Published online Sep 18, 2016. doi: 10.5312/wjo.v7.i9.623
Peer-review started: April 29, 2016
First decision: June 17, 2016
Revised: July 1, 2016
Accepted: July 14, 2016
Article in press: July 18, 2016
Published online: September 18, 2016
A case of complicated lateral subtalar dislocation is presented and the literature concerning this injury is reviewed. Subtalar joint dislocations are rare and often the result of a high-energy trauma. Complications include avascular necrosis of the talus, infection, posttraumatic osteoarthritis requiring arthrodesis and chronic subtalar instability. Negative prognostic factors include lateral and complicated dislocations, total talar extrusions, and associated fractures. A literature search was performed to identify studies describing outcome after lateral subtalar joint dislocation. Eight studies including fifty patients could be included, thirty out of 50 patients suffered a complicated injury. Mean follow-up was fifty-five months. Ankle function was reported as good in all patients with closed lateral subtalar dislocation. Thirteen out of thirty patients with complicated lateral subtalar joint dislocation developed a complication. Avascular necrosis was present in nine patients with complicated injury. Four patients with complicated lateral subtalar dislocation suffered deep infection requiring treatment with antibiotics. In case of uncomplicated lateral subtalar joint dislocation, excellent functional outcome after closed reduction and immobilization can be expected. In case of complicated lateral subtalar joint dislocation immediate reduction, wound debridement and if necessary (external) stabilisation are critical. Up to fifty percent of patients suffering complicated injury are at risk of developing complications such as avascular talar necrosis and infection.
Core tip: Subtalar dislocations are a rare and severe injury which is often result of high-energy trauma. Subtalar dislocations represent 1%-2% of all dislocations. The foot is displaced laterally in about 25% of cases. Excellent outcome can be expected in patients with uncomplicated lateral subtalar dislocation if immediate closed reduction is achieved. In case of complicated subtalar joint dislocations requiring open reduction, wound debridement, appropriate joint reduction and additional stabilisation with an external fixation are critical. A complication rate up to 50% can be expected in these patients.
- Citation: Veltman ES, Steller EJ, Wittich P, Keizer J. Lateral subtalar dislocation: Case report and review of the literature. World J Orthop 2016; 7(9): 623-627
- URL: https://www.wjgnet.com/2218-5836/full/v7/i9/623.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i9.623
Subtalar joint dislocation is defined as a simultaneous dislocation of the subtalar (talocalcaneal) and talonavicular joint[1]. Subtalar dislocations are rare and often the result of high-energy trauma[1,2]. Rarity of this injury can be attributed to the presence of strong ligaments connecting the talus and the calcaneus, the strong biomechanical properties of the ankle and the tight joint capsule[2]. The trauma causing this type of injury is frequently a fall from considerable height or a motor vehicle accident[4]. In American literature, a large number of patients feature trauma after jumps during a basketball game, which has led to the term “basketball foot”[3,4].
Subtalar joint dislocations are frequently accompanied by fractures of the adjacent tarsal and metatarsal bones. Severe soft tissue injury can also be present[1]. The currently used classification of subtalar dislocations was introduced by Broca in 1853 and adjusted by Malgaigne et al[5] in 1856. Dislocations of the talus are classified based on the direction in which the foot is dislocated[1,6]. In about 72% of patient the talus is dislocated medially, lateral dislocation is present in 26% of patients and posterior or anterior dislocation in the remainder of patients[1]. Lateral subtalar joint dislocations are produced by forced eversion with the foot in dorsiflexion[1]. Inability to reduce lateral subtalar dislocations can be caused by interposition of the posterior tibialis tendon in case of rupture of the flexor retinaculum[7,8]. Pure ligamentous dislocations have an excellent prognosis after proper reduction[9]. Diagnosing additional injury is essential, as fractures of the lateral talar process and the sustentaculum tali may lead to the rapid development of posttraumatic osteoarthritis of the subtalar joint[10]. Talar avascular necrosis is reported in up to 50% of patients after complicated lateral subtalar dislocation[11].
Isolated lateral subtalar joint dislocation has only scarcely been described in literature. We report the case of a patient suffering complicated lateral subtalar joint dislocation and we give a comprehensive review of the available literature on lateral subtalar joint dislocations.
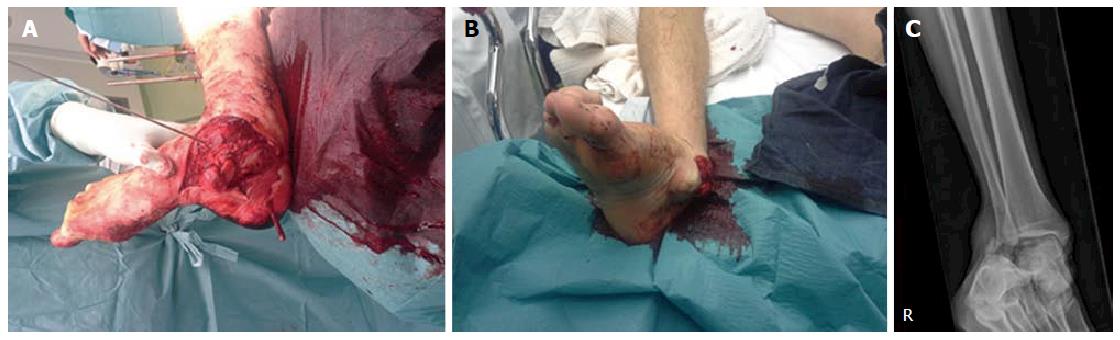
In May 2015, a 31-year-old male was presented to the emergency room with pain of the foot after eversion trauma while jumping on a trampoline. Initial trauma screening revealed a hemodynamically stable patient with a complicated (Gustilo type 3) subtalar joint dislocation of the right leg (Figure 1). During trauma screening no other injuries were detected. The patient was transported to the OR within 4 h of presentation. The dislocated talus was immediately reduced using a surgical spoon and a femoral head impactor. We performed meticulous wound debridement, after which the wound was closed transcutaneously over a subcutaneous low vacuum drain. A joint bridging external fixator was constructed with additional kirschner-wires for reduction and temporary stabilisation (Figure 2). A postoperative computed tomography (CT) scan showed several small fracture fragments of the talar bone with congruent ankle and subtalar joints. There were no fractures of the adjacent tarsal and metatarsal bones.
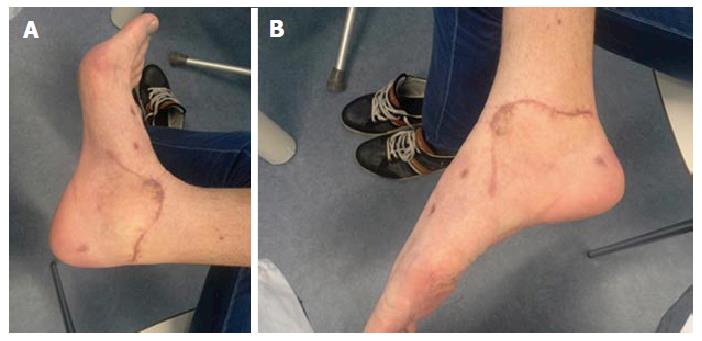
The medial wound healed uneventfully. Eight weeks postoperatively the external fixator and kirschner wires were removed during a visit at the outpatient clinic. At this time the patient engaged in physical therapy and commenced bearing full weight on the affected leg. One year after injury the patient is walking without pain, only using a cane for long distances. Range of motion of the ankle is not restricted (Figure 3). Conventional radiographs show early signs of talar avascular necrosis (Figure 4), without associated clinical symptoms.
Methods: The search was limited to humans aged over eighteen years with a subtalar dislocation. PubMed/MEDLINE, EMBASE, and the Cochrane Library were searched from up to April 1st 2016. Exclusion criteria were minor age and subtalar dislocation in medial, anterior or posterior direction. Case reports were excluded to limit report bias. The lists of references of retrieved publications were manually checked for additional studies potentially meeting the inclusion criteria and not found by the electronic search. Studies reporting various types of subtalar dislocation were identified and only included if the results of patients with lateral subtalar dislocation could be extracted separately.
We collected all information regarding the level of evidence, baseline patient characteristics, baseline clinical findings and mean period of follow-up. Data regarding type and timing of surgery, postoperative regimen, complications, functional outcome, radiological outcome and patient satisfaction were extracted.
Results: The literature search displayed 367 studies, of which eight studies including fifty patients could be included[6,11-17]. General characteristics can be found in Table 1. All reported numbers are sample-size weighted. Eighty-seven percent of patients were male. Mean age was thirty-four years. Subtalar dislocations were evenly distributed over de left and right extremity. Thirty out of 50 patients suffered a complicated injury. Unfortunately Gustilo grading of complicated injury was not reported in all studies and therefore not available for analysis in this study. Associated fractures of the tarsal or metatarsal bones were present in seventeen patients, posterior tibial tendon rupture was present in six patients.
| Ref. | Year | No.of patients | Follow-up (mo) | Age | Male | Female | Left | Right | Complicated injury | Avascular necrosis | Infection |
| Camarda et al[12] | 2015 | 3 | 69 | 50 | x | x | x | x | 0 | 0 | 0 |
| Edmunds et al[13] | 1991 | 4 | 36 | 43 | 4 | 0 | 3 | 1 | 4 | 3 | 1 |
| Garofalo et al[14] | 2004 | 5 | 122 | 32 | 4 | 1 | 3 | 2 | 4 | 0 | 0 |
| Goldner et al[11] | 1995 | 10 | 36 | 26 | 8 | 2 | x | x | 10 | 5 | 2 |
| Jungbluth et al[6] | 2010 | 6 | 58 | 42 | 4 | 2 | x | x | 2 | 0 | 0 |
| Karampinas et al[15] | 2009 | 9 | 21 | 32 | 7 | 2 | 4 | 5 | 9 | 1 | 1 |
| Merchan et al[16] | 1992 | 10 | 66 | 36 | 7 | 3 | 2 | 8 | 1 | 0 | 0 |
| Ruhlmann et al[17] | 2016 | 3 | 84 | 39 | 3 | 0 | 2 | 1 | 0 | 0 | 0 |
| Total/mean | 50 | 55 | 34 | 37 | 10 | 14 | 17 | 30 | 9 | 4 |
Closed lateral subtalar dislocations were treated with reduction and below the knee casting. Closed reduction was successful in all of these cases. All complicated lateral subtalar dislocations were treated with wound debridement. Additional fixation with k-wires was performed in three patients. An external fixator was placed in eleven patients, the other nineteen patients were treated with a below the knee cast. The patients were non-weight bearing for a mean period of seven weeks (range 4-12), after which the cast was removed and patients were allowed to bear weight. Mean follow-up was fifty-five months. Four studies[6,12,15,17] provide patient reported outcome with the use of the American Orthopaedic Foot and Ankle Society score (AOFAS)[18], which has not been validated for this purpose. Mean AOFAS score at follow-up was 82. Ankle function was reported as good in all patients with closed lateral subtalar dislocation. Severe pain was reported in nine patients with avascular necrosis and in two additional patients with severe osteoarthritis.
Radiologic assessment revealed subtalar osteoarthritis (Altman et al[19] type 2 or 3) in eight out of fifty patients. Avascular necrosis was present in nine additional patients. Patients with avascular necrosis were eventually treated with arthrodesis of the ankle in most cases. Four patients with complicated lateral subtalar dislocation suffered deep infection requiring treatment with antibiotics.
Lateral subtalar joint dislocation is a rare and severe injury. The number of patients reported with this type of injury is therefore small. The high-energy trauma which is needed to cause lateral dislocation is reflected in the percentage of patients with severe soft tissue damage. Immediate reduction, extensive wound debridement and when necessary additional stabilisation are key features of treatment and should be performed as short after presentation as possible.
Complications are not evenly distributed among patients with closed and complicated injury. The literature review reports avascular necrosis or deep infection in 13 out of 30 patients with complicated lateral subtalar dislocation, compared to no avascular necrosis or deep infection in twenty patients with closed subtalar dislocation. Complicated injury is the main predictor of poor outcome. Avascular necrosis or deep infection can be expected in about 50% of cases.
In all cases, in addition to plain ankle and foot radiographs, a CT-scan should be performed after reduction to document additional bony injury to the subtalar area and adjacent bones. Additional injury is often underestimated in a plain radiograph of the hindfoot, but can have serious consequences such as osteoarthritis or chronic instability if undetected.
The duration of immobilization remains controversial. In uncomplicated injury an early weight-bearing protocol seems possible, after a lower leg cast for a period of 3-4 wk. In case of complicated injury or instability the use of an external fixator might be necessary, prohibiting patients from walking for a period of 6-12 wk depending on the extent of additional fractures of the tarsal and metatarsal bones.
This study gives a comprehensive review of the literature concerning lateral subtalar joint dislocation, treatment and expected outcome. Unfortunately, our literature search shows a lack of quality evidence. High level evidence on treatment and prognosis of subtalar joint dislocations is absent due to the rarity of this injury. The weaknesses of the original studies are reflected in our results. Patient specific characteristics such as smoking, obesity and diabetes, which affect the risk of developing avascular necrosis or infection, were not reported in the original studies and therefore not analysed. Daily practice would benefit from a large scale prospective study on optimal treatment, however with the extremely low number of patients suffering this injury this can be qualified as wishful thinking.
Excellent outcome can be expected in patients with uncomplicated lateral subtalar dislocation if immediate closed reduction is achieved. In case of complicated subtalar joint dislocations requiring open reduction, wound debridement, appropriate joint reduction and additional stabilisation with an external fixation are critical. A complication rate up to 50% can be expected in these patients. The review helps physicians treating a patient with a lateral subtalar dislocation to discuss treatment and prognosis of this severe injury of the foot.
Hindfoot pain and Gustilo grade 3 complicated injury of the hindfoot after jumping the trampoline.
Gustilo grade 3 complicated, isolated lateral subtalar joint dislocation.
Ankle luxation fracture, talar fracture, talar extrusion, talar fracture, calcaneal fracture.
All labs were within normal limits.
Plain radiographs (before reduction) of the foot showed a lateral subtalar dislocation. A post-reduction computed tomography-scan demonstrated multiple small fracture fragments of the talar bone, without fractures of the adjacent bones.
Immediate reduction, wound debridement and external fixation.
See reference list for more articles on the same subject.
Immediate reduction and meticulous wound debridement are key features in treating subtalar dislocations. In case of instability external fixation can be applied.
A simple rare article with simple to understand and something to learn.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: the Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Brasileiro B, Wani IA S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Hoexum F, Heetveld MJ. Subtalar dislocation: two cases requiring surgery and a literature review of the last 25 years. Arch Orthop Trauma Surg. 2014;134:1237-1249. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Giannoulis D, Papadopoulos DV, Lykissas MG, Koulouvaris P, Gkiatas I, Mavrodontidis A. Subtalar dislocation without associated fractures: Case report and review of literature. World J Orthop. 2015;6:374-379. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Simon LC, Schulz AP, Faschingbauer M, Morlock M, Jürgens C. [“Basketball Foot”--long-time prognosis after peritalar dislocation]. Sportverletz Sportschaden. 2008;22:31-37. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Wagner R, Blattert TR, Weckbach A. Talar dislocations. Injury. 2004;35 Suppl 2:SB36-SB45. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Malgaigne JF, Buerger CG. Die Knochenbrüche und Verrekungen. Stuttgart: Rieger, 1856. [Cited in This Article: ] |
| 6. | Jungbluth P, Wild M, Hakimi M, Gehrmann S, Djurisic M, Windolf J, Muhr G, Kälicke T. Isolated subtalar dislocation. J Bone Joint Surg Am. 2010;92:890-894. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Waldrop J, Ebraheim NA, Shapiro P, Jackson WT. Anatomical considerations of posterior tibialis tendon entrapment in irreducible lateral subtalar dislocation. Foot Ankle. 1992;13:458-461. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | de Palma L, Santucci A, Marinelli M, Borgogno E, Catalani A. Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg. 2008;128:593-598. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Rammelt S, Goronzy J. Subtalar dislocations. Foot Ankle Clin. 2015;20:253-264. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Bibbo C, Lin SS, Abidi N, Berberian W, Grossman M, Gebauer G, Behrens FF. Missed and associated injuries after subtalar dislocation: the role of CT. Foot Ankle Int. 2001;22:324-328. [PubMed] [Cited in This Article: ] |
| 11. | Goldner JL, Poletti SC, Gates HS, Richardson WJ. Severe open subtalar dislocations. Long-term results. J Bone Joint Surg Am. 1995;77:1075-1079. [PubMed] [Cited in This Article: ] |
| 12. | Camarda L, Abruzzese A, La Gattuta A, Lentini R, D’Arienzo M. Results of closed subtalar dislocations. Musculoskelet Surg. 2016;100:63-69. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Edmunds I, Elliott D, Nade S. Open subtalar dislocation. Aust N Z J Surg. 1991;61:681-686. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Garofalo R, Moretti B, Ortolano V, Cariola P, Solarino G, Wettstein M, Mouhsine E. Peritalar dislocations: a retrospective study of 18 cases. J Foot Ankle Surg. 2004;43:166-172. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Karampinas PK, Kavroudakis E, Polyzois V, Vlamis J, Pneumaticos S. Open talar dislocations without associated fractures. Foot Ankle Surg. 2014;20:100-104. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Merchan EC. Subtalar dislocations: long-term follow-up of 39 cases. Injury. 1992;23:97-100. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Ruhlmann F, Poujardieu C, Vernois J, Gayet LE. Isolated Acute Traumatic Subtalar Dislocations: Review of 13 Cases at a Mean Follow-Up of 6 Years and Literature Review. J Foot Ankle Surg. 2016;. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Altman RD, Hochberg M, Murphy WA, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3 Suppl A:3-70. [PubMed] [Cited in This Article: ] |