Published online Dec 18, 2017. doi: 10.5312/wjo.v8.i12.929
Peer-review started: August 25, 2017
First decision: September 20, 2017
Revised: October 20, 2017
Accepted: November 8, 2017
Article in press: November 8, 2017
Published online: December 18, 2017
To measure the sensitivity and specificity of the cup version assessment by using only anteroposterior hip and pelvis views, evaluate the incidence of inadequate cup version in patients with repeated dislocations after total hip arthroplasty (THA).
Radiographic retrospective analysis of 2 groups of patients, with follow up of 6-60 mo, after undergoing primary THA. First group of 32 patients (20 female, 12 male) with unilateral THA (32 hips) required early revision arthroplasty for reasons of dislocation. The mean age and mode were 59 (from 38 to 83) and 66 ages respectively. The average body mass index (BMI) was 24.2 (from 17.7 to 36.3), mode 23.9. Second group was consisted of 164 patients (101 female, 63 male) without dislocations during the follow-up period (170 hips). Among them 6 patients required bilateral THA. The mean age was 60 (from 38 to 84) and mode 59. BMI was 24.8 (17.2-36.8), mode 25.2. Clinical significance of the cup anteversion sign was estimated with cross tabulation 2 × 2.
The value of the χ2 yates was 10.668 (P < 0.01). Sensitivity of SAI (sign of anteversion insufficiency) was 29% (95%CI: 9%-46%), and specificity was 92% (95%CI: 88%-96%). Relative risk of dislocation in patients with SAI was 3.4 (95%CI: 1.8-6.3).
This method provides the surgeons with the ability to perform a reliable and simple qualitative assessment of the acetabular component version. It can be useful during patient examination with early loosening of the implant, dislocations, and impingement. Additionally, it can provide necessary information during planning of revision surgery, especially when considering question about cup replacement, although final assessment of the cup position should be done with a computed tomography scan.
Core tip: The acetabular cup position is a crucial factor of normal function and implant survival. Several methods to determine cup anteversion are described. Among them are mathematical methods based on a standard anteroposterior (AP) view, modifications of a cross-table lateral views, and computed tomography-scan. Latter two methods are not always available or practical in outpatient setting. The purpose of our study was to estimate sensitivity, specificity of the cup version assessment by using only AP hip and pelvis views. Our findings suggest that inadequate anteversion sign appears when the anteversion angle is less than half the angle between X-ray beams in the AP hip and pelvis views.
- Citation: Denisov A, Bilyk S, Kovalenko A. Acetabular cup version modelling and its clinical applying on plain radiograms. World J Orthop 2017; 8(12): 929-934
- URL: https://www.wjgnet.com/2218-5836/full/v8/i12/929.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i12.929
Compared to most other orthopedic interventions, total hip arthroplasty (THA) is only a first step in a lengthy journey. Successful patient outcome relies heavily on the implant, which requires regular observation to assess the prosthesis and surrounding tissues. It is well known that bearing surface wear rate and prosthesis stability are dependent upon proper component positioning[1-3]. Thus, timely recognition of component malposition is a major goal in the postoperative period. Early awareness may allow for a timely correction of acetabular cup position and expedited return to daily activities without undesirable effects of improper component alignment. Two main parameters that must be taken into account while assessing acetabular component position are inclination and anteversion. Inclination is a measure of the angle between longitudinal axis (line drawn between the teardrops) and acetabular axis (cup tilt). Cup version measurement, on the other hand, poses a greater challenge.
Calculation of this angle can be achieved via several techniques. These methods are based on the evaluation of a visible ellipse on anteroposterior (AP) view as a result of cup rotation. Previously described techniques by Pradhan, Acland, Lewinnek are often used[4], as well as specialized software which can provide calculation of cup version[5], and even orthopedic grid calipers which approximate this calculation[6]. However, none of these techniques can differentiate cup ellipse appearance in patients with same degree of anteversion vs retroversion. This issue can be resolved by using a cross-table lateral view or computed tomography (CT) scan[7], both of which are seldom used due to challenge with patient position in the early postoperative period and concerns for radiation exposure.
To measure the sensitivity and specificity of the cup version assessment by using only AP hip and pelvis views and evaluate the incidence of inadequate cup version in patients with repeated dislocations after THA.
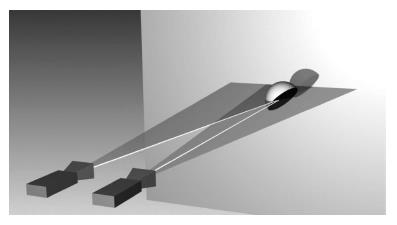
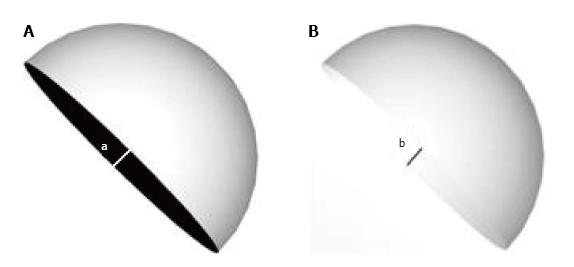
Cup shadows in retroversion and anteversion were reproduced on AP hip and pelvis views using Autodesk 3ds Max software (Autodesk, Inc., San Rafael, CA, United States) (Figure 1). Difference in angles of cup version, which may be seen as a result of difference between X-ray beams centered on AP hip and pelvis views, were subsequently analyzed. The distance from the beam source to the screen was 100 cm, the distance from the cup model to the screen was 15 cm, and the cup diameter was 50 mm. Cup version angles ranged from -20 to 20 degrees in one degree intervals. The shift of the source beam between AP pelvis and AP hip views was 12 cm. Acquired data was used for radiographic retrospective analysis of 2 groups of patients, with follow up of 6-60 mo, after undergoing primary THA.
First group of 32 patients (20 female, 12 male) with unilateral THA (32 hips) required early revision arthroplasty for reasons of dislocation. The mean age and mode were 59 years (38-83) and 66 years respectively. Average BMI was 24.2 (17.7-36.3), mode 23.9.
Second group consisted of 164 patients (101 female, 63 male) without dislocations during the follow-up period (170 hips). Among them 6 patients required bilateral THA. The average age was 60 years (38-84) and mode 59 years. BMI was 25.1 (17.2-36.8), mode 25.2. Clinical significance of cup anteversion sign was estimated with cross tabulation 2 × 2.
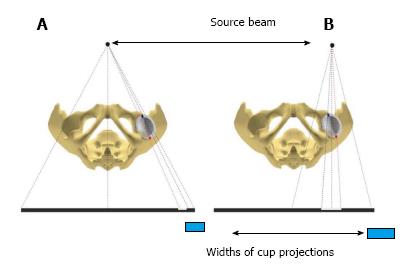
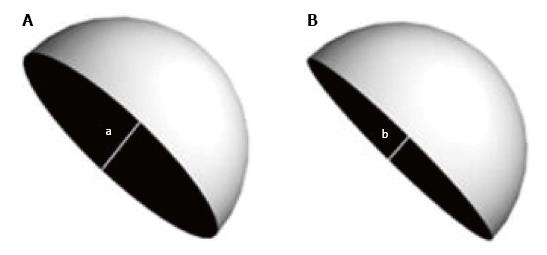
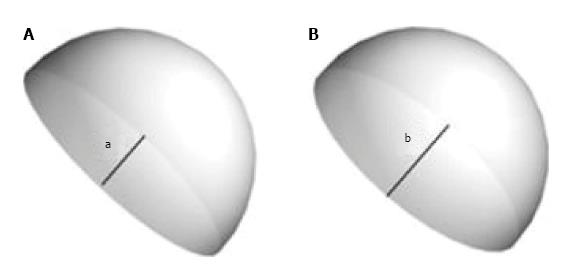
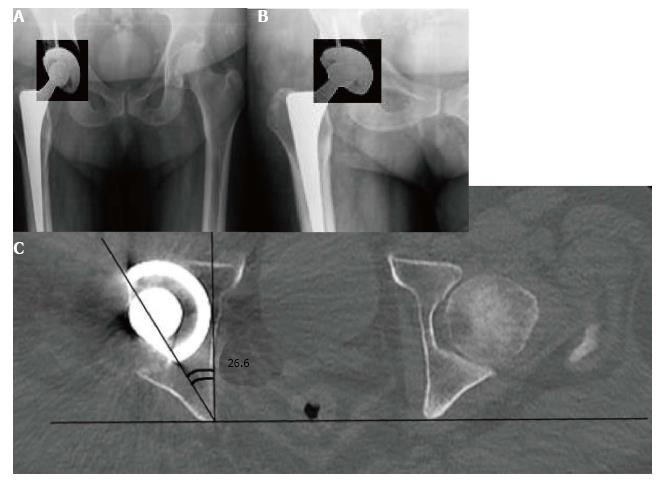
Three-dimension modelling revealed that the widths of the ellipse-shaped shadow formed by the projection of the cup base to the screen are distinct in different views (Figure 2). The shadow ellipse width appears less pronounced in AP pelvis view as compared to AP hip view when the cup is anteverted (Figure 3). On the other hand, the observed shadow profile is greater in AP pelvis view as compared to AP hip view when cup is retroverted (Figure 4). A sign of retroversion was also noted when true anteversion angle did not exceed 1/2 of the angle between X-ray beam in different views (AP hip and AP pelvis). Ellipse width profiles were equal between 2 projections at the point where true anteversion was 3.5 degrees (Figure 5).
Doubling the distance of medialization of the source beam (12 to 24 cm) from the AP hip to AP pelvis position, this threshold increased in a linear manner from 3.5 degrees to 7 degrees. Retro- or anteversion angle was confirmed with a CT scan among patients having indications for revision arthroplasty (Figure 6). For discrete X-rays assessment, we assigned expression of sign shown on Figure 2 to the sign of anteversion (SA), and all others options (Figures 3 and 4) to sign of anteversion insufficiency (SAI). Thus, two options were available in assessment of cup position on X-rays-SA and SAI. Findings are presented in Table 1.
| X-ray diagnostic conclusion | Dislocation | Total | |
| Yes | No | ||
| SAI | 9 | 12 | 21 |
| SA | 23 | 158 | 181 |
| Total | 32 | 170 | 202 |
The value of the χ2 yates was 10.668 (P < 0.01). Sensitivity of SAI was 29% (95%CI: 9%-46%), and specificity was 92% (95%CI: 88%-96%). Relative risk of dislocation in patients with SAI was 3.4 (95%CI: 1.8-6.3).
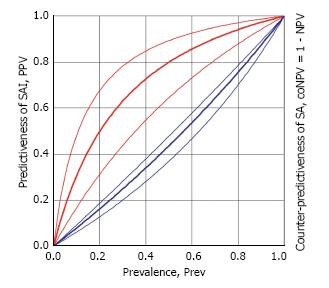
Predictiveness (positive predictive value) of SAI (predictive probability dislocation appearance) was 0.20 (95%CI: 0.09-0.38). Counter-predictiveness (Counter-negative predictive value) of SA (predictive probability dislocation absence) was only 0.046 (95%CI: 0.026-0.081) (Figure 7).
The method of this investigation was described by Markel et al[8] in 2007. However, the authors only described the technique and recommended it’s use as a screening tool without reporting its sensitivity and specificity.
Threshold value for the sign inversion corresponds to the cup anteversion value that is equal to 1/2 of the X-ray beam angle penetrating the acetabular component in AP hip and AP pelvis views. The threshold value was only 3.5° in baseline conditions of our experiment. The version sign can appear retroverted in the cases when true cup anteversion is less than the threshold values. Thus, the sign can point to retroversion while the cup is, in fact, anteverted. However, in such cases, anteversion value will be out of Lewinnek’s safety zone of 10°-20°[9] and further imaging would be encouraged. For these cases, we recommend the use of special views or a CT-scan to refine implant position.
In clinical practice threshold value, will depend on the patient anthropometric parameters which affect cup distance to the X-ray detector and the distance between centers of pelvis and hip joint. Nevertheless, two-fold shift in the beam source, compared to our model baseline condition, leads to increase in sign of inversion threshold up to 7°. This either corresponds to patient with a pelvis twice as wide than average[10] or, to a beam centered in front of a contralateral joint instead of symphysis pubis, which is unlikely. In addition, method accuracy can be affected by improper beam centering during radiography.
Low sensitivity (29%) and predictiveness (positive predictive value) of SAI (20%) can be explained by multifactorial causes of dislocation such as stem position, offset, muscle insufficiency and comorbidities. On other hand, specificity of SA (92%) points to a high probability to find SA in a patient without dislocation. Furthermore, counter-predictiveness (counter-negative predictive value) of SA points to the probability that dislocation can occur with frequency of only 4.6%. This data leads us to believe that these radiographic signs have a strong clinical relevance and can be useful in orthopedic practice.
X-ray assessment immediately after surgery or during outpatient follow-up, when lateral view is not available, can be limited to evaluation of cup inclination and ellipse presence that suggests about probable cup version. However, a bias exists because of a two-dimensional nature of conventional X-ray views. Additional comparison of cup position on AP hip and AP pelvis views allows to avoid this bias. This simple method is useful as a screening assessment of post-op cup position and, in outpatient and remote follow-up. Furthermore, it can be used for X-ray assessment in patients with early components loosening, dislocations, impingement and preoperative revision planning, especially when there is a possibility of avoiding an acetabular cup revision. In the last example provided, we recommend performing a CT-scan for additional analysis.
On the other hand, high incidence of retroversion sign confirms clinical relevance of this method in the group of patients who required early revision surgery for the reason of hip dislocations. Postoperative radiographic evaluation is usually limited to measuring of inclination and cup ellipse, may be indirect evidence of anteversion. Such assessment methodology can have an error due to plain radiography imaging features described above. Additional comparison of pelvic AP and hip AP view allows the possibility to eliminate this error during radiographic evaluation and decreases the probability of early hip joint instability. This simple radiographic test can be used both for screening assessment of acetabular cup version on postoperative images and in outpatient setting.
This method provides surgeons with ability to use it as a screening examination because of the simplicity of the acetabular component version qualitative assessment. It can be useful during patient examination with suspicion of the implant malposition, early implant loosening, dislocations and impingement to provide with the argument for obtaining CT scan. Additionally, it can provide necessary information during planning of revision surgery, especially when considering question about cup replacement, although final assessment of the cup position should be done with a CT scan.
Correct cup positioning is one of the crucial factors of preventing hip luxation after total hip arthroplasty (THA). It can be estimated using simple radiographic views (AP of pelvis and hip) and calculating of the cup inclination angle.
Some techniques can provide calculation of cup version, however none of these techniques can differentiate cup ellipse appearance in patients with same degree of anteversion vs retroversion. It can be resolved by using a cross-table lateral view or CT scan, both of which are seldom used due to challenge with patient position in the early postoperative period and concerns for radiation exposure and sometimes not available in orthopedic practice.
The authors measured the sensitivity and specificity of the cup version assessment by using AP hip and pelvis views, evaluated the incidence of inadequate version in patients with repeated dislocations after THA. The authors believe that estimation of simple radiographic anteversion sign can be used for screening assessment for further obtaining of additional examinations in case of cup malposition and repeated dislocations (as one of the provoking factor).
Cup shadows in retroversion and anteversion were reproduced on AP hip and pelvis views using Autodesk 3ds Max software (Autodesk, Inc., San Rafael, CA, United States). Difference in angles of cup version, which may be seen as a result of difference between X-ray beams centered on AP hip and pelvis views, were subsequently analyzed. Acquired data was used for analysis of 2 groups of patients, with follow up of 6-60 mo, after undergoing primary THA.
The value of the χ2 yates was 10.668 (P < 0.01). A sign of retroversion was also noted when true anteversion angle did not exceed 1/2 of the angle between X-ray beam in different views (AP hip and AP pelvis). Sensitivity of SAI was 29% (95%CI: 9%-46%), and specificity was 92% (95%CI: 88%-96%). Relative risk of dislocation in patients with SAI was 3.4 (95%CI: 1.8-6.3).
Results of our study showed high specificity of the sign of anteversion inclination 92% and low sensitivity (29%) due to other risk factors of hip dislocation.
In this article were not studied other factors provoking hip dislocation. That is way for future perspectives, the authors want to determine the current role of the cup malposition in comparison with other factors of hip luxation.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Russia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P- Reviewer: Angoules A, Cartmell S, Chen YK, Georgiev GPP, Liu JY S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Korduba LA, Essner A, Pivec R, Lancin P, Mont MA, Wang A, Delanois RE. Effect of acetabular cup abduction angle on wear of ultrahigh-molecular-weight polyethylene in hip simulator testing. Am J Orthop (Belle Mead NJ). 2014;43:466-471. [PubMed] [Cited in This Article: ] |
| 2. | Williams D, Royle M, Norton M. Metal-on-metal hip resurfacing: the effect of cup position and component size on range of motion to impingement. J Arthroplasty. 2009;24:144-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Barrack RL. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003;11:89-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 211] [Cited by in F6Publishing: 202] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 4. | Nho JH, Lee YK, Kim HJ, Ha YC, Suh YS, Koo KH. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012;94:32-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Tiberi JV, Pulos N, Kertzner M, Schmalzried TP. A more reliable method to assess acetabular component position. Clin Orthop Relat Res. 2012;470:471-476. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Liaw CK, Yang RS, Hou SM, Wu TY, Fuh CS. Measurement of the acetabular cup anteversion on simulated radiographs. J Arthroplasty. 2009;24:468-474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Esposito CI, Gladnick BP, Lee YY, Lyman S, Wright TM, Mayman DJ, Padgett DE. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015;30:109-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 154] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 8. | Markel DC, Andary JL, Pagano P, Nasser S. Assessment of acetabular version by plain radiograph. Am J Orthop (Belle Mead NJ). 2007;36:39-41. [PubMed] [Cited in This Article: ] |
| 9. | Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1972] [Cited by in F6Publishing: 1881] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 10. | Bouffard V, Begon M, Champagne A, Farhadnia P, Vendittoli PA, Lavigne M, Prince F. Hip joint center localisation: A biomechanical application to hip arthroplasty population. World J Orthop. 2012;3:131-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |