Published online Mar 18, 2016. doi: 10.5312/wjo.v7.i3.195
Peer-review started: December 14, 2015
First decision: January 4, 2016
Revised: January 9, 2016
Accepted: January 27, 2016
Article in press: January 29, 2016
Published online: March 18, 2016
Processing time: 89 Days and 14.5 Hours
AIM: To investigate knee awareness and functional outcomes in patients treated with simultaneous bilateral vs unilateral total knee arthroplasty (TKA).
METHODS: Through a database search, we identified 210 patients who had undergone unilateral TKA (UTKA) and 65 patients who had undergone simultaneous bilateral TKA (SBTKA) at our institution between 2010 and 2012. All TKAs were cemented and cruciate retaining. The mean follow-up period was 3.2 (2 to 4) years. All the patients had symptomatic and debilitating unilateral or bilateral osteoarthritis for which all conservative and non-surgical treatments were failed, thus preoperatively the patients had poor functionality. All patients were asked to complete Forgotten Joint Score (FJS) and Oxford Knee Score (OKS) questionnaires. The patients were matched according to age, gender, year of surgery, Kellgren-Lawrence score and pre- and postoperative overall knee alignment. The FJS and OKS questionnaire results of the two groups were then compared.
RESULTS: A mixed-effects model was used to analyze differences between SBTKA and UTKA. OKS: The mean difference in the OKS between the patients who had undergone SBTKA and those who had undergone UTKA was 1.5, which was not statistically significant (CI = -0.9:4.0, P-value = 0.228). The mean OKS of the SBTKA patients was 37.6 (SD = 9.0), and the mean OKS of the UTKA patients was 36.1 (SD = 9.9). FJS: The mean difference in the FJS between the patients who had undergone SBTKA and those who had undergone UTKA was 2.3, which was not statistically significant (CI = -6.2:10.8, P-value = 0.593). The mean FJS of the SBTKA patients was 59.9 (SD = 27.5), and the mean FJS of the UTKA patients was 57.5 (SD = 28.8).
CONCLUSION: SBTKA and UTKA patients exhibited similar joint functionality and knee awareness. Our results support the use of SBTKA in selected patients suffering from clinically symptomatic bilateral osteoarthritis.
Core tip: We investigated the functional outcomes and knee awareness of patients who had undergone simultaneous bilateral compared with those who had undergone unilateral total knee arthroplasty (TKA). To accomplish this, we used the well-known Oxford Knee Score and the recently introduced Forgotten Joint Score (FJS). The FJS is based on a novel concept, or a patient’s ability to forget about an artificial joint as a result of successful treatment; this result is considered as the ultimate goal of joint replacement surgery. No differences in final outcomes were observed between the groups. Therefore, individuals for whom bilateral TKA is indicated should be offered this option.
- Citation: Latifi R, Thomsen MG, Kallemose T, Husted H, Troelsen A. Knee awareness and functionality after simultaneous bilateral vs unilateral total knee arthroplasty. World J Orthop 2016; 7(3): 195-201
- URL: https://www.wjgnet.com/2218-5836/full/v7/i3/195.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i3.195
The number of patients undergoing simultaneous bilateral total knee arthroplasty (SBTKA) has steadily increased. Currently, approximately 6% of all total knee arthroplasties (TKAs) performed in the United States are simultaneous bilateral procedures[1].
The potential benefits of SBTKA compared with staged procedures include a decreased length of hospitalization, decreased time under anesthesia, decreased rehabilitation time, and decreased cost to the healthcare system[2-5]. The disadvantages of SBTKA include an increased need for blood transfusions and increased physiological stress induced by simultaneous surgery[1,6-9]. Although these benefits and disadvantages are accepted in the medical community, it remains a matter of debate whether functional outcomes, pain relief and patient satisfaction are equivalent between bilateral and staged procedures.
The need to rehabilitate two knees after SBTKA could be hypothesized to result in inferior functional outcomes for each knee compared with those achieved following rehabilitation of a single knee, as in unilateral TKA (UTKA)[10]. Furthermore, the increased length of time required to perform SBTKA compared with UTKA could result in inferior technical performance toward the end of the procedure. This decreased performance could possibly be reflected in functional outcomes and knee awareness[11]. Hence, functional outcomes and knee awareness following SBTKA could be inferior following UTKA according to the two aforementioned hypotheses. If functional outcomes and knee awareness are indeed inferior after SBTKA relative to UTKA, then the indications for performing SBTKA will be limited, and reconsideration of current SBTKA treatment strategies will be warranted.
The purpose of this study was to compare knee awareness and functional outcomes between patients who had undergone SBTKA and those who had undergone primary UTKA.
This study was performed in accordance with the Declaration of Helsinki of the World Medical Association.
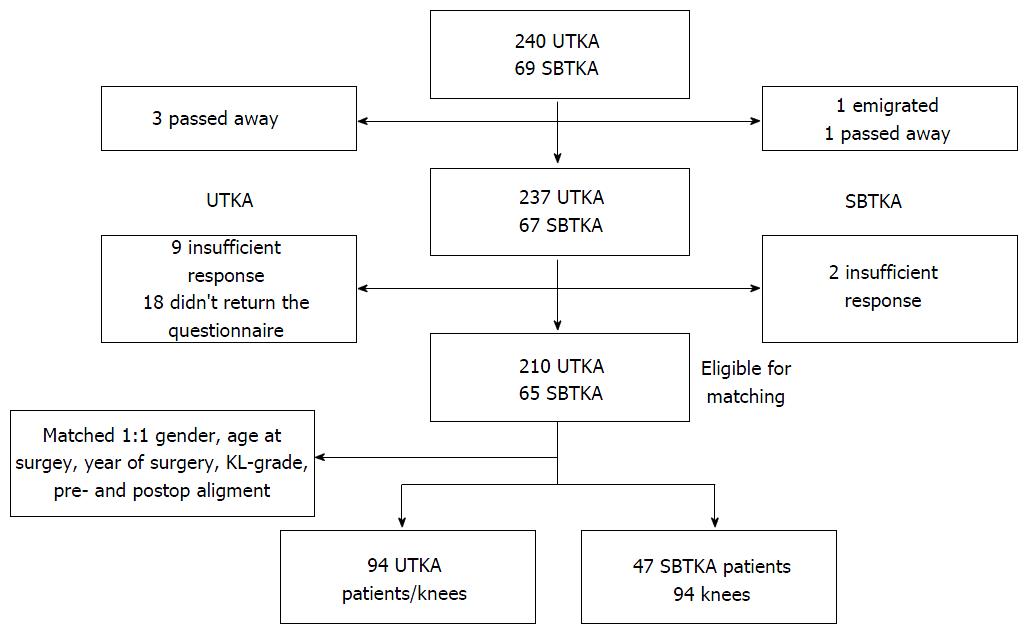
In the current retrospective, matched, case-control cohort study, we identified 69 patients who had undergone SBTKA with insertion of prostheses with the same TKA design in both knees at our institution between January 2010 and December 2012. During that period, the same TKA design was used in 240 UTKA procedures. Selected patients had symptomatic and debilitating unilateral or bilateral osteoarthritis for which conservative and non-surgical treatments were failed. Hence, preoperatively all the patients had poor functional performance. These UTKA patients were enrolled in the study as controls. The large size of the UTKA group ensured that as many patients as possible could be matched. Patients who had undergone knee surgery before primary TKA or who had undergone revision surgery with replacement of the prosthetic components after primary TKA were excluded. All TKA procedures had been performed using a medial para-patellar approach and were cemented and cruciate retaining (AGC, Biomet, Warsaw, Indiana). Additionally, all procedures included patellar resurfacing. The AGC prosthesis is a widely used TKA system that demonstrated good clinical results and longevity in earlier studies[12-14]. All patients had undergone surgery in a fast-track setting and had followed the same standardized postoperative rehabilitation program[15]. Patients had been selected for SBTKA if they had bilateral disabling osteoarthritis and no cardiopulmonary comorbidity (ASA 1 to 2).
