Published online Sep 18, 2015. doi: 10.5312/wjo.v6.i8.636
Peer-review started: April 24, 2015
First decision: May 13, 2015
Revised: June 16, 2015
Accepted: July 11, 2015
Article in press: July 14, 2015
Published online: September 18, 2015
Processing time: 147 Days and 8.4 Hours
AIM: To present the results of total hip arthroplasty (THA) for post tubercular arthritis of the hip joint.
METHODS: Sixty-five patients (45 male, 20 female) with previously treated tuberculosis of the hip joint underwent cementless THA for post tubercular arthritis. The average age at the time of THA was 48 years (range 29 to 65 years). Erythrocyte sedimentation rate, C reactive protein, chest X-ray and contrast enhanced magnetic resonance imaging were done preoperatively to confirm resolution of the disease and to rule out any residual disease. Intra-operative samples were taken for microbiological examination, polymerase chain reaction (PCR) and histological examination. Patients were started on anti-tubercular drugs one week before the operation and continued for 6 mo post operatively. The patients were followed up clinically using the Harris hip score as well as radiologically for any loosening of the implants, osteolysis and any recurrence of tuberculosis. Any complications especially the recurrence of the infection was also recorded.
RESULTS: The mean interval from completion of antitubercular therapy for tuberculosis to surgery was 4.2 years (range, 2-6 years). Preoperatively, 17 patients had ankylosis whereas 48 patients had functional but painful range of motion. The mean surgical time was 97 min (range, 65-125) whereas the mean blood loss was 600 mL (range, 400-900 mL). The average follow up was 8.3 years (range 6-11 years). The average Harris Hip score improved from 27 preoperatively to 91 at the final follow up. Seventeen patients had acetabular protrusion which was managed with impaction grafting and cementless acetabular cup. The bone graft had consolidated in all these 17 patients at the follow up. Two patients developed discharging sinuses at 9 and 11 mo postoperatively respectively. The discharge tested positive for tuberculosis on the PCR. Both these patients were put on antitubercular therapy for another year. Both of them recovered and had no evidence of any loosening or osteolysis on X-rays. There were no other complications recorded.
CONCLUSION: Total hip replacement restores good function to patients suffering from post tubercular arthritis of the hip.
Core tip: Total hip replacement restores good function to patients suffering from post tubercular arthritis of the hip. A good preoperative work up to rule out any residual disease as well as perioperative chemotherapy are recommended to ensure success. Any recurrence of the disease can be managed by chemotherapy.
- Citation: Kumar V, Garg B, Malhotra R. Total hip replacement for arthritis following tuberculosis of hip. World J Orthop 2015; 6(8): 636-640
- URL: https://www.wjgnet.com/2218-5836/full/v6/i8/636.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i8.636
Tuberculosis of the hip accounts for a significant proportion of cases of osteo-articular tuberculosis, being next to only tuberculosis of spine[1]. Tuberculosis of hip constitutes 10%-15% of all patients with osteoarticular tuberculosis[1,2]. The patients in developing countries usually present late with advanced joint destruction as a result of the disease. Moreover, many of these patients are young and have several decades of active life ahead of them once the infection has healed with destruction of the affected hip joint. The surgical options for such patients suffering from arthritis of hip due to tuberculosis include excision arthroplasty, arthrodesis, and, total hip replacement. Excision arthroplasty results in an unstable joint with shortening and an abnormal gait[3,4]. An arthrodesis produces a stable painless immobile joint with poor function and is often associated with non union, pain in the adjacent joints and a slow abnormal gait[5]. Total hip arthroplasty (THA) provides a painless stable joint with a normal gait. Although THA has been recommended in patients with post tubercular arthritis[6-10], recurrence of the disease[11-13], fear of high complication rates and the long term survival of the reconstruction remain major concerns. THA, nonetheless, still is reported to be associated with a good outcome in these patients[6-10].
The aim of this study is to present the results of THA done at our center for post tubercular arthritis or ankylosis of hip joint.
