMed] |
| 97. | Schuligoi R, Schmidt R, Geisslinger G, Kollroser M, Peskar BA, Heinemann A. PGD2 metabolism in plasma: kinetics and relationship with bioactivity on DP1 and CRTH2 receptors. Biochem Pharmacol. 2007;74:107-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 98. | Haberl C, Hültner L, Flügel A, Falk M, Geuenich S, Wilmanns W, Denzlinger C. Release of prostaglandin D2 by murine mast cells: importance of metabolite formation for antiproliferative activity. Mediators Inflamm. 1998;7:79-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 99. | Zhang J, Gong Y, Yu Y. PG F(2α) Receptor: A Promising Therapeutic Target for Cardiovascular Disease. Front Pharmacol. 2010;1:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 100. | Liston TE, Roberts LJ. Metabolic fate of radiolabeled prostaglandin D2 in a normal human male volunteer. J Biol Chem. 1985;260:13172-13180. [PubMed] |
| 101. | Akiyama M, Watanabe Y, Nishikawa T. Immunohistochemical characterization of human cutaneous mast cells in urticaria pigmentosa (cutaneous mastocytosis). Acta Pathol Jpn. 1991;41:344-349. [PubMed] |
| 102. | Freeman JG, Ryan JJ, Shelburne CP, Bailey DP, Bouton LA, Narasimhachari N, Domen J, Siméon N, Couderc F, Stewart JK. Catecholamines in murine bone marrow derived mast cells. J Neuroimmunol. 2001;119:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 103. | Azzolina A, Bongiovanni A, Lampiasi N. Substance P induces TNF-alpha and IL-6 production through NF kappa B in peritoneal mast cells. Biochim Biophys Acta. 2003;1643:75-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 162] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 104. | Gordon JR, Galli SJ. Mast cells as a source of both preformed and immunologically inducible TNF-alpha/cachectin. Nature. 1990;346:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 736] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 105. | Echtenacher B, Männel DN, Hültner L. Critical protective role of mast cells in a model of acute septic peritonitis. Nature. 1996;381:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 696] [Cited by in RCA: 667] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 106. | Kaartinen M, Penttilä A, Kovanen PT. Mast cells in rupture-prone areas of human coronary atheromas produce and store TNF-alpha. Circulation. 1996;94:2787-2792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 107. | Suto H, Nakae S, Kakurai M, Sedgwick JD, Tsai M, Galli SJ. Mast cell-associated TNF promotes dendritic cell migration. J Immunol. 2006;176:4102-4112. [PubMed] |
| 108. | Nakae S, Suto H, Kakurai M, Sedgwick JD, Tsai M, Galli SJ. Mast cells enhance T cell activation: Importance of mast cell-derived TNF. Proc Natl Acad Sci USA. 2005;102:6467-6472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 204] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 109. | Bradding P, Mediwake R, Feather IH, Madden J, Church MK, Holgate ST, Howarth PH. TNF alpha is localized to nasal mucosal mast cells and is released in acute allergic rhinitis. Clin Exp Allergy. 1995;25:406-415. [PubMed] |
| 110. | Walsh LJ, Trinchieri G, Waldorf HA, Whitaker D, Murphy GF. Human dermal mast cells contain and release tumor necrosis factor alpha, which induces endothelial leukocyte adhesion molecule 1. Proc Natl Acad Sci USA. 1991;88:4220-4224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 421] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 111. | Nakae S, Ho LH, Yu M, Monteforte R, Iikura M, Suto H, Galli SJ. Mast cell-derived TNF contributes to airway hyperreactivity, inflammation, and TH2 cytokine production in an asthma model in mice. J Allergy Clin Immunol. 2007;120:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 151] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 112. | Sampson AP, Castling DP, Green CP, Price JF. Persistent increase in plasma and urinary leukotrienes after acute asthma. Arch Dis Child. 1995;73:221-225. [PubMed] |
| 113. | Brightling CE, Bradding P. The re-emergence of the mast cell as a pivotal cell in asthma pathogenesis. Curr Allergy Asthma Rep. 2005;5:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 114. | Tanaka S, Tanaka H, Abe S. High dose of inhaled fluticasone reduces high levels of urinary leukotriene E4 in the early morning in mild and moderate nocturnal asthma. Chest. 2003;124:1768-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 115. | Leukotriene B4; Human metabolome database (2013, May 29). Avalible from: URL: http: //www.hmdb.ca/metabolites/HMDB01085. . |
| 116. | Longley J, Duffy TP, Kohn S. The mast cell and mast cell disease. J Am Acad Dermatol. 1995;32:545-651; quiz 562-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 140] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 117. | Rosbotham JL, Malik NM, Syrris P, Jeffery S, Bedlow A, Gharraie S, Murday VA, Holden CA, Carter ND. Lack of c-kit mutation in familial urticaria pigmentosa. Br J Dermatol. 1999;140:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 118. | Lim KH, Tefferi A, Lasho TL, Finke C, Patnaik M, Butterfield JH, McClure RF, Li CY, Pardanani A. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood. 2009;113:5727-5736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 411] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 119. | Molderings GJ, Kolck U, Scheurlen C, Brüss M, Frieling T, Raithel M, Homann J. Systemic mast cell disease with gastrointestinal symptoms--a diagnostic questionnaire. Dtsch Med Wochenschr. 2006;131:2095-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |