Published online Apr 18, 2016. doi: 10.5312/wjo.v7.i4.251
Peer-review started: June 1, 2015
First decision: August 25, 2015
Revised: December 17, 2015
Accepted: January 8, 2016
Article in press: January 11, 2016
Published online: April 18, 2016
AIM: To investigate the short-term clinical results of the Oxford phase III cementless medial unicondylar knee prosthesis (UKP) compared to the cemented medial UKP.
METHODS: We conducted a cross-sectional study in a tertairy orthopedic centre between the period of May 2010 and September 2012. We included 99 medial UKP in 97 patients and of these UKP, 53 were cemented and 46 were cementless. Clinical outcome was measured using a questionnaire, containing a visual analogue scale (VAS) for pain, Oxford Knee score, Kujala score and SF-12 score. Knee function was tested using the American Knee Society score. Complications, reoperations and revisions were recorded. Statistical significance was defined as a P value < 0.05.
RESULTS: In a mean follow-up time of 19.5 mo, three cemented medial UKP were revised to a total knee prosthesis. Reasons for revision were malrotation of the tibial component, aseptic loosening of the tibial component and progression of osteoarthritis in the lateral- and patellofemoral compartment. In five patients a successful reoperation was performed, because of impingement or (sub)luxation of the polyethylene bearing. Patients with a reoperation were significant younger than patients in the primary group (56.7 vs 64.0, P = 0.01) and were more likely to be male (85.7% vs 38.8%, P = 0.015). Overall the cementless medial UKP seems to perform better, but the differences in clinical outcome are not significant; a VAS pain score of 7.4 vs 11.7 (P = 0.22), an Oxford Knee score of 43.3 vs 41.7 (P = 0.27) and a Kujala score of 79.6 vs 78.0 (P = 0.63). The American Knee Society scores were slightly better in the cementless group with 94.5 vs 90.2 (P = 0.055) for the objective score and 91.2 vs 87.8 (P = 0.25) for the subjective score.
CONCLUSION: The cementless Oxford phase III medial UKP shows good short-term clinical results, when used in a specialist clinic by an experienced surgeon.
Core tip: The higher revision rate in unicondylar knee arthroplasty compared to total knee arthroplasty is a concern. The cementless unicondylar knee prosthesis (UKP) eliminates one of the technical errors related to failure; the cementing technique. The cementless Oxford UKP also shows reduced radiolucent lines at one year follow-up, whereas the cemented UKP shows occurrence of radiolucent lines. The developing hospital has published encouraging results of the cementless Oxford phase III medial UKP. In our independent retrospective cohort study we observed three revisions of cemented UKP. There were five successful reoperations. The cementless UKP seems to perform better, but no significant difference could be found.
- Citation: Dorp KBV, Breugem SJ, Bruijn DJ, Driessen MJ. Promising short-term clinical results of the cementless Oxford phase III medial unicondylar knee prosthesis. World J Orthop 2016; 7(4): 251-257
- URL: https://www.wjgnet.com/2218-5836/full/v7/i4/251.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i4.251
The unicondylar knee prosthesis (UKP) is an established treatment for end-stage medial osteoarthritis (OA) of the knee and accounts for around 8%-10% of all primary knee replacements[1,2]. One of the successful implants used, is the cemented Oxford medial UKP phase III. This is a fully congruent mobile bearing prosthesis, which is implanted via a minimal invasive procedure with minimal bone-loss. Success of the medial UKP is still largely related to the indication for UKP and the experience of the surgeon and the surgical team. This is confirmed by the lower survival rates of UKP in national registers compared to the survival rates of UKP implanted by specialized surgeons who perform UKP surgery regularly[1,2].
The higher revision rates in unicondylar arthroplasty are a concern. The difference in revision rate between UKP and total knee prosthesis (TKP) is likely to be multi-factorial. A major issue seems to be the ease to choose for revision of a UKP compared to a revision of a TKP. With the introduction of the cementless Oxford UKP (2003) one of the technical errors related to failure, the cementing technique, can be eliminated. Also, the cementless Oxford medial UKP shows reduced radiolucent lines at one year follow-up, whereas the cemented Oxford medial UKP shows occurrence of radiolucent lines during follow-up[3]. The occurrence of these radiolucent lines is thought to be a misleading factor for revision in patients with unexplained pain after cemented UKP. The developing hospital has published encouraging results of the cementless Oxford phase III UKP[3], as well as cementless UKP by other manufacturers[4-6].
Since May 2010 the cementless Oxford phase III medial UKP is frequently used in our clinic besides the cemented Oxford phase III medial UKP. In accordance with earlier published results, it is our experience that the cementless Oxford UKP performs as well as, or even better than the cemented Oxford UKP. With this retrospective study we want to compare the short-term clinical outcome of the cemented and the cementless Oxford phase III medial UKP performed in an independent center by one single surgeon.
We conducted a cross-sectional study in an orthopedic center, specialized in prosthesiology and sports medicine. Between May 19, 2010 and September 01, 2011 a total of 106 medial UKP were implanted in 103 patients with primary medial osteoarthritis. For inclusion, patients had to meet the Oxford selection criteria for UKP and had to have a minimum follow-up of one year. Age, activity status and former high tibial osteotomy were not considered contra-indications. Exclusion criteria were patients who had surgery on their lower extremities less than 6 mo ago, hybrid fixation, patients with insufficient comprehension of the Dutch language and patients living abroad.
Of the 103 eligible patients, two patients were deceased at the time of follow-up and one patient refused participation. Four patients did not meet the inclusion criteria and were excluded from the study. Reasons for exclusion were: living abroad (two cemented UKP), surgery on the lower extremities less than 6 mo ago and Multiple Sclerosis with progressive muscle weakness (cementless UKP). In total 99 UKP in 97 patients were included in the study. All study participants provided informed written consent prior to study enrollment. All study participants agreed with anonymous data sharing.
The medial Oxford phase III cemented and the cementless UKP are similar in design, except for the cylindrical main peg and a smaller anterior peg added posterior to the main peg in the cementless femoral component. Additionally, the cementless UKP has a hydroxyapatite coating with a porous titanium undercoating to stimulate bone adhesion.
All surgeries were performed by the senior author (MD), who performs more than 100 UKP per year. A short medial arthrotomy was used, followed by a thorough inspection of the knee to make the final decision. If the chondropathy was limited to the anteromedial tibia plateau, the lateral compartment had full thickness cartilage in the weight-bearing areas and the ligaments were intact, the knee was fit for an UKP. A tourniquet was used in all cases. The surgical technique was performed as described in the Oxford operative manual, but without intramedullary alignment of the femur component, as we believe this enlarges the risk of haemarthrosis.
Patients were told to start active knee flexion and extension as soon as possible. Post-operative pain management consisted of Acetaminophen, Diclofenac and an epidural patient controlled pain pump with Chirocaïn/Sufentanil in the first ± 24 h. Full weight-bearing with two elbow crutches was started the second post-operative day. Thrombosis prophylaxis consisted of Nadroparine and a compression stocking for a period of 6 wk. Patients who did not reach full extension or had trouble reaching 90 degrees flexion at discharge started with physical therapy immediately. All other patient started physical therapy 2 wk post-operative, to ensure adequate wound healing the first two weeks.
Except for patients who had a revision and patients who had a reoperation less than 6 mo ago, all patients received a questionnaire consisting a visual analogue scale (VAS) for pain ranging from 0-100 (0 being no pain), the Oxford Knee score (OKS) scored from 48 to 0 with 48 being the best possible outcome[7], the Kujala anterior knee pain score scored from 100 to 0 with 100 being the best possible score[8] and the SF-12 health survey[9]. If questions were left blank we contacted patients by phone. For clinical outcome we used the American Knee Society score[10] (AKSS objective and subjective score both ranging from 0-100, with 100 being the best possible score) performed by the first author (Karin B van Dorp) or by one of the co-authors. Range of motion and alignment were measured with the patient in supine position and with a goniometer measuring in 5 degree increments.
Revision was defined as a case in which the femoral or tibial component had to be removed and cases which were planned for this procedure. Cases in which nettoyage and polyethylene (PE) meniscal replacement took place or cases which were planned for this procedure are defined as reoperation.
Conventional X-rays in anteroposterior and lateral view, taken pre-operative, the first day post-operative and one year post-operative were evaluated on osteoarthritis grade per compartment using the Ahlbäck[11] (scored from 1 to 5, focusing on narrowing/attrition) by the first author. Progression of osteoarthritis of the lateral or patellofemoral compartment was defined as a change in Ahlbäck score between the X-rays taken the first day-post-operative and one year post-operative.
Data were analyzed using SPSS 17 (IBM, New York, United States). Statistical significance was defined as a P value < 0.05. Scale variables were tested using the independent samples t test. Pearson’s χ2 test was used in case of nominal or ordinal variables.
Of the 99 medial UKP implanted, 53 (53.5%) were cemented UKP and 46 (46.5%) were cementless UKP. Patient characteristics are described in Table 1. The groups were well matched, except for a shorter follow-up time in the cementless group 18.3 mo vs 20.5 mo (P = 0.02). This difference was caused by the relatively low volume of cementless UKP implanted in the introduction period.
| Cementedn = 53 | Cementlessn = 46 | P value | |
| Age (yr) | 64.6 ± 8.2 | 62.2 ± 6.7 | 0.12 |
| Sex | 0.471 | ||
| Male | 21 (39.6%) | 21 (45.7%) | |
| Female | 32 (60.4%) | 25 (54.3%) | |
| ASA | 0.497 | ||
| 1 | 15 (28.3%) | 10 (21.7%) | |
| 2 | 30 (56.6%) | 31 (67.4%) | |
| 3 | 8 (15.1%) | 5 (10.9%) | |
| BMI (kg/m2) | 27.7 ± 4.1 | 29.0 ± 4.7 | 0.17 |
| Follow-up (mo) | 20.5 ± 3.9 | 18.3 ± 4.5 | 0.02 |
| Ahlbäck grade medial joint space | 0.442 | ||
| 0 (> 3 mm) | 0 (0%) | 1 (2.2%) | |
| 1 (< 3 mm) | 41 (77.4%) | 33 (71.7%) | |
| 2 (Obliteration) | 10 (18.9%) | 12 (26.1%) | |
| 3 (Attrition < 5 mm) | 2 (3.8%) | 0 | |
| Ahlbäck grade lateral joint space | 0.129 | ||
| 0 (> 3 mm) | 53 (100%) | 45 (95.7%) | |
| 1 (< 3 mm) | 0 | 2 (4.3%) | |
| 2 (Obliteration) | 0 | 0 | |
| 3 (Attrition < 5 mm) | 0 | 0 | |
| Ahlbäck grade patellofemoral joint space | 0.139 | ||
| 0 (> 3 mm) | 29 (54.7%) | 18 (39.1%) | |
| 1 (< 3 mm) | 23 (43.4%) | 28 (60.9%) | |
| 2 (Obliteration) | 1 (1.9%) | 0 | |
| 3 (Attrition < 5 mm) | 0 | 0 | |
During a mean follow-up of 19.5 mo (range 12-33 mo, SD 4.3), seven patients were eligible for reoperation (7%) and three revisions tot TKP were performed (3%). An overview of reoperations and revisions is given in Table 2. The main reason for reoperation was bony or soft-tissue impingement in four cases (4.1%). In two cases (2.0%) subluxation of the meniscal bearing and in one case (1.0%) a 90 degrees rotation of the meniscal bearing occurred. Reoperations were treated with a minimal invasive medial arthrotomy, using the old incision. The impinging osteophytes were removed with a small osteotome, the presence of posterior osteophytes was checked with a curved osteotome and excessive fibrotic tissue was removed. In all cases a thicker PE meniscus was necessary to gain the appropriate balance. The clinical outcome of the reoperations, which were performed more than 6 mo ago, were all good to excellent (Table 2). Statistically, patients with a reoperation were significant younger than patients in the primary group (56.7 vs 64.0, P = 0.01) and were more likely to be male (85.7% vs 38.8%, P = 0.015). There were no significant differences between the primary group and the redo group concerning body mass index (BMI), ASA classification, SF-12 scores and pre-operative or post-operative OA grade.
| Type | Fixation | Operation performed | Indication | Survival(mo) | Gender | Age(yr) | ASA | BMIkg/m2 | OKS | AKSSO/S |
| Revision | C | TKP PS 5/5/15 mm | Malrotation tibial component | 16 | Male | 50 | 1 | 30.0 | - | - |
| Redo | CL | Nettoyage PE 5 to 8 | Subluxation PE | 19 | Male | 50 | 1 | 30.0 | 48 | 100/100 |
| Revision | C | TKP elsewhere | Aseptic loosening tibial component | 20 | Female | 78 | 1 | 27.2 | - | - |
| Redo | C | Nettoyage PE 5 to 6 | PE luxation 90 degrees | 21 | Male | 60 | 2 | 32.8 | 46 | 100/100 |
| Redo | CL | Nettoyage PE 5 to 7 | Impingement | 21 | Male | 55 | 3 | 32.4 | 37 | 80/90 |
| Redo | CL | Nettoyage PE 4 to 7 | Impingement | 21 | Male | 64 | 2 | 31.7 | 42 | 90/100 |
| Redo | C | Nettoyage PE 4 to 6 | Subluxation PE | 22 | Male | 51 | 2 | 28.4 | 48 | 95/100 |
| Redo | CL | Planned | Impingement | 23 | Male | 55 | 2 | 26.6 | - | - |
| Redo | CL | Planned | Impingement | 26 | Female | 62 | 2 | 25.8 | - | - |
| Revision | C | ACS 5/5/12, 5 mm | Progression of OA lateral/PF | 27 | Male | 51 | 2 | 36.3 | - | - |
All three revisions (3.1%) to TKP were cemented Oxford UKP. Reasons for revision were malrotation of the tibial component, aseptic loosening of the tibial component (revision surgery was performed elsewhere) and progression of OA in the lateral- and patellofemoral compartment. The time to revision was 16, 20 and 27 wk post-implantation. There were no significant differences between the primary group and the revision group concerning age, gender, BMI, ASA classification, SF-12 scores and pre-operative or post-operative Ahlbäck score.
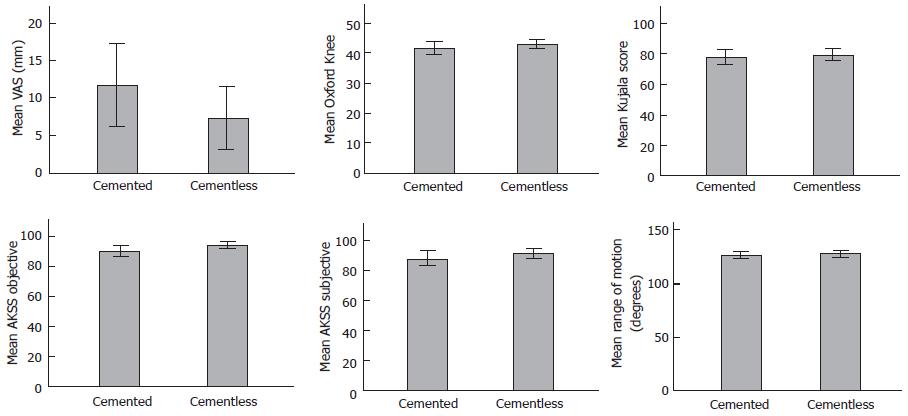
The revisions and reoperations excluded, 89 of the original UKP were still in situ and eligible for clinical assessment. Although no significant differences were found, the scores were slightly better in the cementless group, with a VAS pain score of 7.4 vs 11.7 (P = 0.22), an OKS of 43.3 vs 41.7 (P = 0.27) and a Kujala score of 79.6 vs 78.0 (P = 0.63) (Figure 1).
Because of health issues three patients accounting for four medial UKP were not able to come to our clinic for clinical evaluation. One patient refused clinical evaluation because of personal reasons. All these patients had good to excellent OKS outcomes (48, 48, 48 and 38). Of the remaining 85 medial UKP, 44 UKP (51.2%) were cemented and 41 (48.8%) were cementless UKP. The AKSS scores were slightly better in the cementless group 94.5 vs 90.2 (P = 0.055) for the objective score and 91.2 vs 87.8 (P = 0.25) for the subjective score, both not significantly different (Figure 1). The SF-12 scores were not significantly different in the cementless group, with a mean Physical Component Summary (PCS) score of 49.5 vs 47.6 (P = 0.28) and Mental Component Summary (MCS) score of 55.3 vs 54.5 (P = 0.60).
There were no cases of thrombosis or deep infection. No vascular or neurological complications occurred. No fractures were observed post-operatively in this cohort. One patient experienced a length difference of the operated leg after a total hip replacement, which resulted in an inappropriate gait pattern and led to pain in the knee in which the medial UKP was implanted (VAS score 76, OKS 9, Kujala 26).
With this cross-sectional study we wanted to compare the short-term clinical outcomes of the cemented and the cementless Oxford phase III medial UKP performed in an independent center by one single surgeon. We achieved a good to excellent short-term clinical outcome of both the cemented and the cementless Oxford UKP. Although not significant different, the cementless UKP showed better clinical results compared to the cemented UKP. These results support the good clinical results of the Oxford study group[12,13].
In three cases (sub)luxation of the PE bearing occurred. PE bearing exchange with a good clinical outcome was not considered as a revision, but was listed as a reoperation (Table 2). In four cases the patient experienced impingement of the PE bearing, because of bony- or soft tissue re-growth at the bone ridge cranial to the anterior side of the femur condyle.
Patients requiring a reoperation were significantly younger and more frequently male. In earlier Oxford UKP survival studies gender has shown not to affect UKP survival. Whether age under 60 years old influences the survival rates is still a discussion. The Oxford group has shown in their studies no significant difference between survival in patients under and over 60 years old[13]. Worldwide registers and other independent studies however show higher revision rates in patients under 60 years old[14-16]. Patients aged under 60 in the reoperation group were relatively active patients, which we think might be part of the explanation for (sub)luxation. Impingement might be caused by too little bone resection cranial to the anterior side of the femur component or because of re-growth. We currently use the microplasty instrumentation and aim for a resection of approximately 10 mm caudal to the femur component, which seems to reduce the amount of patients with signs of anterior impingement.
Based on our results and experience, we believe that if there is an obvious reason for pain in a medial UKP, a reoperation can be successful and it prevents (early) revision surgery. This does require accurate patient selection, based on physical examination and radiologic reviewing by an experienced surgeon.
There were no revisions in the cementless group. Of the cemented UKP, three had to be revised to a TKP, two of these revisions were performed in our clinic. Reasons for revision were malposition, aseptic loosening of the tibia component and progression of OA in the lateral and patellofemoral compartments. The time to revision varied between 16-27 mo. Two of the revisions were performed within the first two years after implantation. Generally, it is not recommended to revise a medial UKP to a TKP in the first two years after implantation, because of tibial stress and the bone remodeling that occurs. In this phase, medial pain is common and a bone scintigraphy can show false-positive results. Unless there is an obvious reason for failure of the UKP, revision to a TKP in this phase can be unsatisfying[13].
The revision rates of the cemented UKP lie in between the excellent results of the Oxford study group[13] and the Joint registry reports[17].
Surgical errors play a considerable role in UKP failure, as over-correction of an existing valgus deformity, overstuffing and cementing technique are frequently reported reasons for revision[17]. With the cementless UKA, cementing errors such as uneven distribution of the cement, cement residue posterior and loose particles, are eliminated. It is also known that cemented medial UKP show physiological radiolucent lines at follow-up, a phenomenon that is less seen in the cementless medial UKP[3]. Physiological radiolucent lines after medial UKP can easily be mistaken for radiolucency due to aseptic loosening. These factors may contribute to lower revision rate in cementless medial UKP compared to cemented medial UKP[1].
The cementless UKP needs an adequate initial fixation. Although not observed in this cohort, peri-prosthetic tibia plateau fractures are more frequently observed in cementless UKP. This might be due to a deep posterior tibial cortical cut or due to hard hammering, both should be avoided.
The strength of this study is the specialized character of our clinic and the choice to only include patients operated by one single surgeon. The occurrence of surgical errors is related to the frequency of the operation performed and the experience of the surgeon and his staff[17]. Our clinic is specialized in sports-, arthroscopic- and prosthetic surgery. We perform approximately 200 UKP per year of which more than half are performed by the senior author (Marcel JM Driessen). By comparing the clinical outcome of the cemented and cementless UKP performed by a single surgeon, we eliminated a surgeon bias for indication as well as a bias in surgical technique. Limitations of this study are the cross-sectional design and the relatively short follow-up time.
The cementless Oxford phase III medial UKP shows promising short-term clinical outcome when used in a specialized orthopedic center. Because of the promising results of the cementless Oxford phase III medial UKP, it is now the most used medial UKP in our clinic for eligible patients.
We would like to thank Arne Heneweer MSc. for biostatistical review.
The unicondylar knee prosthesis (UKP) is an established treatment for end-stage osteoarthritis (OA) of the knee and accounts for around 8%-10% of all primary knee replacements. One of the successful implants used, is the cemented Oxford medial UKP phase III. This is a fully congruent mobile bearing prosthesis, which is implanted via a minimal invasive procedure with minimal bone-loss. The success of the medial UKP is still largely related to the indication for surgery and the experience of the surgeon and the surgical team. The higher revision rates in unicondylar arthroplasty are a concern. The difference in revision rate between a UKP and a total knee prosthesis (TKP) is likely to be multi-factorial. A major issue seems to be the ease of choosing for a revision of a UKP compared to a TKP.
The developing hospital has published encouraging results of the cementless Oxford phase III medial UKP, as well has cementless UKP by other manufacturers.
With the introduction of the cementless Oxford UKP (2003) one of the technical errors related to failure, the cementing technique can be eliminated. Also, the cementless Oxford medial UKP shows reduced radiolucent lines at one year follow-up, whereas the cemented Oxford medial UKP shows occurrence of radiolucent lines during follow-up. The occurrence of radiolucent lines is thought to be a misleading factor for revision in patients with unexplained pain after cemented UKP. In accordance with earlier published results, it is our experience that the cementless Oxford UKP performs as well as, or even better than the cemented Oxford UKP.
With this retrospective study the authors want to compare the short-term clinical outcome of the cemented and the cementless Oxford phase III medial UKP performed in an independent center by one single surgeon.
This is a good article.
P- Reviewer: Gill TK S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Robertsson O, Knutson K, Lewold S, Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001;83:45-49. [PubMed] [Cited in This Article: ] |
| 2. | Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128-135. [PubMed] [Cited in This Article: ] |
| 3. | Pandit H, Jenkins C, Beard DJ, Gallagher J, Price AJ, Dodd CA, Goodfellow JW, Murray DW. Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J Bone Joint Surg Br. 2009;91:185-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Saxler G, Temmen D, Bontemps G. Medium-term results of the AMC-unicompartmental knee arthroplasty. Knee. 2004;11:349-355. [PubMed] [Cited in This Article: ] |
| 5. | Forsythe ME, Englund RE, Leighton RK. Unicondylar knee arthroplasty: a cementless perspective. Can J Surg. 2000;43:417-424. [PubMed] [Cited in This Article: ] |
| 6. | Magnussen PA, Bartlett RJ. Cementless PCA unicompartmental joint arthroplasty for osteoarthritis of the knee. A prospective study of 51 cases. J Arthroplasty. 1990;5:151-158. [PubMed] [Cited in This Article: ] |
| 7. | Haverkamp D, Breugem SJ, Sierevelt IN, Blankevoort L, van Dijk CN. Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop. 2005;76:347-352. [PubMed] [Cited in This Article: ] |
| 8. | Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159-163. [PubMed] [Cited in This Article: ] |
| 9. | Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171-1178. [PubMed] [Cited in This Article: ] |
| 10. | Van Der Straeten C, Witvrouw E, Willems T, Bellemans J, Victor J. Translation and validation of the Dutch new Knee Society Scoring System ©. Clin Orthop Relat Res. 2013;471:3565-3571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:7-72. [PubMed] [Cited in This Article: ] |
| 12. | Pandit H, Liddle AD, Kendrick BJ, Jenkins C, Price AJ, Gill HS, Dodd CA, Murray DW. Improved fixation in cementless unicompartmental knee replacement: five-year results of a randomized controlled trial. J Bone Joint Surg Am. 2013;95:1365-1372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Liddle AD, Pandit H, O’Brien S, Doran E, Penny ID, Hooper GJ, Burn PJ, Dodd CA, Beverland DE, Maxwell AR. Cementless fixation in Oxford unicompartmental knee replacement: a multicentre study of 1000 knees. Bone Joint J. 2013;95-B:181-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC. Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee. 2010;17:48-52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 110] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 15. | Matharu G, Robb C, Baloch K, Pynsent P. The Oxford medial unicompartmental knee replacement: survival and the affect of age and gender. Knee. 2012;19:913-917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Kort NP, van Raay JJ, van Horn JJ. The Oxford phase III unicompartmental knee replacement in patients less than 60 years of age. Knee Surg Sports Traumatol Arthrosc. 2007;15:356-360. [PubMed] [Cited in This Article: ] |
| 17. | Labek G, Sekyra K, Pawelka W, Janda W, Stöckl B. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop. 2011;82:131-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |