Published online Apr 18, 2017. doi: 10.5312/wjo.v8.i4.357
Peer-review started: November 23, 2016
First decision: December 15, 2016
Revised: December 21, 2016
Accepted: January 11, 2017
Article in press: January 14, 2017
Published online: April 18, 2017
To investigate the clinical and functional outcomes following total hip arthroplasty (THA) in patients with Paget’s disease.
We carried out a systematic review of the literature to determine the functional outcome, complications and revision rates of THA in patients with Paget’s disease. Eight studies involving 358 hips were reviewed. The mean age was 70.4 years and follow-up was 8.3 years. There were 247 cemented THAs (69%), 105 uncemented THAs (29%) and 6 hybrid THAs (2%).
All studies reported significant improvement in hip function following THA. There were 19 cases of aseptic loosening (5%) at a mean of 8.6 years. Three cases occurred in the uncemented cohort (3%) at a mean of 15.3 years and 16 cases developed in the cemented group (6%) at a mean of 7.5 years (P = 0.2052). There were 27 revisions in the 358 cases (8%) occurring at a mean of 7 years. Six revisions occurred in the uncemented cohort (6%) at a mean of 8.6 years and 21 in the cemented cohort (9%) at a mean of 6.5 years (P = 0.5117).
The findings support the use of THA in patients with Paget’s disease hip arthropathy. The post-operative functional outcome is largely similar to other patients; however, the revision rate is higher with aseptic loosening being the most common reason for revision. Uncemented implants appear to be associated with a lower failure rate, however, there were no modern stem designs fixed using current generation cementing techniques used in the reported studies, and as such, caution is advised when drawing any conclusions.
Core tip: Patients with Paget’s disease commonly develop structural bone deformities in the proximal femur, making total hip arthroplasty (THA) technically demanding. In addition, achieving adequate fixation of hip implants in the hypervascular and often sclerotic bone may prove challenging. This review has shown that, despite its challenging nature, THA can be very successful in terms of improving symptoms and restoring hip function in this unique group of patients. The failure rate, however, appears to be slightly higher than in other patients undergoing a primary total hip replacement. The most common reason for revision surgery is aseptic loosening, and using modern uncemented implants appear to reduce the risk of this occurring.
- Citation: Hanna SA, Dawson-Bowling S, Millington S, Bhumbra R, Achan P. Total hip arthroplasty in patients with Paget’s disease of bone: A systematic review. World J Orthop 2017; 8(4): 357-363
- URL: https://www.wjgnet.com/2218-5836/full/v8/i4/357.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i4.357
Paget’s disease of bone (PDB) is a chronic deforming metabolic disorder characterised by increased osteoclastic bone resorption and subsequent erratic compensatory formation of new woven bone of an abnormal microstructure[1]. British surgeon Sir James Paget first described PDB in 1877 as a chronic inflammation of bone and termed it “osteitis deformans”[2]. The resultant bone is mechanically weaker, larger, less compact, more vascular, and more susceptible to fracture than normal adult lamellar bone[1]. Although the exact aetiology of PDB remains unknown, both genetic and environmental factors have been suggested[3]. PDB is more common in Europe, North America and Australasia than in Asia and Africa. It is thought to result from a slow viral infection occurring in individuals with a genetic predisposition[4]. PBD evolves through three distinct phases: An initial osteolytic phase, a mixed phase with lytic and blastic features, and a final osteoblastic or sclerotic phase[5]. Its prevalence has been shown to increase with age and the most commonly involved sites include the pelvis, femur, spine, skull and tibia[5]. The pelvis and proximal femur are involved in 20%-80% of patients resulting in disabling hip disease[6]. A number of structural bony deformities such as coxa vara, anterolateral femoral bowing and acetabular protrusio are commonly seen in patients with advanced PDB hip arthropathy[3]. When secondary degenerative changes occur in the hip, symptoms may be initially treated with activity and life-style modifications, anti-inflammatory and anti-pagetic medications, functional bracing and physical therapy. If these measures fail, total hip arthroplasty (THA) is indicated to manage significant pain, joint stiffness and deformity. If THA is considered, preoperative treatment with bisphosphonates or calcitonin is thought to reduce the incidence of intraoperative bleeding, heterotrophic ossification and loosening, although no randomised controlled trials exist to support their use[7]. The increased bone turnover and remodelling is associated with elevated levels of serum alkaline phosphatase (ALP), which is used to assess the activity of the PDB and the effectiveness of medical treatment by bisphosphonates[8].