Gender, age at the time of surgery and year of surgery were documented for all patients. Preoperative radiographs were available for all knees and were analyzed for the degree of osteoarthritis using the Kellgren-Lawrence (KL) grading scale[16,17]. Pre- and postoperative anteroposterior knee anatomical alignment was measured using short-film radiographs according to the method described by Petersen et al[18]. The same observer performed all radiographic assessments.
SBTKA patients and UTKA controls were invited to participate in this study in January 2014. Each patient received Forgotten Joint Score (FJS) and Oxford Knee Score (OKS) questionnaires. The patients in the UTKA group received one set of questionnaires, whereas those in the SBTKA group received two sets of questionnaires, with one clearly marked for each knee. The questionnaire responses left 65 SBTKA and 210 UTKA patients eligible for matching and further analysis.
Each knee in the SBTKA group was matched 1:1 to the knees in the UTKA group regarding gender, age at the time of surgery, year of surgery, KL grade and pre- and postoperative anatomical knee alignment (Table 1). This resulted in a study cohort of 94 knees in 47 patients in the SBTKA group and 94 knees in 94 patients in the UTKA group. The FJS and OKS were then calculated and compared between the matched groups. The follow-up period in this study was 2 to 4 years (mean 3.2 years). A flow chart describing the study’s participants can be found in Figure 1.
| Bilateral | Unilateral | ||
| Gender, No. of knees (%) | Male | 34 (36%) | 34 (36%) |
| Female | 60 (64%) | 60 (64%) | |
| Age at operation, mean (SD) range | 66 yr (8.2) | 65 yr (7.4) | |
| 45, 81 | 46, 80 | ||
| Osteoarthritis grade, No. of knees (%) | KL 1 + 2 | 27 (29%) | 27 (29%) |
| KL 3 + 4 | 67 (71%) | 67 (71%) | |
| Alignment, mean (SD) range | Preoperative | 1.2 (5.3) | 1.3 (5.9) |
| -16.3, 16.21 | -12.1, 21.81 | ||
| Postoperative | 5.2 (3.0) | 4.9 (3.4) | |
| -1.1, 12.81 | -11.2, 12.81 | ||
| Operation year, No. of knees (%) | 2010 | 24 (26%) | 24 (26%) |
| 2011 | 62 (66%) | 62 (66%) | |
| 2012 | 8 (9%) | 8 (9%) |
For all participants, the OKS was calculated. The range of the OKS is 0 to 48, with 48 being the best possible score[19].
The FJS[20] is based on a 12-item questionnaire that evaluates a patient’s ability to forget about his or her artificial joint in everyday life (awareness of the knee). The range for the FJS is 0 to 100, with 100 being the best possible score; the properties of the FJS questionnaire have been reported in earlier studies[20-22].
The data used in the current study were sufficiently anonymized, and The Danish National Data Protection Agency approved the project (AHH-2014-010).
The statistical methods used in this study were reviewed by Thomas Kallemose, a biomedical statistician from Clinical Research Center, Copenhagen University Hospital Hvidovre, Kettegaard Alle 30, DK-2650 Hvidovre, Copenhagen, Denmark.
Matching was performed for all patients who completed both the FJS and the OKS questionnaires. The matching was prioritized by operation year, gender, KL score, age at the time of surgery, postoperative anatomical knee alignment and preoperative anatomical knee alignment. The year of surgery was most highly prioritized because of the small amount of overlap between the UTKA and the SBTKA patients. Pooled squared differences corresponding to age at the time of surgery, postoperative anatomical knee alignment and preoperative anatomical knee alignment were used to determine the best matching; 100000 permutations were used, and the best was selected based on the smallest pooled squared difference.
Sample size estimation was based on the ability to detect an inter-group difference (power 90%, P-level 0.05, SD: 10) of 5 points or more (considered to be clinically relevant) in the OKS. This resulted in a need for 85 cases per group.
A mixed-effects model was used to assess the differences between UTKA and SBTKA patients in terms of both the FJS and the OKS. The score difference between the UTKA and the SBTKA patients within each matched knee pair was used as an outcome in the model. Because of the assumed within-patient variance in the SBTKA group, a random effect corresponding to the SBTKA patients’ scores was added. Because of the matching, no other factors were added to the model. A P-value less than 0.05 was considered statistically significant. All matching and analyses were performed using R 3.02 (R Foundation for Statistical Computing, Vienna, Austria).
The mean difference in the OKS between the SBTKA and the UTKA groups was 1.5, which was not statistically significant (CI = -0.9:4.0, P-value = 0.228). The mean OKS was 37.6 (SD = 9.0) in the SBTKA group, and it was 36.1 (SD = 9.9) in the UTKA group (Table 2).
| SBTKA | UTKA | ||
| PROM outcomes, mean (SD) range | OKS | 37.6 (9.0) | 36.1 (9.9) |
| 10, 48 | 9, 48 | ||
| FJS | 59.9 (27.5) | 57.5 (28.8) | |
| 0, 100 | 0, 100 |
The mean difference in the FJS between the SBTKA and the UTKA groups was 2.3, which was not statistically significant (CI = -6.2:10.8, P-value = 0.593). The mean FJS was 59.9 (SD = 27.5) in the SBTKA group, and it was 57.5 (SD = 28.8) in the UTKA group (Table 2).
Whether the advantages of SBTKA outweigh its potential disadvantages has been a topic of much debate. Numerous studies have investigated the risk of perioperative complications after SBTKA[1,4-9,23-29] and the cost-effectiveness of the procedure[2,30-33] in comparison with UTKA. However, the majority of these studies have not focused on long-term functional outcomes or knee awareness. In the current study, we investigated functional outcomes and knee awareness during daily-living activities using patient-reported outcome measures following SBTKA and UTKA.
We hypothesized that the longer duration required to perform SBTKA could lead to inferior technical performance when operating on the second knee and that difficulties during postoperative rehabilitation of two knees after SBTKA could result in an overall inferior functional outcome and higher knee awareness compared with those for UTKA. We found that the SBTKA group did not significantly differ from the UTKA group with respect to functional outcomes or knee awareness at 2 to 4 years post-surgery. This result is consistent with the findings from a previous study[34], in which 150 consecutive, but selected, SBTKA cases were compared with 271 UTKA cases in a standardized fast-track setting between 2003 and 2009. Husted et al[34] demonstrated that the outcome at three months and two years was similar or better in the SBTKA group with regard to satisfaction, the range of motion, pain, the use of a walking aid and the ability to work and perform activities of daily living. However, this previous study did not use a validated PROM, such as those used in the present study.
In a retrospective review of 697 TKAs in 511 consecutive patients (SBTKA: 186, UTKA: 325) with bilateral knee arthritis and a follow-up period of 2 to 8 years, using the Knee Society Score and its subscales as endpoints, Bagsby and Pierson[35] demonstrated a statistically significant better postoperative functional outcome, including an increased total range of motion (P = 0.001), improved flexion (P = 0.003), and an increased function score (P < 0.001) associated with SBTKA. They presumed that this finding was related to the absence of contralateral arthritis, which would produce pain and restrict rehabilitation. This contradicts our hypothesis that simultaneous surgeries on two knees would make rehabilitation more difficult and potentially result in an inferior outcome compared with that associated with UTKA. However, their findings are ultimately consistent with our conclusions regarding the performance of SBTKA.
