Published online Nov 18, 2016. doi: 10.5312/wjo.v7.i11.752
Peer-review started: March 24, 2016
First decision: July 5, 2016
Revised: August 6, 2016
Accepted: September 7, 2016
Article in press: September 8, 2016
Published online: November 18, 2016
To compare outcomes of our revision surgical operations in obstetric brachial plexus palsy (OBPP) patients to results of conventional operative procedures at other institutions.
We analyzed our OBPP data and identified 10 female and 10 male children aged 2.0 to 11.8 years (average age 6.5 years), who had prior conventional surgical therapies at other clinics. Of the 20 patients, 18 undergone triangle tilt, 2 had only mod Quad. Among 18 patients, 8 had only triangle tilt and 10 had also mod Quad as revision surgeries with us. We analyzed the anatomical improvements and functional modified Mallet statistically before and after a year post-revision operations.
Pre-revision surgery average modified Mallet score was 12.0 ± 1.5. This functional score was greatly improved to 18 ± 2.3 (P < 0.0001) at least one-year after revision surgical procedures. Radiological scores (PHHA and glenoid version) were also improved significantly to 31.9 ± 13.6 (P < 0.001), -16.3 ± 11 (P < 0.0002), at least one-year after triangle tilt procedure. Their mean pre-triangle tilt (yet after other surgeon’s surgeries) PHHA, glenoid version and SHEAR were 14.6 ± 21.7, -31.6 ± 19.3 and 16.1 ± 14.7 respectively.
We demonstrate here, mod Quad and triangle tilt as successful revision surgical procedures in 20 OBPP patients, who had other surgical treatments at other clinics before presenting to us for further treatment.
Core tip: We compared functional and anatomical improvements from our revision surgical treatment experiences to outcomes of other surgical treatments at other institutions in 20 obstetric brachial plexus palsy (OBPP) children. Pre-revision surgery mean modified Mallet scores and shoulder anatomical measurements were improved statistically highly significantly at least one-year after revision surgeries. We demonstrate here, mod Quad and triangle tilt as successful revision surgical procedures in 20 OBPP patients, who had other surgical treatments at other clinics before presenting to us for further treatment.
- Citation: Nath RK, Somasundaram C. Improvements after mod Quad and triangle tilt revision surgical procedures in obstetric brachial plexus palsy. World J Orthop 2016; 7(11): 752-757
- URL: https://www.wjgnet.com/2218-5836/full/v7/i11/752.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i11.752
Poor recovery of neurological function in obstetric brachial plexus palsy (OBPP) results in muscle weakness and imbalances around the shoulder[1-3]. Progressive muscle imbalance causes bony deformities at the shoulder joint, affecting it’s movements and functions[4,5]. Many traditional surgical interventions have been reported to improve the upper extremity functions in OBPP patients[6-11].
Muscle release and tendon transfer procedures have been shown[12-19] to reduce the muscle contractures and improve shoulder movements. Humeral rotational osteotomy corrects the arm at resting position, but does not address the glenohumeral and Scapular Hypoplasia, Elevation and Rotation (SHEAR) deformities. These surgical treatments do not address these two osseous deformities.
We have published extensively the effectiveness of triangle tilt surgery in correcting glenohumeral joint incongruity and thereby improving upper extremity functions in OBPP patients[20-28]. Here, we show both functional and anatomical improvements significantly after triangle tilt and or mod Quad as revision surgeries in 20 OBPP patients, who had other surgical treatments at outside clinics before visiting our clinic for further treatment.
We analyzed our OBPP data and identified 10 female and 10 male patients, aged 2.0 to 11.8 years (average age 6.5 years), who had operative procedures at other clinics.
Of the 20 OBPP patients in our present study group, 8 patients undergone only the bony procedure, triangle tilt and 10 had both triangle tilt and mod Quad (Tables 1 and 2). Therefore, these 18 patients (Table 2) have anatomical and radiological scores (PHHA, SHEAR and glenoid version), in addition to functional modified Mallet scale (Table 1). Two patients, number 19 and 20 in Table 1, underwent only mod Quad procedure, as they did not have shoulder subluxation. Therefore, these two patients did not need to undergo triangle tilt procedure, which addresses shoulder subluxation. Modified Mallet and radiological scores were measured, statistically analyzed to compare. All measurements were done at least one-year after surgical treatments.
| Patients | Other surgeons’ surgery | Gender | Age (yr) | Nerve involved | TT/MQ | Total Mallet pre- revision surgery | Total Mallet post- revision surgery |
| 1 | Botox | F | 2.5 | C5-C7 | TT | 13 | 23 |
| 2 | Partial MQ, subscap release lat dorsi rerouting | M | 6.4 | C5-C7 | TT | 11 | 16 |
| 3 | Neurolysis/nerve graft | F | 4.2 | Total | TT and MQ | 13 | 18 |
| 4 | Humeral osteotomy | F | 11.1 | C5-C7 | TT and MQ | 11 | 15 |
| 5 | Neuroma excision, nervegraft | M | 11.8 | Total | TT | 11 | 14 |
| 6 | Nerve graft, HO, botox | F | 7.1 | Total | TT | 11 | 17 |
| 7 | Coracoacromial release/coracoid resection | M | 5.5 | C5-C7 | TT | 14 | 21 |
| 8 | Botox | M | 11.3 | C5-C7 | TT and MQ | 10 | 15 |
| 9 | Sural nerve graft | F | 5.0 | Total | TT | 10 | 17 |
| 10 | Botox | M | 3.5 | C5-C6 | TT and MQ | 12 | 20 |
| 11 | Botox | M | 4.3 | Total | TT and MQ | 12 | 18 |
| 12 | Neurolysis | F | 2.0 | C5-C6 | TT and MQ | 11 | 17 |
| 13 | Capsule release | F | 8.5 | Total | TT and MQ | 13 | 19 |
| 14 | Tendon transfer, neurolysis | M | 4.3 | C5-C8 | TT and MQ | 14 | 20 |
| 15 | Neurolysis and botox | F | 5.0 | C5-C6 | TT | 13 | 20 |
| 16 | Muscle transfer | M | 7.9 | C5-C7 | TT | 14 | 21 |
| 17 | BP exploration | M | 2.0 | C5-C6 | TT and MQ | 15 | 20 |
| 18 | Steindler flexorplasty | F | 10.0 | C5-C7 | TT and MQ | 13 | 18 |
| 19 | Humeral osteotomy | M | 14.0 | C5-C6 | MQ | 12 | 18 |
| 20 | Tendon transfer | F | 3.0 | C5-C7 | MQ | 14 | 20 |
| Mean ± STD | 6.5 | 12 ± 1.5 | 18 ± 2.3 | ||||
| P value | < 0.0001 |
| Patients | Other surgeons and previous surgeries | PreTT-PHHA | PostTT-PHHA | PreTT-Version | PostTT-Version | PreTT-SHEAR | PostTT-SHEAR |
| 1 | Subscap release and lat dorsi rerouting | 8 | 33 | -47 | -14 | ||
| 2 | Neurolysis, MQ, HO | 16 | 14 | -41 | -35 | 24 | 10 |
| 3 | MQ | -12 | 19 | -65 | -33 | 40 | 39 |
| 4 | Nerve graft, FO, BTL, MQ | 32 | 37 | -21 | -10 | 3 | 1 |
| 5 | Botox, MQ | 33 | 45 | -18 | -15 | 15 | 3 |
| 6 | Nerve graft | 47 | 48 | -10 | -1 | 5 | 14 |
| 7 | Neurolysis, nerve graft | -7 | 22 | -62 | -12 | 8 | 22 |
| 8 | Neuroma excision, nerve graft | 34 | 35 | -20 | -11 | 0 | 0 |
| 9 | Nerve transfer | 33 | 29 | -16 | -21 | 15 | 12 |
| 10 | Coracoacromial release/resection | -12 | 17 | -51 | -35 | 30 | 15 |
| 11 | Neurolysis, nerve graft | 13 | 4 | -20 | -15 | 7 | 4 |
| 12 | Wrist Caps, HO | 39 | 50 | 0 | 0 | 9 | 0 |
| 13 | Sural nerve graft | 38 | 51 | -10 | -4 | 0 | 1 |
| 14 | Botox, MQ | -8 | 44 | -38 | -22 | 11 | 2 |
| 15 | Neurolysis, MQ | -14 | 35 | -33 | -10 | 25 | 30 |
| 16 | Muscle release | 0 | 19 | -45 | -27 | 32 | 8 |
| 17 | Anterior capsule release | -11 | 34 | -53 | -22 | 48 | 41 |
| 18 | Tendon transfer and neurolysis | 33 | 39 | -18 | -7 | 1 | 1 |
| Mean | 14.6 ± | 31.9 ± | -31.6 ± | -16.3 ± | 16.1 ± | 11.9 ± | |
| STD | 21.7 | 13.6 | 19.3 | 11.0 | 14.7 | 13.5 | |
| P value | 0.001 | 0.0002 | 0.087 |
The nerve involvement was C5-6 (n = 5), C5-7 (n = 8), and total (n = 7). Traditional operative procedures that these OBPP children had in the past at other clinics are nerve transfer/graft, neurolysis, brachial plexus exploration, botox, muscle/tendon transfer and release, humeral osteotomy and anterior capsule release. Outcomes of our revision procedures in OBPP patients were compared to the results of other traditional surgical treatments at other clinics. Further, these patients’ radiological scores were measured from computed tomography and magnetic resonance images and statistically compared.
We examined physically all OBPP children and their video recordings pre- and post-operatively, scoring their modified Mallet parameters on a scale between one and five. One and five denote lack of movement and normal function respectively.
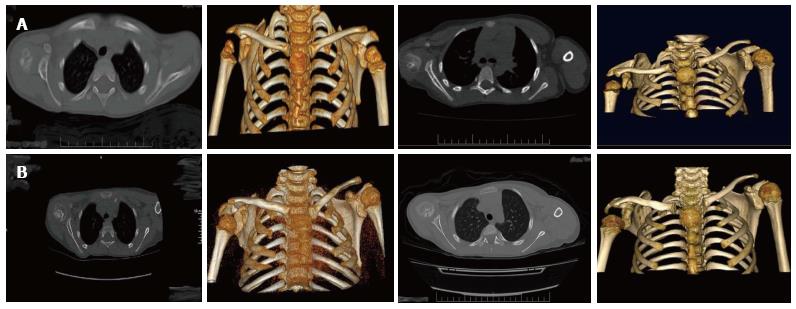
Pre-revision surgery mean modified Mallet score was 12.0 ± 1.5 (Table 1 and Figure 1 upper panels). This functional score was greatly improved to 18 ± 2.3 (P < 0.0001) at least one-year after our revision surgeries (Table 1, Figure 1 lower panels). Furthermore, their shoulder anatomical scores were improved significantly to 31.9 ± 13.6 (P < 0.001) and -16.3 ± 11 (P < 0.0002) at least one-year after triangle tilt operation (Table 2 and Figure 2, lower panels). This was in comparison to their radiological outcomes of other procedures before having triangle tilt with us (mean PHHA, glenoid version and SHEAR were 14.6 ± 21.7, -31.6 ± 19.3 and 16.1 ± 14.7 respectively; Table 2 and Figure 2 upper panels).
Twenty OBPP children in our present study had one or multiple operative procedures at other clinics before visiting our institute for further treatments (Table 1). One patient in our study group had Steindler flexoroplasty, which improves active flexion of the elbow. These conventional treatments fail to address the SHEAR deformity[30] associated with majority of OBPP patients. Therefore, these OBPP patients in our study had persistent shoulder contractures and joint incongruency. Hence, they also had poor upper extremity functions. (Tables 1 and 2; upper panels in Figures 1 and 2).
Mod Quad procedure addresses poor shoulder abduction in permanent OBPP. However, this procedure is ineffective to correct the glenohumeral joint and SHEAR deformities. Eighteen OBPP children, who had shoulder joint incongruency and SHEAR undergone TT bony operation with us. We demonstrated that this procedure effectively addressed the bony deformities of the affected upper extremity and improved it’s anatomy and functions[20-28]. After undergone these two revision surgical procedures with us, these twenty patients had better results both functionally and anatomically. This is highly significant in comparison to the outcomes of other surgical treatments at other clinics.
There was statistically significant improvement anatomically, after having triangle tilt compared to the radiological outcomes of other operative procedures.
In conclusion, we demonstrate here that mod Quad and triangle tilt as successful revision surgical procedures in 20 OBPP patients, who had conventional surgical therapies at other clinics before presenting to us for further treatment.
Many traditional surgical interventions such as posterior glenohumeral capsulorrhaphy, biceps tendon lengthening, humeral osteotomy, anterior capsule release, nerve transfer/graft, botox, muscle and or tendon transfer and release have been reported to improve upper limb functions in obstetric brachial plexus palsy (OBPP) patients.
The authors compared functional and anatomical improvements from the revision surgical treatment experiences to results of other traditional surgeries at other clinics in 20 children with OBPP.
Pre-revision surgery mean mod Mallet scores and radiological scores such as posterior subluxation and glenoid version were improved statistically highly significantly at least one-year after mod Quad and or triangle tilt revision surgeries.
The authors demonstrate here, the triangle tilt and mod Quad as successful revision surgeries in OBPP patients, who had other surgical treatments at other clinics.
SHEAR: Scapular Hypoplasia, Elevation and Rotation; Triangle tilt surgery: This surgical procedure includes osteotomies of the clavicle, neck of the acromion and scapula in order to release the distal acromioclavicular triangle and allow it to reorient itself in a more neutral position into the glenoid.
This is an informative paper, generally well-written and of interest to readers.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Franklyn M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Birch R. Late sequelae at the shoulder in obstetrical palsy in children. Surgical techniques in orthopaedics and traumatology: Shoulder. Volume 3. Surgical Techniques in Orthopaedics and Traumatology. Paris: Elsevier 2001; 55-200-E-210. [Cited in This Article: ] |
| 2. | Kon DS, Darakjian AB, Pearl ML, Kosco AE. Glenohumeral deformity in children with internal rotation contractures secondary to brachial plexus birth palsy: intraoperative arthrographic classification. Radiology. 2004;231:791-795. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | van der Sluijs JA, van Ouwerkerk WJ, de Gast A, Wuisman PI, Nollet F, Manoliu RA. Deformities of the shoulder in infants younger than 12 months with an obstetric lesion of the brachial plexus. J Bone Joint Surg Br. 2001;83:551-555. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Waters PM. Obstetric Brachial Plexus Injuries: Evaluation and Management. J Am Acad Orthop Surg. 1997;5:205-214. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Birch R, Bonney G, Wynn Parry CB: Birth lesions of the brachial plexus. Surgical disorders of the peripheral nerves. In: Birch R, Bonney G, Wynn Parry CB, editors. New York, NY: Churchill Livingstone 1998; 209-233. [Cited in This Article: ] |
| 6. | Shenaq SM, Kim JY, Armenta AH, Nath RK, Cheng E, Jedrysiak A. The Surgical Treatment of Obstetric Brachial Plexus Palsy. Plast Reconstr Surg. 2004;113:54E-67E. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Nath RK, Somasundaram C, Mahmooduddin F. Comparing functional outcome of triangle tilt surgery performed before versus after two years of age. Open Orthop J. 2011;5:59-62. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Hoffer MM, Phipps GJ. Closed reduction and tendon transfer for treatment of dislocation of the glenohumeral joint secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 1998;80:997-1001. [PubMed] [Cited in This Article: ] |
| 9. | Pearl ML, Edgerton BW, Kon DS, Darakjian AB, Kosco AE, Kazimiroff PB, Burchette RJ. Comparison of arthroscopic findings with magnetic resonance imaging and arthrography in children with glenohumeral deformities secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 2003;85-A:890-898. [PubMed] [Cited in This Article: ] |
| 10. | Pedowitz DI, Gibson B, Williams GR, Kozin SH. Arthroscopic treatment of posterior glenohumeral joint subluxation resulting from brachial plexus birth palsy. J Shoulder Elbow Surg. 2007;16:6-13. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Kambhampati SB, Birch R, Cobiella C, Chen L. Posterior subluxation and dislocation of the shoulder in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2006;88:213-219. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Al-Qattan MM. Latissimus dorsi transfer for external rotation weakness of the shoulder in obstetric brachial plexus palsy. J Hand Surg Br. 2003;28:487-490. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | El-Gammal TA, Saleh WR, El-Sayed A, Kotb MM, Imam HM, Fathi NA. Tendon transfer around the shoulder in obstetric brachial plexus paralysis: clinical and computed tomographic study. J Pediatr Orthop. 2006;26:641-646. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Nath RK, Paizi M. Improvement in abduction of the shoulder after reconstructive soft-tissue procedures in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2007;89:620-626. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Pagnotta A, Haerle M, Gilbert A. Long-term results on abduction and external rotation of the shoulder after latissimus dorsi transfer for sequelae of obstetric palsy. Clin Orthop Relat Res. 2004;199-205. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Safoury Y. Muscle transfer for shoulder reconstruction in obstetrical brachial plexus lesions. Handchir Mikrochir Plast Chir. 2005;37:332-336. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | van der Sluijs JA, van Ouwerkerk WJ, de Gast A, Nollet F, Winters H, Wuisman PI. Treatment of internal rotation contracture of the shoulder in obstetric brachial plexus lesions by subscapular tendon lengthening and open reduction: early results and complications. J Pediatr Orthop B. 2004;13:218-224. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Waters PM, Bae DS. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J Bone Joint Surg Am. 2006;88:1035-1042. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Waters PM, Bae DS. Effect of tendon transfers and extra-articular soft-tissue balancing on glenohumeral development in brachial plexus birth palsy. J Bone Joint Surg Am. 2005;87:320-325. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Nath RK, Amrani A, Melcher SE, Eichhorn MG. Triangle tilt surgery in an older pediatric patient with obstetric brachial plexus injury. Eplasty. 2009;9:e26. [PubMed] [Cited in This Article: ] |
| 21. | Nath RK, Amrani A, Melcher SE, Wentz MJ, Paizi M. Surgical normalization of the shoulder joint in obstetric brachial plexus injury. Ann Plast Surg. 2010;65:411-417. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Nath RK, Avila MB, Karicherla P. Triangle tilt surgery as salvage procedure for failed shoulder surgery in obstetric brachial plexus injury. Pediatr Surg Int. 2010;26:913-918. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Nath RK, Liu X, Melcher SE, Fan J. Long-term outcomes of triangle tilt surgery for obstetric brachial plexus injury. Pediatr Surg Int. 2010;26:393-399. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Nath RK, Mahmooduddin F. Triangle tilt surgery: effect on coracohumeral distance and external rotation of the glenohumeral joint. Eplasty. 2010;10:e67. [PubMed] [Cited in This Article: ] |
| 25. | Nath RK, Lyons AB, Melcher SE, Paizi M. Surgical correction of the medial rotation contracture in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2007;89:1638-1644. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Nath RK, Melcher SE, Paizi M. Surgical correction of unsuccessful derotational humeral osteotomy in obstetric brachial plexus palsy: evidence of the significance of scapular deformity in the pathophysiology of the medial rotation contracture. J Brachial Plex Peripher Nerve Inj. 2006;1:9. [PubMed] [DOI] [Cited in This Article: ] |
| 27. | Nath RK, Somasundaram C, Mahmooduddin F. Triangle tilt and steel osteotomy: similar approaches to common problems. Open Orthop J. 2011;5:124-133. [PubMed] [DOI] [Cited in This Article: ] |
| 28. | Nath RK, Somasundaram C, Melcher SE, Bala M, Wentz MJ. Arm rotated medially with supination - the ARMS variant: description of its surgical correction. BMC Musculoskelet Disord. 2009;10:32. [PubMed] [DOI] [Cited in This Article: ] |
| 29. | Friedman RJ, Hawthorne KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992;74:1032-1037. [PubMed] [Cited in This Article: ] |
| 30. | Nath RK, Paizi M. Scapular deformity in obstetric brachial plexus palsy: a new finding. Surg Radiol Anat. 2007;29:133-140. [PubMed] [DOI] [Cited in This Article: ] |
| 31. | Nath RK, Somasundaram C. Successful outcome of modified quad surgical procedure in preteen and teen patients with brachial plexus birth palsy. Eplasty. 2012;12:e54. [PubMed] [Cited in This Article: ] |
| 32. | Nath RK, Kumar N, Somasundaram C. Modified Quad surgery significantly improves the median nerve conduction and functional outcomes in obstetric brachial plexus nerve injury. Ann Surg Innov Res. 2013;7:5. [PubMed] [DOI] [Cited in This Article: ] |