THA in the context of PDB can be a technically challenging procedure because of a number of reasons. The broad spectrum of deformities developing in the hip, including acetabular protrusio, coxa vara and femoral bowing, may hamper dislocation of the hip necessitating a neck cut in-situ. A trochanteric osteotomy may also be required for adequate exposure. A marked deformity of the proximal femur may require a corrective osteotomy to enable adequate femoral component alignment and fixation. The presence of dense sclerotic bone may make reaming and bone preparation extremely difficult. Bone hypervascularity may impair visualisation, require higher than usual fluid and blood replacement, and compromise cement implant fixation. Inability to achieve a dry bone bed for cement interdigitation/micro-interlock may compromise long-term implant fixation[3], which probably explains why the published results of cemented THA in PDB patients appear to be generally poorer than results in other patients[7]. Concerns also exist when using uncemented hip implants in patients with PDB, as the increased bone turnover is believed to predispose to failure of osseointegration and early aseptic loosening in some cases[9].
It is estimated that approximately 3% to 4% of the population over age 50 in the United States are affected by PDB[10]. Although the majority of these patients will not require surgical intervention, those who do, however, represent a unique subset of patients and orthopaedic pathology. When taking into account the exponential increase in the number of THAs performed annually, it can be extrapolated that arthroplasty surgeons will be faced with caring for an increasing number of patients with PDB in the future. It is, therefore, important to recognise the unique problems and challenges inherent to performing THA in patents with PDB. To this end, we therefore performed a systematic review of the literature to determine the method of fixation, failure rates, complication rates and functional outcome of THA in patients with PDB of the hip.
MEDLINE and EMBASE were searched on 1/7/2016 to identify relevant studies in the English literature describing the results of THA in patients with PDB between 1980 and July 2016 in line with the PRISMA statement. Keywords used for the searches were “total hip arthroplasty” or “total hip replacement” and “Paget’s disease”. The bibliographies of all included studies and pertinent reviews were checked carefully for identifying additional studies. We did not contact the corresponding authors to obtain extra data.
Inclusion criteria included all papers, which described the results of THA in patients with PDB published in the English language. Isolated case reports/series with 5 or less patients were excluded. The included articles met the PICO criteria for systematic reviews (Population, Intervention, Comparison and Outcomes).
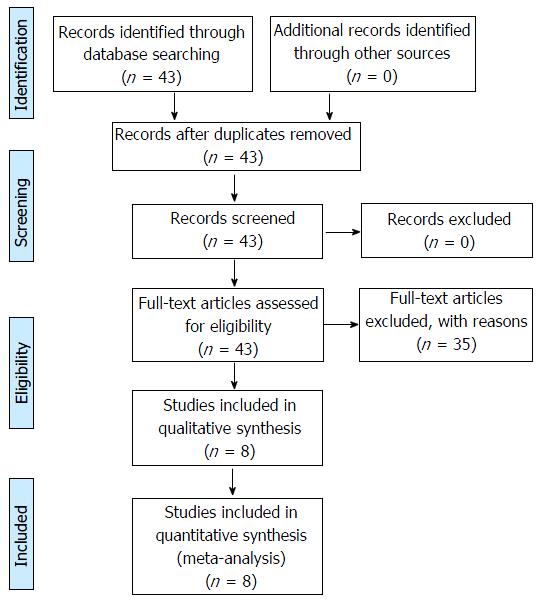
One reviewer (Sammy A Hanna) extracted data through a standardized data collection form, and then another reviewer (Sebastian Dawson-Bowling) checked the data for accuracy. Any inconsistent results were handled by discussion. Data of the number of patients, follow-up period, type of implant, type of fixation, complications, re-operations, revision rate and functional outcome were extracted and entered in a spreadsheet. Figure 1 represents a PRISMA flowchart illustrating the search strategy and number of records screened and included.
Fisher’s exact test was used to compare the incidence of aseptic loosening and revision THA between the uncemented and cemented groups. A P value of < 0.05 was considered statistically significant.
A total of 43 relevant article titles were identified. After reviewing the full text, a total of 8 studies[7,11-17] satisfied the eligibility criteria and the search strategy illustrated in Figure 1. The excluded 35 articles did not meet the PICO criteria. The included 8 studies were small to medium size retrospective case series (n = 19-98). The range of follow-up was 2 to 12.3 years.
All studies were small to medium size retrospective case series (n = 19-98) describing the outcome of THA in patients with PDB of the hip. The range of follow-up in the studies was 2 to 12.3 years.
The studies included 358 THAs performed in patients with a mean age of 70.4 years who were followed-up for a mean of 8.3 years (0.7 to 20). There were 247 cemented THAs (69%), 105 uncemented THAs (29%) and 6 hybrid THAs (2%). The demographics of the patients in the studies are summarised in Table 1.
| Study and country | No. of hips | Age (yr) | Follow-up (yr) | Type of fixation | Approach | Complications (implant related) | Heterotopic ossification (%) | Revision rate (%) | Functional outcome (pre and post op) |
| Merkow et al[11] 1984, United States | 21 | 68.6 (57-80) | 5.2 (2-11.4) | Cemented | Direct lateral (7) Antero-lateral (14) | Aseptic loosening (2) | 52% | 10% | HSS scale: 18 to 30 |
| McDonald et al[12] 1987, United States | 91 | 69.9 (49-85) | 7.2 (0.7-15) | Cemented | Direct lateral (64) Antero-lateral (27) | Aseptic loosening (12) Deep infection (2) Instability (2) Foot drop (1) Nonunion of GT osteotomy (7) | 37% | 15% | HHS: 39 to 83 |
| Ludkowski et al[13] 1990, United States | 37 | 71.5 (60-81) | 7.8 (1-18.4) | Cemented | Direct lateral | Superficial infection (3) | 65% | 0% | HHS: 48.1 to 83.2 |
| Sochart et al[14] 2000, United Kingdom | 98 | 67.4 (51-79) | 10.4 (5.3-20) | Cemented | Direct lateral | Stem fracture (1) Deep infection (1) Instability (1) Aseptic loosening (2) Nonunion of GT osteotomy (1) Foot drop (1) | 29% | 5% | |
| Kirsh et al[15] 2001, Australia | 20 | 72 (62-82) | 5.7 (4-8) | Uncemented (17) Hybrid (3) | Antero-lateral (13) Posterior (7) | Instability (1) | 50% | 0% | HHS: 31 to 88 |
| Parvizi et al[16] 2002, United States | 19 | 71.3 (54-85) | 7 (2-15) | Uncemented | Posterior | Instability (1) | 32% | 0% | HHS: 59.8 to 86.7 |
| Wegrzyn et al[17] 2010, France | 39 | 74.2 (55-89) | 6.6 (2-12) | Uncemented (36) Hybrid (3) | Antero-lateral (36) Posterior (3) | Intra-operative posterior column acetabular fracture (1) Periprosthetic fractures (2) | 56% | 0% | HHS: 54 to 89 |
| Imbuldeniya et al[7] 2014, Australia | 33 | 75 (63-85) | 12.3 (10.3-17) | Uncemented | Posterior | Aseptic loosening/poly wear (4) Periprosthetic fracture (2) | 45% | 18% |
Functional outcome: All studies reported significant improvement in hip function and patient satisfaction following THA. The Harris Hip Score improved by a mean of 40 points post-operatively (27 to 57) in 5 studies[12,13,15-17]. The Hospital for Special Surgery Scale improved from 18 to 30 post-operatively in one study[11].
Aseptic loosening: Overall, there were 19 cases of aseptic loosening in 358 cases (5%) at a mean of 8.6 years (1.5 to 20). Three cases occurred in the uncemented cohort (3%) at a mean of 15.3 years (14 to 17) and 16 cases developed in the cemented group (6%) at a mean of 7.5 years (1.5 to 20) - (P = 0.2052). There was only one case of failure of osseointegration/early subsidence of the femoral stem in the uncemented patients (1%) occurring at 7 mo.
