Peer-review started: August 11, 2016
First decision: September 28, 2016
Revised: October 28, 2016
Accepted: December 7, 2016
Article in press: December 9, 2016
Published online: January 18, 2017
To investigate the total blood loss (TBL) and the safety with respect to the re-amputation rate after transtibial amputation (TTA) conducted with and without a tourniquet.
The study was a single-centre retrospective cohort study of patients with a primary TTA admitted between January 2013 and April 2015. All patients with a primary TTA were assessed for inclusion if the amputation was performed because of arteriosclerosis or diabetic complications. All patients underwent a standardized TTA procedure that was performed approximately 10 cm below the knee joint and performed with sagittal flaps. The pneumatic tourniquet, when used, was inflated around the femur to a pressure of 100 mmHg above the systolic blood pressure. The number of blood transfusions within the first four postoperative days was recorded. The intraoperative blood loss (OBL), which is defined as the volume of blood lost during surgery, was determined from the suction volume and by the weight difference of the surgical dressings. The trigger for a blood transfusion was set at a decrease in the Hgb level < 9.67 g/dL (6 mmol/L). Transfusions were performed with pooled red blood cells containing 245 mL per portion, which equals 55 g/L of haemoglobin. The TBL during the first four postoperative days was calculated based on the haemoglobin level and the estimated blood volume. The re-amputation rate was evaluated within 30 d.
Seventy-four out of 86 consecutive patients who underwent TTA within the two-year study period were included in the analysis. Of these, 38 were operated on using a tourniquet and 36 were operated on without using a tourniquet. There were no significant preoperative differences between the groups. The patients in both groups had a postoperative decrease in their Hgb level compared with preoperative baseline values. The patients operated on using a tourniquet received approximately three millilitres less blood transfusion per kilogram body weight compared with patients operated on without a tourniquet. The duration of surgery was shorter and the OBL was less for the tourniquet group than the non-tourniquet group, whereas no significant difference was observed for the TBL. The TBL median was 859 mL (IQR: 383-1315) in the non-tourniquet group vs 737 mL (IQR: 331-1218) in the tourniquet group (P = 0.754). Within the 30-d follow-up period, 9 patients in the tourniquet group and 11 in the non-tourniquet group underwent a re-amputation at the trans-femoral level. The use of a tourniquet showed no statistically significant association with the 30-d re-amputation at the femur level in the multiple logistic regression model (P = 0.78). The only variable with a significant association with re-amputation was age (OR = 1.07; P = 0.02).
The results indicate that tourniquets do not cause severe vascular damage with an increased postoperative bleeding or failure rate as the result.
Core tip: The authors performed a retrospective cohort study on the use of tourniquets during transtibial amputation with the primary aim of comparing various estimates of blood loss and re-operation between the groups with or without a tourniquet. The basis for investigating this subject is the theoretical risk of increased bleeding due to vascular damage in the tourniquet group, which may, in turn, lead to increased risk of re-amputation due to local oedema, among other factors. We found no significant difference in the total blood loss when calculated on day four after surgery or in the 30-d re-amputation rate between the tourniquet and the non-tourniquet group.
- Citation: Wied C, Tengberg PT, Holm G, Kallemose T, Foss NB, Troelsen A, Kristensen MT. Tourniquets do not increase the total blood loss or re-amputation risk in transtibial amputations. World J Orthop 2017; 8(1): 62-67
- URL: https://www.wjgnet.com/2218-5836/full/v8/i1/62.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i1.62
Recent studies have illuminated the challenges in lower extremity amputation surgery where a high short-term amputation failure rate is especially notable[1,2]. No clear explanation for this result has yet been established. With this retrospective cohort study, we aimed to investigate if the possible cause is related to the use of a pneumatic tourniquet during amputation. Studies have shown that the use of a tourniquet reduces the intra-operative blood loss (OBL) and facilitates the procedure (decreases the duration of surgery) during transtibial amputations (TTA)[3]. However, despite this advantage, the use of tourniquets remains a controversial topic in amputation surgery due to potential complications[4,5]. There is a theoretical risk that the tourniquet could aggravate the blood loss during the first postoperative days. When the tourniquet pressure is applied to arteriosclerotic vessels, there is a risk of causing minor lesions and, as a result, seepage of blood. This seepage could be unrecognized by the operating surgeons due to the late onset re-perfusion of the limb after the release of the tourniquet[6] and cause severe postoperative bleeding. Such “hidden blood loss” could potentially lead to oedema of the stump and maybe associated with an increased risk of early re-amputation.
The aims of this study were (1) to compare the total blood loss (TBL) evaluated on the fourth postoperative day in patients operated with or without the use of a tourniquet and (2) to evaluate if the use of tourniquet increases the risk of re-amputation within the first 30 d after TTA performed with sagittal flaps (ad modum Persson).
The study was a single-centre retrospective cohort study of patients with a primary TTA admitted between January 2013 and April 2015. All patients with primary TTA were assessed for inclusion if amputated because of arteriosclerosis or diabetic complications. Exclusion criteria were a bilateral amputation procedure, on-going gastrointestinal bleeding, amputation due to trauma or incomplete data or death before the final measurement of haemoglobin (Hgb).
All patients underwent a standardized TTA procedure[7] performed approximately 10 cm below the knee joint and performed with sagittal flaps. The pneumatic tourniquet, when used, was inflated around the femur to a pressure of 100 mmHg greater than the systolic blood pressure[8]. It was released again at the end of the procedure but before final closure to secure haemostasis. The decision to use a tourniquet relied on the surgeons. Standardized care was provided for all patients regarding bandages, pain management, rehabilitation, fluid replacement, pausation of antiplatelet drugs, treatment with blood transfusions and thromboprophylaxis[9]. Tranexamic acid was not administered.
The number of blood transfusions within the first four postoperative days was recorded where day 0 is the day of surgery (after the start of the surgical procedure). The OBL, which is defined as the volume of blood lost during surgery, was determined from the suction volume and by the weight difference of the surgical dressings. The trigger for a blood transfusion was set at a decrease in the Hgb level < 9.67 g/dL (6 mmol/L). Transfusions were performed with pooled red blood cells containing 245 mL/portion, which equals 55 g/L of haemoglobin. The TBL during the first four postoperative days was calculated based on the haemoglobin level and the estimated blood volume. The blood volume and loss was determined according to gender, weight, height and the Hgb of the patient using formulae described in previous studies[10,11]:
Blood volume (l) = height (m)3× 0.356 + weight (kg) × 0.033 + 0.183 for women, and Blood volume (l) = height (m)3× 0.367 + weight (kg) × 0.032 + 0.604 for men. Hgbloss = blood volume × (Hgbadm - Hgbfin ) + Hgbtrans, where Hgb loss is the calculated total haemoglobin loss (g), Hgbadm is the haemoglobin value on admission, Hgbfin is the final recorded haemoglobin value on day four and Hgbtrans is the total amount of haemoglobin (in grams) in the transfused red blood cells before the measurement of Hgbfin. The calculated blood loss was estimated using the following formula:
Blood loss in millilitre = (Hgbloss/Hgbadm) × 1000.
Eight predictor variables (age, gender, body mass index, ASA score, duration of surgery, the rank of surgeon, intraoperative blood loss, and anti-fibrinolytic medication) were included in the TBL analysis due to their previously established influence on patient outcome[10,12]. Re-amputations were included if performed within 30 d following the index amputation. Six patients died within the 30-d follow-up period, and of these six patients, all underwent re-amputation; these patients were still included in the re-amputation model.
Continuous data are presented as median values with interquartile ranges (IQRs) or mean values with standard deviations. Differences between the groups were tested using a t test or a Mann-Whitney U test based on the normal distribution assumption. Categorical data are presented as numbers and were compared using the χ2 test or Fisher’s exact test in cases with cell counts of five or less. The associations of TBL and OBL with tourniquets were analysed using univariable and multivariable linear regression. The models use either TBL or OBL as the dependent variable and all previously mentioned predictor variables along with tourniquets as independent variables. The residuals in the models were tested and found to be normally distributed. A logistic regression model with tourniquet as the dependent variable was performed to identify potential inherent selection bias. The association between the 30-d re-amputation and the use of tourniquet was analysed using a multiple logistic regression model. The fit of the model was evaluated using a Hosmer-Lemeshow goodness of fit test. A P value of 0.05 was considered statistically significant. All analyses were performed by a biostatistician working in R 3.2.0 (R Foundation for Statistical Computing, Vienna, Austria).
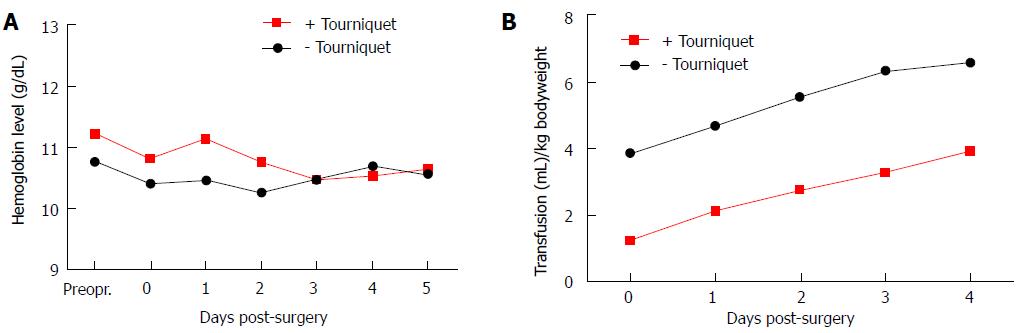
A total of 74 out of 86 consecutive patients who underwent TTA within the two-year study period were included in the analysis. Of these, 38 were operated on using tourniquets and 36 without. Six patients died before the 30-d follow-up (n = 3 in the tourniquet group and n = 3 in the non-tourniquet group). Trained residents or senior consultants performed the surgical procedures. Reasons for exclusion were bilateral amputation (n = 8), trauma (n = 2), and death before the fourth postoperative day (n = 2). There were no significant preoperative differences between the groups (Table 1). The patients in both groups had a postoperative decrease in their Hgb level compared with the preoperative baseline values, as illustrated in Figure 1A. The patients operated on using tourniquets received approximately three millilitres less transfusion blood per kilogram body weight than the patients operated on without using a tourniquet (Figure 1B, P≤ 0.03 for all days). The duration of surgery was shorter, and the OBL was less for the tourniquet group compared with the non-tourniquet group, whereas no significant difference was observed for the TBL. When the median OBL was subtracted from the median TBL for all the patients in the two groups, no significant difference was found (Table 2, P = 0.241). Within the 30-d follow-up, 9 patients in the tourniquet group and 11 in the non-tourniquet group had a re-amputation at the trans-femoral level.
| Variables | All patients n = 74 | Tourniquet group n = 38 | Non-tourniquet n = 36 | P value |
| Sex (female/male) | 25/49 | 11/27 | 14/22 | 0.511 |
| Age (yr) | 72.3 ± 11.0 | 71.3 ± 9.8 | 73.4 ± 12.1 | 0.415 |
| Height (cm) | 172 ± 9 | 173 ± 9 | 171 ± 9 | 0.178 |
| Weight (kg) | 74.2 ± 18.8 | 78.2 ± 18.6 | 70.1 ± 18.4 | 0.065 |
| Body mass index | 25.0 ± 5.4 | 25.9 ± 5.5 | 23.9 ± 5.2 | 0.112 |
| Cause of amputation (diabetes/arteriosclerosis) | 39/35 | 19/19 | 20/16 | 0.806 |
| ASA group 1-2/3-4 | 13/60 | 5/32 | 8/28 | 0.374 |
| Rank of surgeon, (resident/consultant) | 49/25 | 24/14 | 25/11 | 0.745 |
| Preoperative hemoglobin (g/dL) | 10.9 ± 1.6 | 11.2 ± 1.6 | 10.8 ± 1.4 | 0.246 |
| Preoperative Thrombocyte (× 109/L) | 368 ± 150 | 352 ± 121 | 380 ± 169 | 0.481 |
| NSAID or acetylsalicylic acid (yes/no) | 40/34 | 20/18 | 20/16 | 0.985 |
| Clopidogrel (yes/no) | 14/60 | 8/30 | 6/30 | 0.854 |
| All patients | n = 711 | Tourniquet n = 35 | Non-tourniquet n = 36 | P value |
| Duration of surgery (min) | 82 (66-106) | 78 (60-97) | 88 (72-112) | 0.041 |
| Duration of Tourniquet (min) | 30 (18-42) | |||
| Intraoperative blood loss (mL) | 250 (150-500) | 200 (100-300) | 300 (225-600) | < 0.001 |
| Total blood loss from day 0-4 (mL) | 773 (336-1218) | 737 (331-1218) | 859 (383-1315) | 0.754 |
| Delta TBL-OBL (mL) | 479 (66-855) | 495 (115-900) | 296 (-30-803) | 0.241 |
The logistic regression analysis with tourniquet as the dependent variable identified no potential selection bias. However, there was a tendency that patients with a greater body mass index more often had a tourniquet installed during surgery (P = 0.059). The univariable linear regression analysis revealed no significant effect on the TBL from any of the selected variables. Still, the average TBL was lower for women and when consultants performed the procedures (Table 3). The multiple linear regression model of factors influencing the OBL showed that the non-tourniquet group, on average, experienced a greater OBL (mean of 243 mL, P = 0.004) compared with the tourniquet group. No other variables showed a significant association with OBL. There was no significant difference between the two groups regarding the TBL (Table 3). The use of a tourniquet showed no statistically significant association with a 30-d re-amputation at the femur level in the multiple logistic regression model (P = 0.78). The only variable with a significant association with re-amputation was age (OR = 1.07; P = 0.02). The Hosmer-Lemeshow goodness of fit test had a P-value of 0.06 in the re-amputation model.
| Univariable estimate (95%CI) | P value | Multivariable estimate (95%CI) | P value | |
| Tourniquet (used) | -39 (-370-293) | 0.810 | -78 (-431-275) | 0.659 |
| Age (per year older) | -10 (-25-5) | 0.210 | -7 (-23-9) | 0.384 |
| Women/men (men) | 320 (-22-662) | 0.066 | 221 (-149-590) | 0.237 |
| Specialist registrar/consultant (consultant) | -335 (-676-6) | 0.054 | -324 (-689-41) | 0.081 |
| Clopidogrel (in treatment) | 33 (-390-456) | 0.876 | -86 (-520-349) | 0.696 |
| NSAID/acetylsalicylic acid (in treatment) | 205 (-124-534) | 0.218 | 223 (-126-572) | 0.206 |
| Duration of surgery (per minute) | 1 (-5-7) | 0.752 | -3 (-10-5) | 0.482 |
| ASA-1-2/ASA 3-4 (ASA 3-4) | -1 (424-422) | 0.995 | -66 (-506-373) | 0.764 |
| Body mass index (per one unit) | 21 (-9-52) | 0.162 | 17 (-17-50) | 0.322 |
We found that the use of a pneumatic tourniquet in dysvascular TTA surgery ad modum Persson does reduce the duration of surgery, the blood transfusion rate (millilitres of blood transfusion per kilogram bodyweight) and the OBL, but there was no significant difference in the TBL when evaluated on the fourth postoperative day. We found no evidence that the tourniquet causes severe damage to vessels and, therefore, an increased postoperative blood loss. However, although not significant, we did find that patients who were operated by a consultant experienced a lower blood loss than those operated by surgeons with less experience. We found no difference between the groups regarding re-amputation at the femur level within 30-d follow-up. This finding is similar to studies on (ad modum Burgess) amputations with long posterior flaps and tourniquets[13,14].
Patients who require a TTA due to diabetes-related complications or severe arteriosclerosis are often old and have several co-morbidities[15]. Recent studies suggest that a more restrictive strategy towards blood transfusions in patients undergoing major amputations would be appropriate since blood transfusions appear to be associated with post-operative complications, such as acute renal failure and pneumonia[16,17]. The use of a pneumatic tourniquet around the femur can reduce the OBL and, therefore, the transfusion rate and risk of transfusion-related complications[13]. However, the effect of the tourniquet in TTA surgery is not thoroughly described, and the focus has primarily been towards the ability to reduce the OBL.
Our findings of a reduction in the OBL using a tourniquet are similar to the findings from a 2006 randomized controlled trial[13]. These findings are of no surprise since the major vessels are strangulated by the tourniquet and under-tied with sutures by the surgeons. It is reasonable to assume that the reduction in the OBL will reduce the transfusion rate[14]. Our concern was that the tourniquet could aggravate the seepage of blood from the wounds due to damage to the vessels during the time when the tourniquet is inflated. However, we found no statistically significant difference between the groups when the TBL was calculated on the fourth postoperative day indicating no radical change in blood loss.
The fact that the non-tourniquet group had a greater OBL and received more blood transfusions but had a similar TBL as the tourniquet group is a dilemma. This result could illustrate a late onset drop in Hgb level in the patients operated on using tourniquets, pointing at increased postoperative bleeding. Thus, it has been shown that an exsanguinated human limb will swell by approximately 10% of its original volume after the release of a pneumatic tourniquet and mainly due to the return of the exsanguinated blood volume[6]. This delayed reperfusion, which is associated with the duration of use of the tourniquet, creates a potential source of continuous minor bleeding if the surgeons overlook minor vessels not recognized during the time when the tourniquet is inflated[18]. Even if the surgical field is inspected for minutes after the release of the tourniquet, the possible delayed re-perfusion might still cause the non-under tied vessels to begin leaking when the patients are moved from the operating room. However, if serious seepage due to damaged vessels was the case, we would have expected a more dramatic drop in Hgb and a steeper development in the transfusion curve.
This study has some limitations. Although the formula used to calculate the TBL has been used widely in other orthopaedic sub-specialties[10,19], it has limitations in amputation surgery due to the changes in the body surface area after amputation. The patients will, because of this, have a different blood volume after surgery, which is difficult to correct in the equations. However, since we compared two groups with similar baseline values and our interests are the change in the values between the groups, we believe that the calculations are acceptable to illuminate the objectives of our study. Potential biases include the operating surgeons and the selection of patients for surgery with a tourniquet. However, the logistic regression model with respect to this matter showed no evidence that a specific patient’s characteristics triggers the surgeons to use a tourniquet.
In conclusion, the use of a tourniquet reduces the duration of surgery, the OBL, and the transfusion rate in dysvascular TTA amputations. We found no significant difference in the TBL when it is calculated on day four after surgery or in the 30-d re-amputation rate between the tourniquet and the non-tourniquet group. From a haemodynamics point of view, it appears to be advantageous and safe to use a tourniquet during ad modum Persson TTA amputations.
There is an increasing number of high-risk elderly and severely comorbid patients scheduled for dysvascular lower extremity amputations. Continuous optimization of current procedures is necessary. The use of a tourniquet in dysvascular amputees is considered controversial due to fear of vascular damage and potentially increased postoperative bleeding. The primary aim of this study was to compare the total blood loss after transtibial amputation conducted with and without tourniquets, and the secondary aim was to illuminate the safety aspect regarding the re-amputation rate following (ad modum Persson) transtibial amputations.
The authors have reported the first series in the literature of patients with lower extremity amputations who were evaluated with the use of calculated total blood loss on day four after amputation. The approach provides valuable information regarding the blood loss when a tourniquet is applied during transtibial amputations.
The authors found that the use of a pneumatic tourniquet in dysvascular transtibial amputation surgery (ad modum Persson) does reduce the duration of surgery, the blood transfusion rate (millilitres of blood transfusion per kilogram bodyweight) and the intraoperative blood loss but without a significant difference in the total blood loss when evaluated on the fourth postoperative day. The authors found no evidence that the tourniquet causes severe damage to vessels and, therefore, an increased postoperative blood loss. The authors found no difference between the groups regarding re-amputation at the femur level within the 30-d follow-up. This finding is similar to studies on ad modum Burgess amputations with long posterior flaps and tourniquets.
The tourniquet can be considered during transtibial amputations to secure minimal blood loss and duration of surgery.
The study is valuable in showing that the total blood loss is not increased by either method.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Denmark
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Bamberg SJM, Tuncer S S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Wied C, Kristensen MT, Tengberg PT, Holm G, Krasheninnikoff M, Troelsen A. [Patients in need for major lower extremity amputations are a challenge]. Ugeskr Laeger. 2015;177:pii: V10140540. [PubMed] [Cited in This Article: ] |
| 2. | Kristensen MT, Holm G, Gebuhr P. Difficult to predict early failure after major lower-extremity amputations. Dan Med J. 2015;62:A5172. [PubMed] [Cited in This Article: ] |
| 3. | Wakai A, Winter DC, Street JT, Redmond PH. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001;9:345-351. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 115] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001;9:253-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Klenerman L. The tourniquet in operations on the knee: a review. J R Soc Med. 1982;75:31-32. [PubMed] [Cited in This Article: ] |
| 6. | Silver R, de la Garza J, Rang M, Koreska J. Limb swelling after release of a tourniquet. Clin Orthop Relat Res. 1986;86-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 35] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Persson BM. Sagittal incision for below-knee amputation in ischaemic gangrene. J Bone Joint Surg Br. 1974;56:110-114. [PubMed] [Cited in This Article: ] |
| 8. | Ishii Y, Matsuda Y. Effect of tourniquet pressure on perioperative blood loss associated with cementless total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2005;20:325-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Kristensen MT, Holm G, Krasheninnikoff M, Jensen PS, Gebuhr P. An enhanced treatment program with markedly reduced mortality after a transtibial or higher non traumatic lower extremity amputation. Acta Orthop. 2016;87:1-6. [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br. 2006;88:1053-1059. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 228] [Cited by in F6Publishing: 253] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 11. | Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224-232. [PubMed] [Cited in This Article: ] |
| 12. | Taylor SM, Kalbaugh CA, Blackhurst DW, Hamontree SE, Cull DL, Messich HS, Robertson RT, Langan EM, York JW, Carsten CG. Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg. 2005;42:227-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 13. | Choksy SA, Lee Chong P, Smith C, Ireland M, Beard J. A randomised controlled trial of the use of a tourniquet to reduce blood loss during transtibial amputation for peripheral arterial disease. Eur J Vasc Endovasc Surg. 2006;31:646-650. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Singh R, Ghani A, Hakak A, Singh S, Singh B, Padha K, Muzafar K. Use of pneumatic tourniquet in transtibial amputation for peripheral vascular disease: A prospective randomized blinded controlled trail. Int J Curr Res. 2015;7:20086-20089. [Cited in This Article: ] |
| 15. | Belmont PJ, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213:370-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 16. | D’Ayala M, Huzar T, Briggs W, Fahoum B, Wong S, Wise L, Tortolani A. Blood transfusion and its effect on the clinical outcomes of patients undergoing major lower extremity amputation. Ann Vasc Surg. 2010;24:468-473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Ponnusamy KE, Kim TJ, Khanuja HS. Perioperative blood transfusions in orthopaedic surgery. J Bone Joint Surg Am. 2014;96:1836-1844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 18. | Klenerman L, Crawley J, Lowe A. Hyperaemia and swelling of a limb upon release of a tourniquet. Acta Orthop Scand. 1982;53:209-213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86:561-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 312] [Cited by in F6Publishing: 319] [Article Influence: 16.0] [Reference Citation Analysis (0)] |