This study was performed at the All India Institute of Medical Sciences, New Delhi. We retrospectively reviewed 65 patients who underwent a total hip replacement for advanced arthritis of the hip due to tuberculosis following treatment. The Institute Ethics committee approved this study. All patients who had arthritis following tuberculosis of hip were included in the study. All patients had successfully completed full course of 18 mo of Anti tubercular drugs previously with documented complete resolution of the disease. The patients who had clinical and/radiological evidence of tuberculosis and those who had not completed the full course of anti tubercular therapy were excluded from the study. Erythrocyte sedimentation rate (ESR), C reactive protein (CRP), chest X-ray and contrast enhanced magnetic resonance imaging (MRI) were done to confirm resolution of the disease and to rule out any residual disease.
All patients were given Antitubercular drugs (Isoniazid, Pyrazinamide, Ethambutol and Rifampicin) starting one week before until 2 mo following surgery. At 2 mo following the hip replacement, Ethambutol and Pyrazinamide were stopped and Isoniazid and Rifamipicin continued for another 4 mo.
All patients were operated under Spinal or General Anesthesia using the posterior approach in lateral decubitus position. Intravenous 1 g cefazolin was used as antibiotic prophylaxis for 5 d. A Cementless Total hip Replacement was performed in all the patients. The tissue and fluid samples obtained at the time of surgery were sent for Gram staining, acid fast bacilli staining, polymerase chain reaction (PCR), culture and sensitivity for mycobacteria and histopathological examination.
Low molecular weight heparin and compression stockings were used for antithrombotic prophylaxis in all the patients.
A retrospective review of all the case records was done. The data was collected from hospital records and follow up records All the patients are routinely assessed at two weeks, one, three, six and twelve months postoperatively and yearly thereafter. The patients were evaluated clinically using the Harris Hip Score[14] and radiologically for bone ingrowth, stability and fixation using the stability - fixation score[15]. The radiographs were also scrutinized for any evidence of loosening or osteolysis in the 7 Gruen zones[16] around the femoral component and 3 zones around the acetabulum as described by DeLee and Charnley[17]. Any complications especially the recurrence of the infection were recorded.
There were 45 male and 20 female patients. The average age at the time of successful hip replacement was 48 years (29-65 years). Forty-three patients were less than 45 years of age at the time of hip replacement. Twenty-nine patients had right hip involved whereas 36 patients had involvement of the left hip joint.
The implants used were Versys-Trilogy (Zimmer) in 33 patients, Corail -Duraloc (Depuy, Johnson and Johnson) in 27 patients and S ROM -Pinnacle cup (Depuy, Johnson and Johnson) in 5 patients.
Preoperatively, none of the patients had any evidence of residual disease on contrast enhanced MRI. The ESR and CRP were within normal limits in all the patients. On examination of the tissue samples obtained during surgery, no patient had positive tissue culture or histopathological evidence of tuberculosis.
The mean interval from completion of antitubercular therapy for tuberculosis to surgery was 4.2 years (range, 2-6 years). Preoperatively, 17 patients had ankylosis whereas 48 patients had functional but painful range of motion. The preoperative mean limb length discrepancy was 3.8 cm (range 3-5.5 cm).
The mean surgical time was 97 min (range, 65-125) whereas the mean blood loss was 600 mL (range, 400-900 mL).
The average follow up was 8.3 years (range 6-11 years). A fibrous ankylosis was seen in 17 hips. The acetabular defects were classified according to Paprosky classification[18]. There were 17 hips with type I defect, 8 hips with Type IIa defect, and 4 hips with type IIb defects. No major defects were seen on the femoral side. There was a difficulty in dislocating the hip and an in-situ osteotomy of the femoral neck was done in 10 cases that presented with ankylosis of the hip joint.
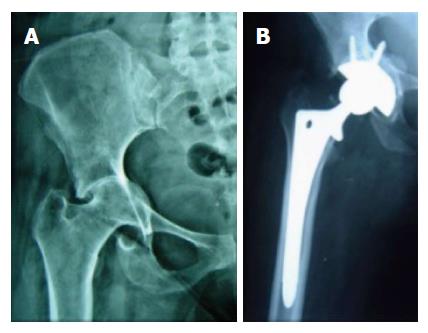
Twenty-five patients had acetabular protrusion (Type I and II Paprosky defect) for which impaction grafting from the femoral head was done was done (Figure 1). The bone grafts consolidated in all the patients at 3 mo. The mean Harris Hip Score improved from 27 (range, 20-36) to 91 (range, 88-94) at the latest follow up. The improvement in Harris Score was similar in both males and females.
All femoral stems had evidence of osteointegration at 1 year and were stable at the latest follow up with no signs of osteolysis or loosening. No patient had any evidence of osteolysis or loosening on the acetabular side.
There was no dislocation or heterotopic bone formation.
There were 2 patients who developed a discharging sinus at 9 and 11 mo postoperatively respectively. The discharge was positive for tuberculosis on PCR. Both these patients were treated with 4-drug chemotherapy for another one year. Both of them recovered and had no evidence of any loosening or osteolysis on X-rays at the latest follow up of 6.2 and 6.5 years respectively.
The patients with tuberculosis of the hip joint often have advanced arthritis with severe deformities and limb length discrepancy. Total hip replacement has been used successfully for the treatment of post tubercular arthritis[6,8,12,19-21]. One of the major concerns is the risk of reactivation of cured or quiescent disease following surgery[8,11-13,22,23].
As tubercular bacilli do not adhere to metal surface and have little or no biofilm formation[24-26], spinal instrumentation has been used successfully in the treatment of active tuberculosis of spine[27]. The early results of Total hip replacement in active tuberculosis are encouraging[10,26,28]. Tuberculosis is a chronic disease and reactivation of disease occurs in 2%-5% of patients as late as 20 years after apparent healing[29]. Systemic Corticosteroid therapy, Malnutrition, diabetes, surgical procedure or injury to previously infected area may cause the dormant bacilli persisting in tissue to start multiplying resulting in reactivation[29]. It has also been observed that the risk of reactivation is more in patients who either had an overlooked tubercular lesion, were on long term steroid treatment, were not given chemotherapy or were non compliant with antitubercular treatment (ATT), had chronic discharging tract, and, in those with positive tissue culture during surgery[8-10,21,26,28].
In patients undergoing THA for tubercular arthritis, the recommended periods of quiescence before THR varies from immediate to 10 years[6,8,9,12,19,20,26,28]. However reactivation has been reported even in cases operated even after a quiescent period of 37-40 years[22]. Hence as a part of preoperative assessment, only patients who had completed full course of antitubercular therapy were considered for THA in the current series. Moreover, any residual disease was ruled out on MRI. In order to prevent any reactivation of disease due to the immune suppression which occurs at the time of surgery, it is recommended to start ATT preoperatively and continue ATT post operatively for 3-6 mo[19-21]. The benefits of ATT in such cases outweigh its possible side effects. In spite of careful patient selection and ATT, there was recurrence in form of a discharging sinus in 2 patients in the current series. It implies that the complete resolution of disease on imaging and limited perioperative chemotherapy for the infection does not guarantee recurrence free follow up. However, we did not see any recurrence after one year of surgery in the current series.
The gold standard for the diagnosis of tuberculosis is the presence of caseating or non-caseating granulomas with or without positive smears or cultures for Acid fast bacilli on histopathological examination of biopsy specimens from synovial tissues[8,30,31]. The histopathological examination of operative specimens in this study did not yield any evidence of tuberculosis, even in the two cases who had recurrence of infection. It is possible that the specimens taken from the femur, acetabulum and capsule were not extensive enough to pick up the dormant bacilli in the joint. Kim et al[8] in their series of THA done for tuberculosis hip had negative histopathological findings in 3 cases at the time of operation which later on developed recurrence. It can be concluded that the negative findings on the intraoperative histopathological specimens and cultures do not necessarily prove the absence of tuberculous infection.
Both the patients who experienced recurrence of the tubercular infection were managed with antitubercular drugs for one year, which led to the complete healing. It has been seen that the tubercular sinuses and ulcers heal within 6-12 wk of systemic antitubercular chemotherapy[29]. Only less than 1% of patients with sinuses require debridement and complete excision of sinuses is often not possible as the sinus ramification is often greater than what is apparent[29].
The treatment of reactivation remains controversial. Johnson et al[22] recommended the removal of the prosthesis for control of reactivation whereas McCullough[13] treated recurrent draining sinus with chemotherapy alone without the removal of prosthesis. Kim et al[8] also treated 6 cases of recurrence in their series with chemotherapy alone in 5 patients and debridement with chemotherapy in one case. They did not have to remove the prosthesis to control the disease. Hence reactivation of disease can be managed with retention of prosthesis with chemotherapy alone as was also done in this series or in combination with debridement as reported in literature.
Both cemented and cementless implants have been used successfully for patients with post-tubercular arthritis. The reactivation rates for both cemented and Cementless THRs in patients with quiescent tuberculosis are similar[8,10] thereby indicating that ostensible mycobactericidal action of thermal reaction from cement is not relevant to reactivation[8,26].
We have seen in that patients with post tubercular arthritis often have destroyed femoral heads but no major defects in the femur. The femoral reconstruction therefore is straightforward. However, there are defects on the acetabular side ranging from segmental to protrusion defects. The presence of these defects on the acetabular side often necessitates the use of a cementless shell along with bone graft. The current series affirms the success of this technique for post tubercular arthritis.
The patients suffering from tuberculosis of hip are young. These patients present with hip arthritis at a relatively young age and therefore a cementless hip replacement is a good option. The current series confirms the mid term survival of cementless implants in this cohort as there were no failures due to the osteolysis at an average follow up of 8.3 years. We conclude that cementless hip replacement can be used successfully for patients with post tubercular arthritis of hip.
The limitations to this study are its retrospective nature, a relatively short follow up considering young patient cohort and heterogeneity of the implants used. Also in view of the recurrence of infection in 2 patients, we are unable to endorse the current recommended regime and duration of recommended perioperative chemotherapy.
To conclude, total hip replacement under ATT cover restores good function to the patients suffering from tuberculosis provided a good preoperative work up is done to rule out any residual disease and postoperatively patients are followed up for any recurrence. A recurrence is possible especially during the first year after surgery despite complete radiological resolution and perioperative antitubercular chemotherapy but is amenable to treatment with chemotherapy.
Tuberculosis of hip often results in arthritis of hip joint warranting a total hip replacement. This study aims to present the results of total hip replacement in patients suffering from hip arthritis as a result of tuberculosis of hip.
The patients suffering from post tubercular arthritis in developing countries are usually young. Total hip replacement in patients with post tubercular arthritis has concerns of recurrence of the disease, fear of high complication rates and the long term survival of the reconstruction.
In this study, cementless total hip replacement restored good function in patients suffering from post tubercular arthritis of hip. A recurrence of disease in form of discharging sinus seen in 2 patients was successfully managed with antitubercular therapy with no surgical intervention.
Cementless total hip replacement done under cover of antitubercular therapy is a safe and durable treatment option for patients suffering from post tubercular arthritis of hip.
This clinical paper analyses the patient response data to tuberculosis of the hip and varying therapies applied. The paper content is a novel comparison of data to a niche area that will be of interest.
P- Reviewer: Cartmell S, Mashreky SR S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res. 2002;93-99. [PubMed] [Cited in This Article: ] |
| 2. | Tuli SM. Tuberculosis of the Skeletal System: Bones, Joints, Spine and Bursal Sheaths. Jaypee Brothers Publishers, 2004. . [Cited in This Article: ] |
| 3. | Clegg J. The results of the pseudarthrosis after removal of an infected total hip prosthesis. J Bone Joint Surg Br. 1977;59:298-301. [PubMed] [Cited in This Article: ] |
| 4. | Tuli SM, Mukherjee SK. Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg Br. 1981;63-B:29-32. [PubMed] [Cited in This Article: ] |
| 5. | Lipscomb PR, McCaslin FE. Arthrodesis of the Hip. J Bone Jt Surg. 1961;43:923-979. [Cited in This Article: ] |
| 6. | Dogra AS, Kulkarni SS, Bhosale PB. Total hip arthroplasty in healed tuberculous hip. J Postgrad Med. 1995;41:114-116. [PubMed] [Cited in This Article: ] |
| 7. | Su JY, Huang TL, Lin SY. Total knee arthroplasty in tuberculous arthritis. Clin Orthop Relat Res. 1996;181-187. [PubMed] [Cited in This Article: ] |
| 8. | Kim YH, Han DY, Park BM. Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am. 1987;69:718-727. [PubMed] [Cited in This Article: ] |
| 9. | Yoon TR, Rowe SM, Anwar IB, Chung JY. Active tuberculosis of the hip treated with early total hip replacement--a report of 3 cases. Acta Orthop Scand. 2001;72:419-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Yoon TR, Rowe SM, Santosa SB, Jung ST, Seon JK. Immediate cementless total hip arthroplasty for the treatment of active tuberculosis. J Arthroplasty. 2005;20:923-926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Hugate R, Pellegrini VD. Reactivation of ancient tuberculous arthritis of the hip following total hip arthroplasty: a case report. J Bone Joint Surg Am. 2002;84-A:101-105. [PubMed] [Cited in This Article: ] |
| 12. | Hardinge K, Cleary J, Charnley J. Low-friction arthroplasty for healed septic and tuberculous arthritis. J Bone Joint Surg Br. 1979;61-B:144-147. [PubMed] [Cited in This Article: ] |
| 13. | McCullough CJ. Tuberculosis as a late complication of total hip replacement. Acta Orthop Scand. 1977;48:508-510. [PubMed] [Cited in This Article: ] |
| 14. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] [Cited in This Article: ] |
| 15. | Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;107-128. [PubMed] [Cited in This Article: ] |
| 16. | Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;17-27. [PubMed] [Cited in This Article: ] |
| 17. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;20-32. [PubMed] [Cited in This Article: ] |
| 18. | Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33-44. [PubMed] [Cited in This Article: ] |
| 19. | Santavirta S, Eskola A, Konttinen YT, Tallroth K, Lindholm ST. Total hip replacement in old tuberculosis. A report of 14 cases. Acta Orthop Scand. 1988;59:391-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Eskola A, Santavirta S, Konttinen YT, Tallroth K, Hoikka V, Lindholm ST. Cementless total replacement for old tuberculosis of the hip. J Bone Joint Surg Br. 1988;70:603-606. [PubMed] [Cited in This Article: ] |
| 21. | Kim YY, Ahn JY, Sung YB, Ko CU, Shim JC, Park HS, Bai GH. Long-term results of Charnley low-friction arthroplasty in tuberculosis of the hip. J Arthroplasty. 2001;16:106-110. [PubMed] [Cited in This Article: ] |
| 22. | Johnson R, Barnes KL, Owen R. Reactivation of tuberculosis after total hip replacement. J Bone Joint Surg Br. 1979;61-B:148-150. [PubMed] [Cited in This Article: ] |
| 23. | Hecht RH, Meyers MH, Thornhill-Joynes M, Montgomerie JZ. Reactivation of tuberculous infection following total joint replacement. A case report. J Bone Joint Surg Am. 1983;65:1015-1016. [PubMed] [Cited in This Article: ] |
| 24. | Ha KY, Chung YG, Ryoo SJ. Adherence and biofilm formation of Staphylococcus epidermidis and Mycobacterium tuberculosis on various spinal implants. Spine (Phila Pa 1976). 2005;30:38-43. [PubMed] [Cited in This Article: ] |
| 25. | Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358:135-138. [PubMed] [Cited in This Article: ] |
| 26. | Neogi DS, Yadav CS, Ashok Kumar SA, Rastogi S. Total hip arthroplasty in patients with active tuberculosis of the hip with advanced arthritis. Clin Orthop Relat Res. 2010;468:605-612. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine (Phila Pa 1976). 1993;18:1890-1894. [PubMed] [Cited in This Article: ] |
| 28. | Sidhu AS, Singh AP, Singh AP. Total hip replacement in active advanced tuberculous arthritis. J Bone Joint Surg Br. 2009;91:1301-1304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;11-19. [PubMed] [Cited in This Article: ] |
| 30. | Holmdahl HC. Tuberculosis of the knee; a review of 170 cases. Acta Orthop Scand. 1950;20:19-49. [PubMed] [Cited in This Article: ] |