In a study by Zeni and Snyder-Mackler[36], 15 subjects who had undergone SBTKA were observed prospectively for a period of 2 years. Subjects in this group were matched with subjects who had undergone UTKA by age, sex and BMI, providing equal samples of 15 subjects in each group. These 2 groups were then compared with a group of 21 orthopedically healthy subjects, which served as the control group. Pre- and post-operative self-reported functional measures and objective clinical tests were then applied to the groups. At 2 years, the long-term outcomes of the bilateral group were similar to those of the matched sample of patients who had undergone UTKA and to those of the control subjects. These findings are again in accordance with the findings of the current study, which unanimously support the practice of SBTKA according to the long-term outcomes.
Seo et al[11] reviewed SBTKA outcomes in 420 patients at 1 year post-surgery. Similar to what was hypothesized in the current study, they hypothesized that the postoperative results produced by SBTKA would vary as a result of disparate surgical scenarios between knees. In support of their hypothesis, they found that the second TKA had a greater incidence of outliers in limb coronal alignment (16.2% vs 9.0%, P = 0.003), more blood loss (735 mL vs 656 mL, P < 0.001) and a slightly longer operation time (61 min vs 58 min, P < 0.001) compared with the first TKA. This supports our hypothesis that lengthier surgeries could lead to inferior technical performance near the end of a procedure, possibly resulting in inferior functional outcomes and higher knee awareness of the knee operated on last. However, at the 1-year follow-up, neither knee showed a difference in its range of motion after surgery (P = 1.000). The postoperative flexion angle improved equally, to 129° and 127°. Moreover, no significant differences in the postoperative Knee Society Function Score or the total Western Ontario and McMaster Universities Arthritis Index scores were observed between the sides (P = 0.316 and 1.000, respectively).
However, a significant difference in the postoperative Knee Society Knee Score was observed (P < 0.001). Concerns that SBTKA produces inferior functional outcomes in one or both knees thus appear to be unwarranted.
A review of previous SBTKA studies concluded that there are no sound counterarguments against the orthopedic advantages of SBTKA[8]. Any remaining debate centers on medical and anesthetic contraindications. Age and preoperative comorbidities play important roles in postoperative morbidity and mortality. In addition, 81% of the participants in the Consensus Conference on Bilateral Total Knee Arthroplasty Group[37] agreed that SBTKA is associated with an increased risk of perioperative adverse events when performed on unselected patients. The consensus group also agreed that physicians and hospitals should consider using more restrictive patient selection criteria and should exclude those with a modified cardiac risk index greater than 3 to mitigate the potentially increased risk of adverse events. Furthermore, the entire group agreed that when there is a conflict between orthopedic need and medical adequacy with regard to SBTKA, the medical concern for a patient’s safety should prevail over the orthopedic need. Hence, only patients with no evidence of cardiopulmonary disease, ASA scores of 1 or 2 and bilateral disabling osteoarthritis are considered as acceptable candidates for SBTKA at our institution. In the current study, because cardiopulmonary disease tends to increase with age, we found that patients in the SBTKA group were younger before matching was performed. It can be argued that younger patients might experience fewer degenerative changes in the knees. To account for this, we matched the SBTKA and UTKA groups in terms of gender, age at the time of surgery, year of surgery, KL grade and pre- and postoperative anatomical knee alignment to minimize potential bias.
The FJS has recently been introduced and validated as a post-surgical assessment tool for total joint replacement[20]. The FJS specifically evaluates a patient’s level of awareness of their artificial joint in 12 scenarios commonly encountered in daily life. Joint awareness includes strong sensations, such as pain, and the ability to perform activities of daily living, as well as more subtle feelings, such as mild stiffness, subjective dysfunction and any other discomfort that a patient might encounter. The forgotten joint concept, which is based on the level of knee awareness, is a more discerning assessment method that has shown better discriminatory power and less of a ceiling effect than traditional questionnaires measuring pain or function do. These features are especially appealing for more active patients with good to excellent outcomes after TKA. The FJS also allows detection of potential subtle differences between patients and between follow-up time points[20,21].
The current study has certain limitations. We matched patients according to the abovementioned parameters, whereas other factors (e.g., BMI, social status, psychological profile, preoperative duration and pain intensity, comorbidities and ASA score) that may potentially affect functional outcomes and knee awareness, were not accounted for in this study. However we have chosen parameters, which have a high influence on functional outcomes and involved in this study. The primary strength of the present study is the matching of patients between the study groups in terms of gender, age at the time of surgery, KL grade and pre- and postoperative knee alignment. Because of this matching procedure, we believe that our study groups are comparable, counteracting the study’s limitations.
SBTKA and UTKA patients exhibit similar knee function and knee awareness. Our results support the use of SBTKA in selected patients without cardiopulmonary comorbidity who suffer from clinically symptomatic bilateral osteoarthritis.
The potential benefits of simultaneous bilateral total knee arthroplasty (TKA) include a decreased overall length of hospitalization, shorter overall anesthesia time and decreased cost to both the patient and the institution. Although many prior studies examining differences between unilateral and bilateral TKA have focused on short-term postoperative outcomes, costs, and complications, few have assessed differences in long-term results and functional outcomes.
To the authors’ knowledge, this is the first review to analyze patient-reported outcomes (PROs) after simultaneous bilateral TKA using the newly introduced Forgotten Joint Score (FJS). The FJS was validated in Danish in a parallel study at the authors’ institution and was used to compare PROs between simultaneous bilateral TKA patients and unilateral TKA patients.
Several reports have shown the potential effects of knee alignment on PRO measures after TKA. Therefore, the authors measured osteoarthritis severity and pre- and post-operative overall knee alignment based on the radiographs of 340 patients. Moreover, the authors used the forgotten joint concept, which is a more discerning assessment method that has shown better discriminatory power and less of a ceiling effect than traditional questionnaires measuring pain or function do. These features are especially appealing for more active patients with good to excellent outcomes after TKA. The authors obtained perfect matching regarding age, gender, year of surgery, Kellgren-Lawrence score and pre- and post-operative overall knee alignment, which allowed comparison of parameters of interest without confounding by other elements. Concurrently with the FJS, the authors also used the well-known Oxford Knee Score (OKS) to investigate patient functionality after joint replacement.
The results support the use of simultaneous bilateral TKA in selected patients without cardiopulmonary comorbidity who suffer from clinically symptomatic bilateral osteoarthritis.
This is an interesting retrospective study. The patients were evaluated using subjective scores (FJS and OKS Questionnaires) and therefore the results are “more reliable”.
P- Reviewer: Drosos GI, Willis-Owen CA S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Memtsoudis SG, Mantilla CB, Parvizi J, Stundner O, Mazumdar M. Have bilateral total knee arthroplasties become safer? A population-based trend analysis. Clin Orthop Relat Res. 2013;471:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Kovacik MW, Singri P, Khanna S, Gradisar IA. Medical and financial aspects of same-day bilateral total knee arthroplasties. Biomed Sci Instrum. 1997;33:429-434. [PubMed] |
| 3. | Dennis DA. Debate: bilateral simultaneous total knee arthroplasty. Clin Orthop Relat Res. 2004;428:82-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Patil N, Wakankar H. Morbidity and mortality of simultaneous bilateral total knee arthroplasty. Orthopedics. 2008;31:780-789; quiz 780-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Stubbs G, Pryke SE, Tewari S, Rogers J, Crowe B, Bridgfoot L, Smith N. Safety and cost benefits of bilateral total knee replacement in an acute hospital. ANZ J Surg. 2005;75:739-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Fabi DW, Mohan V, Goldstein WM, Dunn JH, Murphy BP. Unilateral vs bilateral total knee arthroplasty risk factors increasing morbidity. J Arthroplasty. 2011;26:668-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 150] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Noble J, Goodall JR, Noble DJ. Simultaneous bilateral total knee replacement: a persistent controversy. Knee. 2009;16:420-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Oakes DA, Hanssen AD. Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks. Clin Orthop Relat Res. 2004;428:87-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Bakırhan S, Angın S, Karatosun V, Ünver B, Günal I. Physical performance parameters during standing up in patients with unilateral and bilateral total knee arthroplasty. Acta Orthop Traumatol Turc. 2012;46:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Seo JG, Lee BH, Moon YW, Chang MJ, Park SH. Disparate postoperative results in the first and second knees on simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2014;29:2331-2336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Ritter MA. The Anatomical Graduated Component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg Br. 2009;91:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Worland RL, Johnson GV, Alemparte J, Jessup DE, Keenan J, Norambuena N. Ten to fourteen year survival and functional analysis of the AGC total knee replacement system. Knee. 2002;9:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Thomsen MG, Husted H, Otte KS, Holm G, Troelsen A. Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial. BMC Musculoskelet Disord. 2013;14:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79:168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 428] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 16. | Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9311] [Cited by in RCA: 8877] [Article Influence: 130.5] [Reference Citation Analysis (0)] |
| 17. | Kijowski R, Blankenbaker D, Stanton P, Fine J, De Smet A. Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol. 2006;187:794-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Petersen TL, Engh GA. Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty. 1988;3:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 177] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 655] [Cited by in RCA: 919] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 20. | Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27:430-436.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 577] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 21. | Thienpont E, Opsomer G, Koninckx A, Houssiau F. Joint awareness in different types of knee arthroplasty evaluated with the Forgotten Joint score. J Arthroplasty. 2014;29:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 22. | Giesinger K, Hamilton DF, Jost B, Holzner B, Giesinger JM. Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthritis Cartilage. 2014;22:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 23. | Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl. 2012;83:1-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 193] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 24. | Andersen LØ, Husted H, Otte KS, Kristensen BB, Kehlet H. A compression bandage improves local infiltration analgesia in total knee arthroplasty. Acta Orthop. 2008;79:806-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Andersen LØ, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia. 2009;64:508-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 26. | Bullock DP, Sporer SM, Shirreffs TG. Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am. 2003;85-A:1981-1986. [PubMed] |
| 27. | Fick D, Crane T, Shakespeare D. A comparison of bilateral vs. unilateral total knee arthroplasty mobilised using a flexion regime. Knee. 2002;9:285-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Leonard L, Williamson DM, Ivory JP, Jennison C. An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2003;18:972-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 29. | Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Joint Surg Am. 2003;85-A:1532-1537. [PubMed] |
| 30. | Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;428:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Jankiewicz JJ, Sculco TP, Ranawat CS, Behr C, Tarrentino S. One-stage versus 2-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;309:94-101. [PubMed] |
| 32. | Lane GJ, Hozack WJ, Shah S, Rothman RH, Booth RE, Eng K, Smith P. Simultaneous bilateral versus unilateral total knee arthroplasty. Outcomes analysis. Clin Orthop Relat Res. 1997;345:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 78] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13:172-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 209] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 34. | Husted H, Troelsen A, Otte KS, Kristensen BB, Holm G, Kehlet H. Fast-track surgery for bilateral total knee replacement. J Bone Joint Surg Br. 2011;93:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 35. | Bagsby D, Pierson JL. Functional outcomes of simultaneous bilateral versus unilateral total knee arthroplasty. Orthopedics. 2015;38:e43-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 36. | Zeni JA, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25:541-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Memtsoudis SG, Hargett M, Russell LA, Parvizi J, Cats-Baril WL, Stundner O, Sculco TP. Consensus statement from the consensus conference on bilateral total knee arthroplasty group. Clin Orthop Relat Res. 2013;471:2649-2657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |