Published online Feb 18, 2017. doi: 10.5312/wjo.v8.i2.170
Peer-review started: May 11, 2015
First decision: July 10, 2015
Revised: November 11, 2016
Accepted: November 27, 2016
Article in press: November 29, 2016
Published online: February 18, 2017
To determine if complete, split casts and backslabs [plaster of Paris (POP) and fiberglass] generate different intracast pressures and pain.
Increased swelling within casts was modeled by a closed water system attached to an expandable bag placed directly under different types of casts applied to a healthy lower limb. Complete fiberglass and POP casts, split casts and backslabs were applied. Twenty-five milliliter aliquots of saline were injected into the system and the generated intracast pressures were measured using a sphygmomanometer. The subject was blinded to the pressure scores to avoid bias. All casts were applied to the same right limb on the same subject to avoid the effects of variations in anatomy or physiology on intracast pressures. Pain levels were evaluated using the Visual Analogue Score after each sequential saline injection. Each type of cast was reapplied four times and the measurements were repeated on four separate occasions. Sample sizes were determined by a pre-study 90% power calculation to detect a 20% difference in intracast pressures between cast groups.
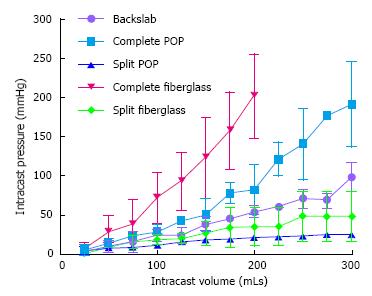
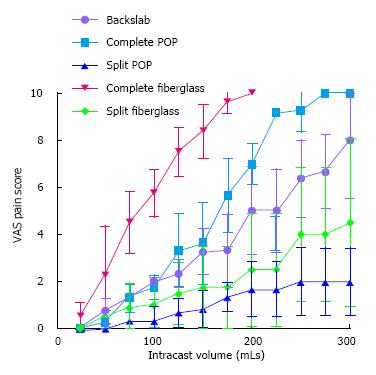
A significant difference between the various types of casts was noted when the saline volume was greater than 100 mL (P = 0.009). The greatest intracast pressure was generated by complete fiberglass casts, which were significantly higher than complete POP casts or backslabs (P = 0.018 and P = 0.008 respectively) at intracast saline volumes of 100 mL and higher. Backslabs produced a significantly lower intracast pressure compared to complete POP only once the saline volume within casts exceeded 225 mL (P = 0.009). Intracast pressures were significantly lower in split casts (P = 0.003). Split POP and fiberglass casts produced the lowest intracast pressures, even compared to backslabs (P = 0.009). Complete fiberglass casts generated the highest pain levels at manometer pressures of 75 mmHg and greater (P = 0.001). Split fiberglass casts had significantly reduced pain levels (P = 0.001). In contrast, a split complete POP cast did not produce significantly reduced pain levels at pressures between 25-150 mmHg. There was no difference in pain generated by complete POP and backslabs at manometer pressures of 200 mmHg and lower.
Fibreglass casts generate significantly higher intracast pressures and pain than POP casts. Split casts cause lower intracast pressures regardless of material, than complete casts and backslabs.
Core tip: Little information is available regarding whether different lower limb casts generate different intracast pressures and pain during swelling, increasing the risk of compartment syndrome. Increased swelling within casts was modeled by a closed water system attached to an expandable bag placed directly under different types of casts. Our study suggests that split casts generate lower intracast pressures than backslabs, which are traditionally thought to accommodate swelling better. Fibreglass casts generate significantly higher intracast pressures and pain levels than plaster of Paris casts. Judicious use of complete casts, particularly fiberglass, and backslabs may be advisable for lower limb immobilisation.
- Citation: Chaudhury S, Hazlerigg A, Vusirikala A, Nguyen J, Matthews S. Lower limb intracast pressures generated by different types of immobilisation casts. World J Orthop 2017; 8(2): 170-177
- URL: https://www.wjgnet.com/2218-5836/full/v8/i2/170.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i2.170
It is common practice to apply lower limb casts to manage non-displaced fractures, following lower limb surgery or the temporary stabilisation of ankle fractures awaiting surgery so as to maintain a plantar grade position and to prevent contracture. Charnley originally described the principle of three-point loading of casts in the management of fractures[1]. Fractures and subsequent immobilization with a constraining cast are associated with a potentially devastating risk of compartment syndrome, which results from elevated pressures within a confined space that results in occlusion of the arterial blood supply to muscles. Consequently it has become usual practice to apply backslabs instead of complete casts to obviate this risk. Casts can be applied either as backslabs, or as complete casts that may or may not be split. Splitting of casts is thought to allow for swelling, although they are no longer able to provide three point fixation. Clinical experience from the senior author has suggested that backslabs can also be associated with pain and compartment syndrome.
Previous studies have demonstrated that skin surface pressure under a cast correlates to intracompartmental pressure[2]. There has been no detailed analysis to date of the effect of swelling on intracast pressures generated by backslabs or different commonly utilized casts materials applied as complete casts, and whether splitting the cast alleviates these pressures. In view of the increased risk of pain and compartment syndrome following fractures and subsequent immobilization with a cast, it is important to address whether different casting materials and types vary in their ability to accommodate swelling.
Backslabs are commonly applied to the acutely fractured limb as a temporizing measure to provide splintage and prevent displacement. This modality is employed on the assumption that the backslab will accommodate swelling, whereas application of a complete cast is thought to constrain any ensuing swelling. The effects of complete casts on generating intracast pressures within the upper limb have been investigated in a small number of studies, but have not been investigated in such detail in the lower limb. Younger et al[3] compared the cast pressures associated with forearm plaster of Paris (POP) backslabs and complete POP casts that were split with different methods. The authors concluded that a split and spread cast was better able to accommodate intracompartmental swelling compared to backslabs. A study by Moir et al[4] investigating intracast pressures in distal radius fractures showed that intracast pressures fall over the first week as swelling subsides. Interestingly, they demonstrated that a small immediate pressure rise is recorded as soon as the backslab is completed, even if completion occurs as late as 14 d. Another study using encircling distal radius plasters that were applied post manipulation of Colles fractures, failed to show any sustained increase in pressure. Despite this, the authors advocate that this technique is to be avoided and proposed a U-slab as a more favourable option in order to avoid the risk of Volkmann’s ischaemic contracture[5].
Split casts have been advocated by many as an alternative to backslabs, allowing sufficient compliance for swelling whilst retaining enough rigidity to support the fracture. A single split in cast in animal study was shown to reduce cast pressure by 65%[6]. Weiner et al[7] investigated the effect of bivalving casts and spreading each side by approximately half a centimeter, and subsequently measured the effects on intramuscular pressures in lower leg anterior and posterior compartments in healthy volunteers. It was reported that bivalving casts significantly reduced the pressures by 47% and 33% in the anterior and posterior compartment respectively (P < 0.05).
Two of the most commonly used materials for casts are POP and fiberglass; differences in their mechanical properties are well documented. Fibreglass is more expensive and less easy to mould, however it is lighter and less permeable to water than POP. This study addressed whether different types of commonly utilized plaster materials for forming lower limb casts generate different surface pressures. As backslabs concentrate any pressures over a smaller surface area, we hypothesized that backslabs may generate higher intracast pressures than complete casts.
The primary aim of this study was to evaluate the intracast pressures generated by different types of commonly used casts used to immobilize lower limb fractures, such as a complete POP or fiberglass casts, and how they compared to POP backslabs. This study also assessed whether splitting the casts significantly reduced the intracast pressures. A secondary aim was to ascertain whether there were differences in subjective pain levels associated with intracast pressure changes generated by different cast materials based on the senior author’s experience of compressive pain in postoperative patients being immediately relieved by removal of the back slab. Our working null hypothesis was that there is no difference in the intracast pressures or pain generated by different complete casts or backslabs. Our second null hypothesis was that split complete casts would not have reduced intracast pressures or associated pain levels compared to complete casts.
This study modeled increased swelling within casts that may occur after lower limb injuries or surgery. A closed water system circuit attached to a 1-L expandable bag (Figure 1) was placed directly under different types of casts that had been applied to a healthy right lower limb (Figure 2). Intracast pressures were measured from the right leg for all of the readings, with the ankle in a neutral position with the knee extended while the subject rested on an examination bed. An intravenous giving set was connected to the emptied bag with a three-way tap. The three-way tap was connected to a sphygmomanometer through one portal and a 50 mL syringe through another portal, with a Luer lock used to secure all lines. Twenty-five milliliter aliquots of saline were injected into the system and the intracast pressures were directly measured using a sphygmomanometer (Figure 3). Measurements were started after an initial injection of 25 mL of saline, which were increased in increments of 25 mL until a total of 300 mL of saline had been injected. Two commonly utilized cast materials, fibreglass and POP were applied to the healthy lower limb before measurements were taken in a random order. The subject was blinded to the pressure scores in order to avoid bias.
During each pressure reading, a subjective assessment of any pain was also made using the Visual Analogue Score (VAS). The VAS score ranges from 1 to 10, with 10 indicating the most severe pain. Between each recording, the system was fully drained of all liquid before recommencing the next casting. The sphygmomanometer was returned to zero in between castings. The measurements were terminated early before 300 mL had been injected if the subject reported a VAS score of 10 or when three identical consecutive pressure readings were measured after injection of sequential 25 mL aliquots. Each type of cast was reapplied four times and the entire measurement process was repeated on four separate occasions. A pre-study power calculation based upon pilot data determined that n = 4 was sufficient to achieve 90% power to detect a 20% difference in intracast pressures between different cast groups, with alpha = 0.05. In order to reduce the effects of bias or multiple castings on VAS pain scores, a random order was selected for application of the different cast materials to try to reduce variability.
A single healthy subject with no history of lower limb trauma was fitted with sequential casts. All casts were applied to the same right limb on the same subject to avoid the effects of any variations in anatomy or physiology on intracast pressures that may arise from using different subjects. The subject had no previous experience of any casts.
In order to reduce variability in application techniques, the plastering for the different cast groups was carried out in exactly the same manner by a single orthopaedic plaster technician with over 15 years of experience. The expandable bag was placed on the anterolateral aspect of the right calf. Marks on the calf delineated exactly where the bag should be placed for all castings and the saline bag was taped in place to assist reproducible placement. A 4-inch stockinette was used, followed by 2 layers of Velband® (Velband®, Smith and Nephew, Hull, United Kingdom) before the top layers of the casts were applied using a standard technique. For the POP casts, 3 rolls (Gypsona®, BSN Medical, France) were used per cast and for the fibreglass casts (BSN Medical) 4 rolls were utilized. When splitting of the cast was required, a single medial split was made along the medial edge of the tibia and the cast was cut to skin. Backslabs were applied with a single slab of POP posteriorly, consisting of 4 layers of POP. The backslabs were further reinforced on the medial and lateral sides, as per standard local protocol. The casts were allowed to harden fully before the data was collected from the lower leg.
Any differences between the 5 cast groups were assessed using a repeated measures ANOVA with a Bonferroni multiple comparison test to compare individual cast types and account for potential type-I errors associated with multiple statistical tests. All tests were two tailed and a significance level of P < 0.05 was set. GraphPad Prism 5 (Graph Pad Software, LaJolla, California) software was used for statistical analysis.
The results indicated that the introduction of fluid into the different casts generated different intracast pressures (Table 1). A significant difference between the various types of casts was noted when the saline volume was greater than 100 mL (P = 0.009, Figure 4). The greatest intracast pressure was measured from complete fiberglass casts and this was significantly greater than complete POP casts (P = 0.018) and backslabs (P = 0.008) at intracast saline volumes of 100 mL and higher. Backslabs produced a significantly lower intracast pressure compared to complete POP only once the saline volume within casts exceeded 225 mL (P = 0.009).
| Mean | Std. deviation | Std. error | 95%CI for mean | Minimum | Maximum | P-value | |||
| Lower bound | Upper bound | ||||||||
| Intracast pressure (mmHg) | Backslab | 47.05 | 31.8 | 4.79 | 37.38 | 56.71 | 2 | 120 | < 0.001 |
| Full POP | 72.28 | 60.3 | 9.66 | 52.73 | 91.83 | 2 | 230 | ||
| Split POP | 17.15 | 7.53 | 1.29 | 14.52 | 19.77 | 1 | 28 | ||
| Fibreglass | 82.73 | 67.01 | 12.23 | 57.71 | 107.76 | 2 | 240 | ||
| Split Fibreglass | 26.58 | 21.33 | 3.25 | 20.02 | 33.15 | 0 | 70 | ||
| Total | 47.88 | 48.48 | 3.52 | 40.94 | 54.82 | 0 | 240 | ||
| Pain | Backslab | 3.99 | 2.9 | 0.44 | 3.11 | 4.87 | 0 | 10 | < 0.001 |
| (VAS | Full POP | 4.77 | 3.73 | 0.6 | 3.56 | 5.98 | 0 | 10 | |
| score) | Split POP | 1.04 | 1.06 | 0.18 | 0.67 | 1.41 | 0 | 3 | |
| Fibreglass | 5.8 | 3.37 | 0.62 | 4.54 | 7.06 | 0 | 10 | ||
| Split Fibreglass | 1.9 | 2.09 | 0.32 | 1.25 | 2.54 | 0 | 7 | ||
| Total | 3.43 | 3.24 | 0.24 | 2.97 | 3.9 | 0 | 10 | ||
Split POP casts generated the lowest intracast pressure of all the different casts. Split POP casts produced significantly less intracast pressure compared to backslabs when saline volumes were greater than 100 mL. At this volume of 100 mL, a significant reduction in intracast pressures were noted after splitting of both the complete POP and complete fiberglass casts (P = 0.003). Once both types of complete casts had been split, there was no significant difference between the two different groups of split casts.
The effects of different types of casts on pain levels were also investigated. Fiberglass casts generated significantly greater pain levels when saline volumes were as low as 75 mL (P = 0.001) and continued to produce the highest pain levels at all measured volumes between 75-200 mL (P < 0.05, Figure 5). Splitting the complete fiberglass cast at 75 mL of saline significantly reduced pain levels (P = 0.001) and this trend was also seen between 100-200 mL of saline (P < 0.001). In contrast, splitting a complete POP cast did not significantly reduce the pain levels at saline volumes between 25-150 mL. When the intracast volumes were set at 175 mL, splitting the complete POP cast does result in a significant reduction in pain (P = 0.013). This trend towards no reduction in pain is also seen at saline volumes between 200-250 mL (P < 0.003).
Closed splinting techniques with casts are commonly used in orthopaedics as a temporizing management technique for both conservatively and operatively treated lower limb injuries to prevent secondary equinus deformities. POP casts are frequently applied in the immediate acute setting, and these are often later changed to synthetic casts. Controversies exist between the ideal cast material and application mode. Important material properties that need to be considered for orthopaedic splints include strength, stiffness, compliance and weight. If constrictive casts increase the extra or intracast pressure in swollen lower limbs carries, they can potentially contribute to compartment syndrome, as well as other complications such as increasing pain, skin necrosis, circulatory compromise and fracture displacement. Thus, minimizing pressures associated with casts is imperative.
This study found that different casts produce different intracast pressures and fiberglass casts generate significantly higher intracast pressures than POP casts, rejecting our null hypothesis. These findings are consistent with results from published studies[8]. Fiberglass casts are frequently utilized to form casts due to a number of advantageous material properties, including its lighter weight compared to POP. The time taken to reach maximum strength is much shorter in fiberglass compared to POP[9] and the strength and stiffness achieved with fiberglass has been shown to be greater than POP[10,11]. The polyurethane in standard fiberglass undergoes a chemical change during hardening[12]. We hypothesize that fiberglass casts generated higher intracast pressures due to their higher recoil element, which is not applicable to POP, and their lower compliance[8]. Compliance between fiberglass and POP has been compared in previous studies. Fiberglass was shown to require a greater volume change to generate the same pressure rise during the initial stages of swelling[13]. However, once a certain pressure threshold had been exceeded, fiberglass pressures were found to rise steeply with less volume change. Our study found that once the intracast volume of saline exceeded 75 mL, fiberglass casts produced a rapid rise in intracast pressures. Stress relaxation has been demonstrated in both POP and fiberglass and attributed to the composite nature of fiberglass and POP, as well as the mesh design. These properties are presumed to allow relaxation within the materials over a constant volume distention, ultimately allowing pressures to reduce. Clinically this is advantageous as otherwise peak pressures generated by both materials would be much higher and sustained for longer periods[13]. In view of the persistently higher pressures demonstrated by fiberglass casts in this study, the authors advocate POP casts over fiberglass for injured lower limbs in the acute phase, particularly for the first 24 h.
Backslabs were associated with significantly higher intracast pressures than split POP casts at saline volumes of greater than 125 mL, suggesting that split POP generate less intracast pressure when the swelling and volume rises within a cast. Interestingly, these results suggest that split POP are more effective than backslabs at avoiding the generation of high intracast pressures when the swelling and volume of saline within the cast increases. Ultimately, split POP casts may be a safer choice for casting technique in situations when swelling is expected, such as immediately following fractures or post-operatively. According to our results, backslabs were associated with lower intracast pressures in comparison to complete fiberglass or POP casts. Despite the fact that backslabs only cover a smaller surface area compared to complete casts, backslabs do not concentrate the intracast pressures and thus our null hypothesis was rejected. This study supports the widely assumed theory that backslabs are better able to facilitate acute swelling and supports the use of backslabs immediately after injury or after surgery when further swelling is anticipated. While backslabs may accommodate further swelling, this must be balanced against the risk that once the swelling reduces, backslab provide less resistance to deforming forces compared to complete casts which ultimately increases the potential for fracture displacement. While Charnley’s three-point loading of casts for the management of fractures is a commonly accepted and applied principle[1], this appears to be more difficult to achieve with backslabs. Wytch et al[14] used intracast pressure measuring techniques to demonstrate that loading in backslabs is low and although this is improved with moulding, they did not find evidence of Charnley’s three-point loading principle.
Issues of generating high intracast pressures are applicable to both upper and lower limb fractures, as the former are also often managed with an initial backslab that may later be converted into a complete cast. As an example, a common preliminary method of managing Colles fracture includes application of an initial dorsoradial plaster that is later completed to a complete below elbow cast once a sufficient time period has elapsed and the risk of significant swelling is assumed to have diminished.
Splitting the casts resulted in a universal decrease in intracast pressures, regardless of cast material. However the reduction in cast pressures following splitting was more marked in fiberglass than in POP casts. This study suggests that splitting complete casts, particularly fiberglass casts, may be advisable in clinical scenarios associated with acute limb swelling. This difference may be attributable to the greater ability of fiberglass to recoil at the site of splitting the cast.
Measuring compliance of material and pressures generated from encasement with a cast has been investigated with a variety of different methodologies. This study utilized a saline bladder system rather than an air-filled system as it is easier to detect any leaks. Sensors can directly be applied to the skin to measure surface cast pressures, however they do not allow a spectrum of recordings to be carried out in a dynamic volumetric distension system, as was permitted by our study design. A study used a modified Sengstaken tube to investigate intracast pressures generated within backslabs that had been applied following surgical fixation of ankle fractures in 15 patients[15]. The mean pressure rise reported was 3.4 mmHg and the maximum measured pressure was 20.2 mmHg. The study also showed that maximum pressure peaked within 2 h of surgical fixation. This study measured a much wider range of manometer and surface pressures.
A number of limitations are associated with this study. A healthy subject was used and a saline system was used to emulate soft tissue swelling that may occur in an acutely fractured lower limb and the authors appreciate that this is not a direct measurement of compartment pressure. Previous studies investigating intracast pressures have found lower readings in healthy subjects compared to injured patients[5]. However, the aim of this study was to investigate the effects of soft tissue swelling on intracast pressures and this could be achieved using a healthy subject. This study cannot extrapolate how intracast pressures are related to intracompartmental pressures or compartment syndrome, even though a strong correlation between extra and intracompartmental pressures has been previously demonstrated[16]. The direct effect of different casts on intracompartmental pressures was beyond the scope of this study and ideally should be addressed by future studies. All measurements in this study were performed on a single subject to avoid inter-subject variations in pain threshold, thus avoiding potential bias. However, there was potential for the subject to become sensitized to pain, following repeated measurements after multiple cast applications. To avoid this, different casts were applied in a random order. Although the subject was blinded to pressure readings, the subject would have been aware of the increase in pressure as the study progressed with each individual cast and may have anticipated increasing pain.
This study only investigated the pressures generated immediately after cast application and did not model any delayed increases that may occur following swelling of fractured limbs as a healthy limb was utilized. Patrick et al[5] measured intracast pressures in healthy subjects and patients with Colles fractures. In the Colles fracture group they observed a first and second peak phenomenon, whereby pressures rose immediately after application of the plaster and then rose again after an average of 13 h before gradually declining to reach a resting value after 72 h. The first peak was observed in healthy subjects however the second peak was not and the authors concluded that the second peak was due to delayed swelling associated with the fracture. Attempts were made to keep the infusion rate constant, but this was not verified by any measurements. A previous study showed using pressure volume dynamics that fluid infused at a faster rate led to a quicker pressure rise and decreased accommodation in POP and fibreglass. Interestingly, the decreased stiffness observed in the two materials at slower infusion rates was more apparent at lower pressures in the POP group than the fibreglass[13].
External splinting is widely utilized in orthopaedics and trauma to stabilize fractures or support surgical constructs. Casts are associated with rare but potentially devastating complications of compartment syndrome and skin necrosis. This study demonstrated that as the volume within a cast rose, complete fibreglass casts generated significantly higher intracast pressures than complete POP casts. Complete fiberglass and POP casts were associated with significantly greater pressures than backslabs. Splitting casts confirmed a universal decrease in intracast pressures regardless of the material utilized. Backslabs are traditionally thought to allow greater swelling and produce lower pressures within the cast, yet our findings suggest that split POP produces the lowest intracast pressures and may be the most appropriate casting technique in situations where swelling is anticipated. Thus judicious use of complete casts, particularly fiberglass casts may be advisable in cases where significant swelling is anticipated in fractured limbs. The application of split POP casts in the immediate acute setting may be more beneficial in high-risk patients such as neuropathic, diabetic and unconscious patients. Further research is required to determine the pressure rises associated with a broader range of casts such as soft casts and hybrid fiberglass reinforced POPs as well as whether the stockinette or Velband® generate higher constraint and pressures than other materials.
Acknowledgements to Claire Granville. Trauma Unit, John Radcliffe Hospital, University of Oxford, Oxford, OX3 7LD, United Kingdom.
Lower limb fractures with subsequent immobilisation with a cast are associated with a potential risk of developing compartment syndrome.
Different types of casts could potentially produce different intracast pressures which could ultimately increase intracompartmental pressures. There has been no detailed analysis to date of the effect of swelling on intracast pressures generated by backslabs or different commonly utilized cast materials applied as complete casts, and whether splitting the cast alleviates the pressures.
Introduction of fluid into different casts was used as a surrogate for volume expansion. This generated different intracast pressures. When increase in saline volume was greater than 100 mL, a significant difference in intracast pressures was observed between various types of casts. Intracast pressures were significantly greater in complete fibreglass casts in comparison to complete plaster of Paris (POP) casts and backslabs. Backslabs produced a significantly lower intracast pressure compared to complete POP casts only once the saline volume within casts exceeded 225 mL. Split POP casts generated the lowest intracast pressures of all casts and less than backslabs when saline volume exceeded 100 mL. Splitting casts reduced intracast pressures of both POP casts and fibreglass casts. When split, no significant difference was observed in intracast pressures between the two types of split casts. Fibreglass casts produced greater pain levels when saline volume was as low as 75 mL and it continued to produce the highest pain levels. The data indicates that split fiberglass casts were associated with significantly less pain than complete fiberglass casts. Splitting the complete POP cast did not significantly reduce the pain levels until saline volume was 175 mL.
Judicious use of complete casts, particularly fibreglass casts and backslabs may be advisable for lower limb immobilisation. The use of a split cast for lower limb immobilisation in the immediate acute setting may be more beneficial for high risk patients such as neuropathic, diabetic and unconscious patients.
POP cast: Plaster of Paris is a hemihydrated calcium sulfate material which solidifies when mixed with water. It is used as a cast for immbolisation of a fractured limb. Fibreglass is a synthetic alternative to the traditional POP. The fibreglass bandages are impregnated with a quick setting water-soluble resin. It is a lighter, water proof cast used for immobilisation of fractured limbs. Backslabs are partial casts applied to the posterior aspect of the limb. They are held onto the limb with a bandage.
This is a good manuscript on a clinical relevant issue. Style and study design are fine.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Labek G S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Charnley J. The closed treatment of common fractures. Br J Surg. 1957;191:299. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Uslu MM, Apan A. Can skin surface pressure under a cast reveal intracompartmental pressure? Arch Orthop Trauma Surg. 2000;120:319-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Younger AS, Curran P, McQueen MM. Backslabs and plaster casts: which will best accommodate increasing intracompartmental pressures? Injury. 1990;21:179-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Moir JS, Wytch R, Ashcroft GP, Neil G, Ross N, Wardlaw D. Intracast pressure measurements in Colles’ fractures. Injury. 1991;22:446-450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Patrick JH, Levack B. A study of pressures beneath forearm plasters. Injury. 1981;13:37-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Garfin SR, Mubarak SJ, Evans KL, Hargens AR, Akeson WH. Quantification of intracompartmental pressure and volume under plaster casts. J Bone Joint Surg Am. 1981;63:449-453. [PubMed] [Cited in This Article: ] |
| 7. | Weiner G, Styf J, Nakhostine M, Gershuni DH. Effect of ankle position and a plaster cast on intramuscular pressure in the human leg. J Bone Joint Surg Am. 1994;76:1476-1481. [PubMed] [Cited in This Article: ] |
| 8. | Marson BM, Keenan MA. Skin surface pressures under short leg casts. J Orthop Trauma. 1993;7:275-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Berman AT, Parks BG. A comparison of the mechanical properties of fiberglass cast materials and their clinical relevance. J Orthop Trauma. 1990;4:85-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Mihalko WM, Beaudoin AJ, Krause WR. Mechanical properties and material characteristics of orthopaedic casting material. J Orthop Trauma. 1989;3:57-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Charles MN, Yen D. Properties of a hybrid plaster-fibreglass cast. Can J Surg. 2000;43:365-367. [PubMed] [Cited in This Article: ] |
| 12. | Mohler LR, Pedowitz RA, Byrne TP, Gershuni DH. Pressure generation beneath a new thermoplastic cast. Clin Orthop Relat Res. 1996;262-267. [PubMed] [Cited in This Article: ] |
| 13. | Deshpande SV. An experimental study of pressure-volume dynamics of casting materials. Injury. 2005;36:1067-1074. [PubMed] [Cited in This Article: ] |
| 14. | Wytch R, Ashcroft P, Kalisse CG, Neil G, Ross N, Ward D. Interface pressures in below elbow casts. Clin Biomech (Bristol, Avon). 1991;6:25-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Bowyer GW, Iu M, Reynard JM. Pressure in plaster backslabs after surgery for ankle fractures. Injury. 1993;24:121-122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Davids JR, Frick SL, Skewes E, Blackhurst DW. Skin surface pressure beneath an above-the-knee cast: plaster casts compared with fiberglass casts. J Bone Joint Surg Am. 1997;79:565-569. [PubMed] [Cited in This Article: ] |