Revisions rate: There were 27 failures requiring revision surgery in the 358 cases (8%) occurring at a mean of 7 years (0.6 to 20). Six revisions occurred in the uncemented cohort (6%) at a mean of 8.6 years (0.6 to 17) and 21 in the cemented cohort (9%) at a mean of 6.5 years (1.5 to 20) - (P = 0.5117). The reasons for failure were aseptic loosening (70%, n = 19), septic loosening (11%, n = 3), periprosthetic fracture (11%, n = 3), femoral stem fracture (4%, n = 1) and instability (4%, n = 1). Table 2 summarises the different complication rates between the cemented and uncemented groups.
| Complication | Cemented THR (n = 247) | Uncemented THR (n = 105) |
| Aseptic loosening | 16 (6) | 3 (3) |
| Septic loosening | 3 (1) | 0 (0) |
| Periprosthetic fracture | 0 (0) | 4 (4) |
| Intra-operative fracture | 0 (0) | 1 (1) |
THA appears to be a generally successful procedure in patients with PDB. The reported post-operative improvement in functional outcome and patient satisfaction is significant in all studies in this review, and is largely comparable to the outcome of THA in other patients[17]. The overall revision rate was 8% at 7 years with aseptic loosening being the main reason for revision (70%). The revision rate was lower in the uncemented patients (6%) at 8.6 years compared with (9%) in the cemented group at 6.5 years and the incidence of aseptic loosening was higher when cemented implants were used (6%), compared with uncemented porous coated implants (3%). Both differences were not statistically significant (P = 0.5117 and 0.2052 respectively). Aseptic loosening also occurred much earlier in the cemented patients (7.5 years vs 15.3 years). These failure rates are slightly higher than those in other patients undergoing THA[18]. According to the Australian National Joint Registry, a revision rate of > 7.5% at 10 years is considered higher than anticipated[19]. It is important to note that the vast majority of cemented THAs in this review included modifications of the Charnely stem coupled with a conventional ultra high molecular weight polyethylene liner and fixed with first/second generation cementing techniques. This may have contributed to the relatively high failure rates[20]. Cementless implants may have a theoretical advantage over cemented ones in the context of PDB. Cement penetration and interdigitation may be limited in Pagetic bone, which is typically sclerotic and more prone to bleeding. In contrast, many authors believe that the altered bone morphology and increased turnover may hamper osseointegration of uncemented implants[7]. Interestingly, there was only one case in the uncemented cohort (1%) where failure of bone ingrowth/osseointegration had occurred. This required revision at 7 mo post index surgery.
The overall reported incidence of heterotopic bone (HO) formation was 46% (29% to 65%). It is unclear how the surgical approach to the hip affects this. It is also unclear as to how best to prevent it in terms of dose and timing of radiation and/or chemoprophylaxis[21,22].
Taking into account the exponential increase in the number of THAs performed annually, it can be extrapolated that arthroplasty surgeons will be faced with caring for an increasing number of patients with PDB in the future. It is, therefore, important to understand the implications of PDB on the medical management of patients, intra-operative technical considerations and the outcomes and complications associated with surgery. When planning to perform THA in a PDB patient, a systematic approach is paramount to ensure optimal outcome. The following pre, intra and post-operative considerations need to be adequately addressed.
Differentiating mechanical joint pain from Pagetic bone pain is important. Diagnostic injections are a useful tool to confirm the intra-articular origin of the hip pain and to rule our concurrent pathology.
Good quality imaging studies including long leg views ± computed tomography (CT) scans to assess bone morphology and extra-articular deformities. This is important to plan surgery, including the need for any extra intra-operative steps such as corrective osteotomy and to choose the appropriate implants.
Review by a cardiologist is recommended to assess cardiac function and the presence of high-output cardiac failure. This will likely have anaesthetic implications and may require optimisation prior to performing the surgery.
Preoperative treatment with bisphosphonates or calcitonin reduces intraoperative bleeding by decreasing disease activity. Anti-pagetic medications should be started at least 6 wk prior to elective surgery. Disease activity can be monitored using ALP serum levels[23].
Pre-operative optimisation of Haemoglobin levels is important to compensate for blood loss intra-operatively. Pre-operative autologous blood donation may also be considered.
Effective blood salvage strategies should be employed including expeditious surgery and the administration of tranexamic acid.
Surgery should be performed through an extensile approach when necessary with liberal soft tissue releases in patients with severe contractures.
Preparation of the femoral side must be performed with caution because standard rasps and reamers may not be effective when used in extremely sclerotic bone. A high-speed burr may be useful to aid in bone preparation. As discussed previously, sclerotic bone may compromise the interdigitation of cement, and uncemented implants may be preferred under these circumstances.
If an uncemented shell is used, it is important to achieve good peripheral rim fit and the use of acetabular screws are recommended to enhance fixation[24].
Concurrent osteotomy to achieve satisfactory femoral component alignment can be difficult. It is advisable to perform the osteotomy in the metaphysis when possible. A previous study has shown that osteotomy performed in a metaphyseal location had a better outcome than those performed through diaphysis[25]. However, the complex nature of the deformity in some of these patients may necessitate diaphyseal, and in some occasions multiplanar osteotomies to achieve a satisfactory correction.
Bisphosphonate treatment should continue if the disease activity high (ALP levels).
It is advisable to administer prophylaxis against HO with preventive measures such as radiation and/or prophylactic drug regimens[21]. The efficacy of indomethacin in preventing HO is well documented[26]. The most common treatment is to give 25 mg three times a day for five to six weeks. Several studies have shown the efficacy of radiation therapy in reducing the incidence of HO following lower limb arthroplasty. The most appropriate dose regimen appears to be 7 to 8 Gy given as a single fraction either < 4 h pre-operatively or < 72 h post-operatively[26].
The main limitation of this review is that it included studies dating back to 1980, with three of the eight papers included being published in 1990 or earlier. Only two articles were published in the last 10 years. This potentially has an impact the results as dated implants and techniques have poorer survivorship. However, although Paget’s disease is fairly common (3%-4% of the United States population above the age of 50 are affected)[10], very limited new information has been published on the topic. With the exponential annual increase of THAs, most arthroplasty surgeons will care for patients with Paget’s disease at some point, which makes this review relevant to clinical practice, especially by highlighting the potential challenges and expected outcomes of THA in this unique group of patients.
The findings of this review support the use of THA to alleviate debilitating hip pain and functional limitation in PDB patients with hip arthropathy. Post-operative patient satisfaction and functional improvement is similar to other patients, however, the revision rate is higher with aseptic loosening being the most common reason for revision. Uncemented implants appear to be associated with a lower failure rate. However, there are no studies reporting on the use of modern stem designs fixed using current generation cementing techniques in PDB patients, so caution is advised when drawing any conclusions.
Paget’s disease is a fairly common disorder, which affects approximately 3% to 4% of the United States population over the age of 50. Although the majority of these patients will not require surgical intervention, those who do, however, represent a unique subset of patients and orthopaedic pathology. Hip involvement is common and performing total hip arthroplasty (THA) in this group of patients is technically demanding. There are three main issues the surgeon needs to address during the procedure: How to deal with the structural deformities present in the hip, how to achieve adequate implant fixation in the hypervascular and sclerotic bone, and how to manage blood loss intra-operatively. This review attempts to answer these questions based on current evidence.
The optimal method of fixation of hip implants in patients with Paget’s disease is frequently debated amongst hip surgeons with no clear consensus. The role of Bisphosphonate therapy peri and post-operatively in reducing blood loss is also a controversial issue.
The review supports the use of THA in patients with Paget’s disease. The functional benefit after the procedure is similar to other patients undergoing a primary THA. However, the authors found a slightly higher revision rate in tis group of patients, with aseptic loosening being the most common reason for revision. Although uncemented implants appear to be associated with a lower failure rate, however, they did not find any studies evaluating the role of modern polished tapered cemented stem designs in patients with Paget’s disease. Caution is therefore advised when drawing any conclusions.
The results highlight the need for a structured, planned and multidisciplinary approach when managing patients with Paget’s disease of bone undergoing THA in order to optimise outcome and reduce the risk of complications.
This is a systematic review on THA in patients with Paget’s disease of bone. The introduction is well written and convincing. This systematic review seems to be highly original and no systematic review currently exists on this topic; thus, this manuscript is timely.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gong JP, Hasegawa M, Korovessis P S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Rebel A, Basle M, Pouplard A, Malkani K, Filmon R, Lepatezour A. Bone tissue in Paget’s disease of bone. Ultrastructure and Immunocytology. Arthritis Rheum. 1980;23:1104-1114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 72] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Paget J. On a Form of Chronic Inflammation of Bones (Osteitis Deformans). Med Chir Trans. 1877;60:37-64.9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 329] [Cited by in F6Publishing: 348] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 3. | Lewallen DG. Hip arthroplasty in patients with Paget’s disease. Clin Orthop Relat Res. 1999;243-250. [PubMed] [Cited in This Article: ] |
| 4. | Rebel A, Basle M, Pouplard A, Malkani K, Filmon R, Lepatezour A. Towards a viral etiology for Paget’s disease of bone. Metab Bone Dis Relat Res. 1981;3:235-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Lander PH, Hadjipavlou AG. A dynamic classification of Paget’s disease. J Bone Joint Surg Br. 1986;68:431-438. [PubMed] [Cited in This Article: ] |
| 6. | Guyer PB, Chamberlain AT, Ackery DM, Rolfe EB. The anatomic distribution of osteitis deformans. Clin Orthop Relat Res. 1981;156:141-144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Imbuldeniya AM, Tai SM, Aboelmagd T, Walter WL, Walter WK, Zicat BA. Cementless hip arthroplasty in Paget’s disease at long-term follow-up (average of 12.3 years). J Arthroplasty. 2014;29:1063-1066. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Delmas PD, Meunier PJ. The management of Paget’s disease of bone. N Engl J Med. 1997;336:558-566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 205] [Cited by in F6Publishing: 207] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Lusty PJ, Walter WL, Walter WK, Zicat B. Cementless hip arthroplasty in Paget’s disease at medium-term follow-up (average of 6.7 years). J Arthroplasty. 2007;22:692-696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | American Academy of Orthopaedic Surgeons. Paget’s Disease of Bone. Available from: http://orthoinfo.aaos.org/topic.cfm?topic=a00076. [Cited in This Article: ] |
| 11. | Merkow RL, Pellicci PM, Hely DP, Salvati EA. Total hip replacement for Paget’s disease of the hip. J Bone Joint Surg Am. 1984;66:752-758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 64] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | McDonald DJ, Sim FH. Total hip arthroplasty in Paget’s disease. A follow-up note. J Bone Joint Surg Am. 1987;69:766-772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 62] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Ludkowski P, Wilson-MacDonald J. Total arthroplasty in Paget’s disease of the hip. A clinical review and review of the literature. Clin Orthop Relat Res. 1990;160-167. [PubMed] [Cited in This Article: ] |
| 14. | Sochart DH, Porter ML. Charnley low-friction arthroplasty for Paget’s disease of the hip. J Arthroplasty. 2000;15:210-219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Kirsh G, Kligman M, Roffman M. Hydroxyapatite-coated total hip replacement in Paget’s disease: 20 patients followed for 4-8 years. Acta Orthop Scand. 2001;72:127-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Parvizi J, Schall DM, Lewallen DG, Sim FH. Outcome of uncemented hip arthroplasty components in patients with Paget’s disease. Clin Orthop Relat Res. 2002;127-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Wegrzyn J, Pibarot V, Chapurlat R, Carret JP, Béjui-Hugues J, Guyen O. Cementless total hip arthroplasty in Paget’s disease of bone: a retrospective review. Int Orthop. 2010;34:1103-1109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Mariconda M, Galasso O, Costa GG, Recano P, Cerbasi S. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011;12:222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 19. | Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA 2011; . [Cited in This Article: ] |
| 20. | Bjørgul K, Novicoff WM, Andersen ST, Brevig K, Thu F, Wiig M, Ahlund O. The Charnley stem: clinical, radiological and survival data after 11-14 years. Orthop Traumatol Surg Res. 2010;96:97-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Ferguson DJ, Itonaga I, Maki M, McNally E, Gundle R, Athanasou NA. Heterotopic bone formation following hip arthroplasty in Paget’s disease. Bone. 2004;34:1078-1083. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Iorio R, Healy WL. Heterotopic ossification after hip and knee arthroplasty: risk factors, prevention, and treatment. J Am Acad Orthop Surg. 2002;10:409-416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 140] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83:1032-1045. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 887] [Cited by in F6Publishing: 947] [Article Influence: 59.2] [Reference Citation Analysis (0)] |
| 24. | Parvizi J, Klein GR, Sim FH. Surgical management of Paget’s disease of bone. J Bone Miner Res. 2006;21 Suppl 2:P75-P82. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Parvizi J, Frankle MA, Tiegs RD, Sim FH. Corrective osteotomy for deformity in Paget disease. J Bone Joint Surg Am. 2003;85-A:697-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Board TN, Karva A, Board RE, Gambhir AK, Porter ML. The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg Br. 2007;89:434-440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |