Published online Mar 18, 2022. doi: 10.5312/wjo.v13.i3.267
Peer-review started: April 26, 2021
First decision: July 28, 2021
Revised: August 7, 2021
Accepted: February 9, 2022
Article in press: February 9, 2022
Published online: March 18, 2022
Intertrochanteric (IT) fracture is one of the most common fractures seen in an orthopaedic practice. Proximal femoral nailing (PFN) is a common modality of fixing IT femur fracture. We retrospectively studied whether a PFN with two proximal lag screws can be done without distal interlocking screws in the 31-A1 and 31-A2 fracture patterns according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) guidelines for IT femur fractures.
To compare the outcomes of IT fractures (AO/OTA 31-A1 and 31-A2) treated by PFN with and without distal interlocking screws.
We carried out a retrospective study of 140 patients in a tertiary care centre who had AO/OTA type 31-A1 and 31-A2 IT fractures. We divided the patients into two groups, in which one of the groups received distal interlocking screws (group 1) and the other group did not (group 2). The subjects were followed up for a mean period of 14 mo and assessed for radiological union time, fracture site collapse, mechanical stability of implant, and complications associated with the PFN with distal interlocking and without distal interlocking. Then, the results were compared.
PFN without distal interlocking screws has several advantages and gives better results over PFN with distal interlocking screws in the AO/OTA 31-A2 fracture pattern. However, similar results were observed in both groups with the fracture pattern AO/OTA 31-A1. In patients with fracture pattern AO/OTA 31-A2 treated by PFN without distal interlocking screws, there were minimal proximal lock-related complications and no risk of distal interlock-related complications. The operative time, IITV radiation time and time to radiological union were reduced. These patients also had better rotational alignment of the proximal femur, and the anatomy of the proximal femur was well maintained. It was also noted that in the cases where distal interlocking was performed, there was a gradual decrease in neck shaft angle, which led to varus collapse and failure of bone-implant construct in 21.40%.
In fracture pattern AO/OTA 31-A2, PFN without distal interlocking had better results and less complications than PFN with distal interlocking.
Core Tip: There are few studies comparing clinical and radiological results of proximal femoral nail (PFN) with and without distal interlocking in fracture pattern 31-A1 and 31-A2 according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association guidelines. From this retrospective study, we conclude that in type 31-A1 intertrochanteric fractures use of long anatomical PFN with or without distal interlocking screws have similar results in terms of radiological union, postoperative proximal femur anatomy, and rotational alignment. In type 31-A2, the use of long anatomical PFN without distal interlocking screws gives better results and less proximal lock-related complications than PFN with distal interlocking screws.
- Citation: Lil NA, Makwana VR, Patel TD, Patel AR. Comparative study of intertrochanteric fracture fixation using proximal femoral nail with and without distal interlocking screws. World J Orthop 2022; 13(3): 267-277
- URL: https://www.wjgnet.com/2218-5836/full/v13/i3/267.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i3.267
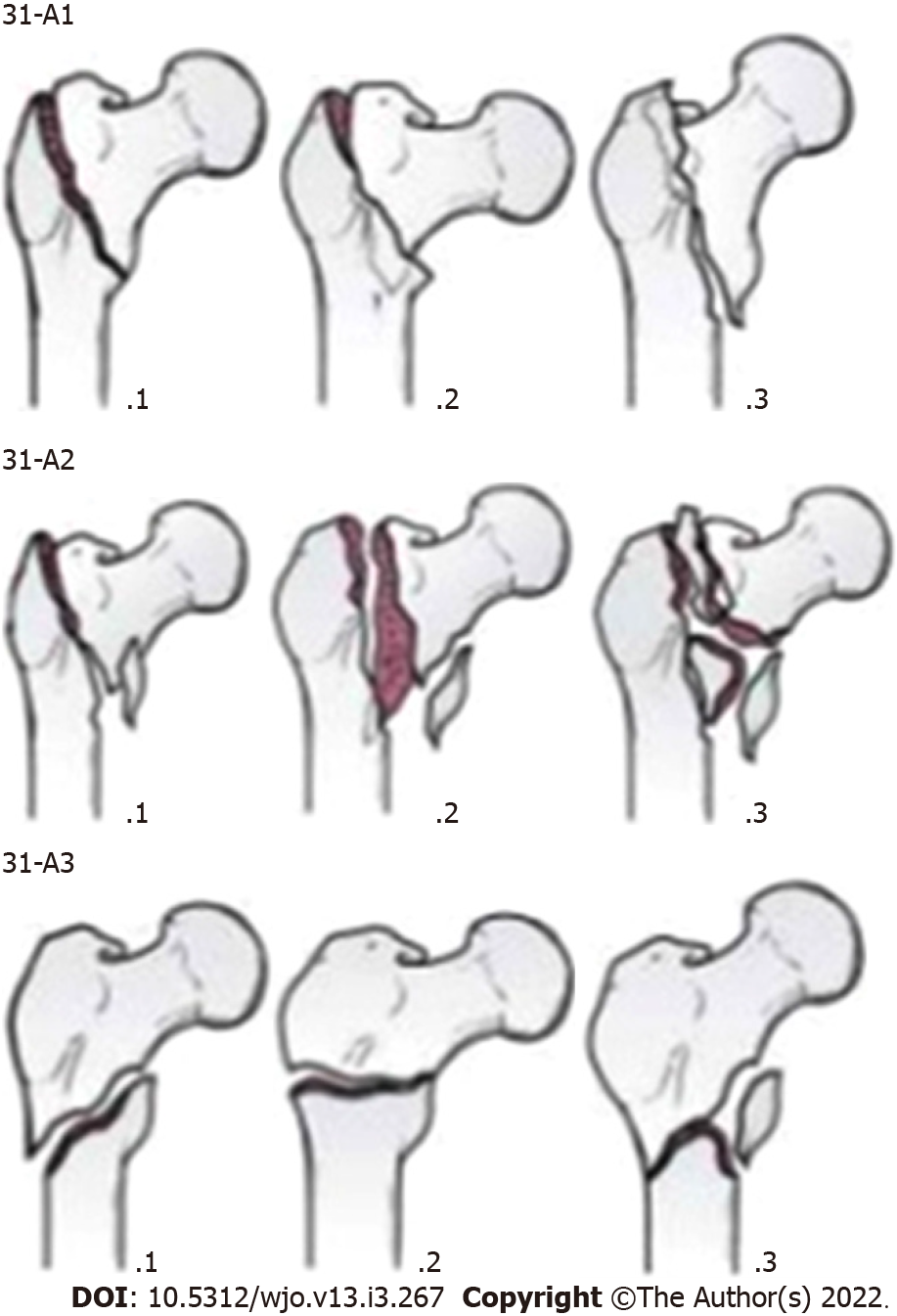
The incidence of fractures in the trochanteric area has risen with the increasing numbers of elderly persons with osteoporosis[1]. Intertrochanteric (IT) fracture is one of the most common fractures seen in orthopaedic practices, and proximal femoral nailing (PFN) has become a popular modality for its treatment. As per the Orthopaedic Trauma Association (OTA) classification system, these fractures are classified as Arbeitsgemeinschaft für Osteosynthesefragen (AO)/OTA 31-A and are further subdivided into groups A1, A2 and A3 (Figure 1). A1 fractures consist of two-part fractures, A2 fractures have multiple fragments, and A3 fractures include reverse oblique and transverse fracture patterns[2,3].
In 1996, for the treatment of unstable per-, intra- and subtrochanteric femur fractures the AO/Association for the Study of Internal Fixation designed the PFN as an intramedullary (IM) device[4]. It is routine practice to perform distal interlocking for fracture fixation while using PFN. Distal interlocking screws of the IM nail were made to avoid longitudinal or rotational instability as well as movement of distal tip of nail in cases of a broad canal for the IT fracture[5]. Nonetheless, drawback of the distal interlocking screw, like loosening, breaking and subsequent peripheral injures, and secondary femur fractures could not be ignored due to the minimal advantages gained[6].
The purpose of this study was to compare the outcomes of IT fractures (AO/OTA 31-A1 and 31-A2) treated by PFN with and without distal interlocking. We hypothesized that PFN without distal interlocking could be a dependable and acceptable option for IT fractures (AO/OTA 31-A1 and 31-A2).
We conducted a retrospective study among 140 patients with AO/OTA 31-A1 and 31-A2 fractures treated with PFN at our institute from November 2016 to November 2019. The patients were divided into two equal groups, as follows: 70 patients treated with PFN with distal interlocking screws (group 1); and 70 patients treated without distal interlocking screws (group 2). The same chief surgeon performed the operations of all of the patients.
Inclusion criteria included AO/OTA 31-A1 and AO/OTA 31-A2 fracture pattern, age more than 20 years, no other injury or fracture, and those treated with long anatomical design PFN. Exclusion criteria included AO/OTA 31-A3 fracture pattern, age less than 20 years, patients lost to follow-up, patients having surgical site infection, and those treated with short PFN.
In our institute, standard preoperative workup included radiographic evaluation of the fracture type along with blood, medical and anaesthetic assessments. Postoperative protocol included intravenous antibiotics given for 48 h followed by oral antibiotics. On postoperative day 1 of surgery, bedside knee bending, static quadriceps exercises and ankle toe mobilisation exercises were started under supervision of a physical therapist. Regular stitch dressings were completed every third day, and stitches were removed between 12-14 d postoperatively. All patients were sent to the same rehabilitation program. Patients were followed up weekly for the first month after surgery. After that, they received follow-up care every 15 d for the next 2 mo and then monthly follow-up for 14 mo.
The patients were evaluated based on the following clinical and radiological parameters: (1) Fracture patterns according to the AO/OTA classification; (2) Duration of surgery (starting from skin incision to skin closure); (3) Time of IITV radiation exposure; (4) Time to radiological union; (5) Implant-related complications like backing-out of proximal screws from the lateral cortex of the femur, ‘Z’ effect, screw breakage, cut-through of implant from femoral head, breakage of distal interlocking screw, and breakage of nail; (6) Anatomy of the proximal femur (neck shaft angle of femur); (7) Level of the distal lock screw in relation to the nail in the anterior posterior (AP) view of the postoperative radiograph and radiograph after union were compared in group 1 and the downward migration of the nail in the IM canal in the AP view of the postoperative radiograph and radiograph after union were compared in group 2; and (8) Length and rotation of the limb after healing.
Out of 140 patients, the 70 patients in group 1 were treated with PFN with distal interlocking screws. Among these, 24 were male and 46 were female, and 32 patients had AO/OTA 31-A1 fracture pattern and 38 patients had AO/OTA 31-A2 fracture pattern. In group 2, 70 patients were treated with PFN without distal interlocking screws. Among these, 29 were male and 41 were female, and 28 patients had AO/OTA 31-A1 fracture pattern and 42 patients had AO/OTA 31-A2 fracture pattern. (Table 1)
| Group-1 (with distal locking) | Group-2 (without distal locking) | |
| Male | 24 | 29 |
| Female | 46 | 41 |
| Total patients | 70 | 70 |
| 31-A1 | 32 | 28 |
| 31-A2 | 38 | 42 |
The average operation time in group 1 was 42 min, and IITV radiation time was 59 s. In group 2, the average operative time was 28 min (P < 0.001) and IITV radiation time was 45 s (P < 0.001). This suggests that there was a significant reduction in operative time and IITV radiation time in group 2. (Table 2)
| Group-1 | Group-2 | P value | |
| Average operative time | 42 min | 28 min | < 0.001 |
| Average IITV radiation time | 59 s | 45 s | < 0.001 |
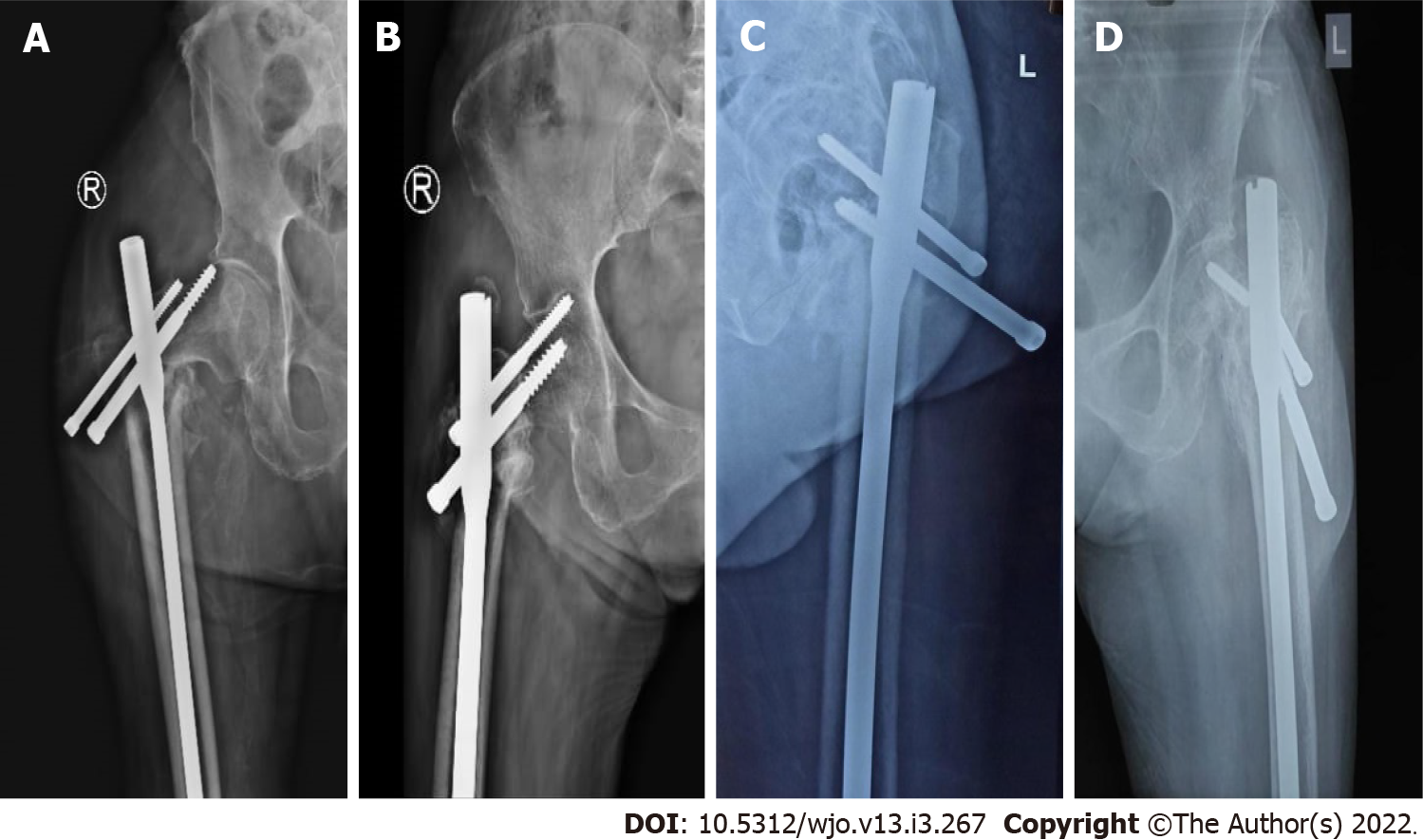
As shown in Table 3, In group 1, 2 out of 70 (2.85%) patients had screw cut-out (Figure 2A), 3 out of 70 (4.28%) patients had Z-effect (Figure 2B), 9 out of 70 (12.85%) patients had a proximal screw back-out (average back-out = 14 mm) (also Figure 2C), and 1 out of 70 (1.42%) patients had proximal screw breakage (also Figure 2D). In group 2, 4 out of 70 (5.71%) patients had a proximal screw back-out (average back-out = 7 mm). There was no Z-effect, screw breakage or proximal screw cut-out.
| Group-1 (n = 70) | Group-2 (n = 70) | |||
| 31A1 (n = 32) | 31A2 (n = 38) | 31A1 (n = 28) | 31A1 (n = 42) | |
| Proximal screw backout | 01 | 08 | 00 | 04 |
| Proximal screw breakage | 00 | 01 | 00 | 00 |
| Proximal screw cut out | 00 | 02 | 00 | 00 |
| Z effect | 00 | 03 | 00 | 00 |
Average time of union was 14-16 wk in both groups for patients having fracture pattern AO/OTA 31-A1. However, in fracture pattern AO/OTA 31-A2, the average union time was 16-18 wk in group 1 and 15-16 wk in group 2 (P < 0.001). There were 3 cases of non-union in group 1 and no cases of non-union in group 2.
Compared to the opposite limb, there was an average of 5 degree external rotation difference in fracture pattern AO/OTA 31-A1 in both groups (P = 0.66). There was an average of 6 degrees more external rotation in group 1 with AO/OTA 31-A2 fracture pattern, and there was an average of 7 degrees more external rotation in group 2 with fracture pattern AO/OTA 31-A2 (P = 0.08). Malrotation of the operated limb was less than 10 degrees in all patients in both groups. This suggests that there was a negligible effect of distal interlocking on the rotational alignment of the limb for fracture patterns AO/OTA 31-A1 and AO/OTA 31-A2.
Varus rotation of the proximal femur was less than 5 degrees in both groups for all patients with AO/OTA 31-A1 (P = 0.81). In AO/OTA 31-A2, the mean neck shaft angle in group 1 was 117 degrees (114-125 degree), and the mean neck shaft angle in group 2 was 126 degrees (124-135 degree) (P < 0.001). This suggests that there was better control of the neck shaft angle where distal interlocking was not performed.
We consider downward migration of the nail as a decrease in distance between the tip of the nail and the upper border of the intercondylar notch of the femur on the AP view of the radiograph. In group 2, 6 out of 70 patients had downward migration of the nail due to controlled collapse of the fracture site, which averaged 5 ± 2 mm. Moreover, in 3 out of 70 patients in group 1, we observed that there was a change in position of the nail in relation to the distal dynamic interlocking screw. There was no downward migration of the nail in the patients in group 1 with static distal locking.
In group 1, we noted thigh pain over the distal locking site in 19 out of 70 (27.14%) patients, and 1 out of 70 patients had breakage of the distal lock due to downward migration of the nail resulting in auto-dynamization (Figure 3). No thigh pain was reported for any patient in group 2. In the postoperative period, 5 out of 70 patients in group 1 had knee joint effusion, and no patient had knee joint effusion in group 2.
In group 1, 6 out of 70 patients had limb length discrepancy with mean shortening of 12 mm (6-18 mm), 10 out of 70 patients had implant impingement, and 5 out 70 patients had decreased range of movement. In group 2, there was an average of 10 mm of limb shortening (5-15 mm), 1 patient had implant impingement, and all patients had near to normal range of movement as compared to the opposite site.
IT femur fractures amount to almost half of total hip fractures caused by a low-energy injury, like a fall from standing height. These fragility hip fractures occur in a population with risk factors including elderly age, female sex, osteoporosis, history of trauma and gait problems[7]. IT fractures are not common in young age patients and require investigation; in this population, IT fractures are caused by high-energy injuries or from a pathological process. Thus, secondary injuries or malignancies must be ruled out[8]. Surgery is typically the recommended treatment as the morbidity and mortality associated with non-operative treatment has been high historically. Patients often have pre-existing comorbidities that dictate the ultimate outcome.
Diagnosis is confirmed by plain radiographs in the AP and lateral views. Traction with internal rotation radiograph view is helpful in assessing significant fracture displacement if the patient is able to tolerate. The antero-posterior and lateral X-ray views of the whole femur are required for long anatomical PFN fixation.
The treatment of proximal femoral fractures with sliding hip screw implants involving an extramedullary or an IM device is a universally accepted method of fixation[4]. In IM fixation there is minimal soft tissue dissection, less blood loss, a lower chance of infection, and fewer wound complications than extramedullary fixation, which has popularized PFN in IT fractures.
At present, PFN is a favourable minimally invasive technique for treating proximal femur fractures, especially where closed reduction is achievable. Nonetheless, proximal lag screw cut-out, Z-effect, reverse Z-effect, femur fracture at the tip of nail or at the site of distal screw insertion, thigh pain as a result of iliotibial tract irritation or cortical hypertrophy and difficulty in insertion of distal interlocking screw are among the probable complications that can occur[1].
There was no pre-established treatment protocol for choosing a long nail or short nail for femoral IT fractures. However, many surgeons are reluctant to use short nails based on the historic literature showing high fracture rates. They also believe that long nails will avoid diaphyseal stress risers and make peri-prosthetic fracture rates acceptable[9]. Short PFNs do not follow the anatomical curvature and the tip may impinge the endosteum of the anterior femoral cortex giving rise to anterior thigh pain. Long PFNs follow the anatomical shape of the femur and would not cause such a problem. At our institute, we have been using long anatomical PFNs. We routinely use long PFN with two proximal interlocks that maintain IT fracture reduction in good valgus position and provide excellent rotational control of the proximal fragment.
Hardware or fixation failure is not related to the type of nail, implant material or AO/OTA classification, but a neck shaft angle of < 125 degrees leads to a significant increase in fixation failure[10]. The influence of varusmal reduction for femur neck fractures and trochanteric fractures was described previously[11]. An increased varus reduction is associated with a higher cut-out rate after sliding hip screw fixation. An increased valgus reduction is beneficial for screw positioning resulting in stable fixation of the femoral head and neck[12]. Kashigar et al[13] showed a significant association between an increased varus reduction and cut-out for cephalo-medullary nailing. In addition to nail design, surgical method is also an important factor in determining the incidence of the above-mentioned complications.
Some personnel have supported the IM nailing without distal locking through their biomechanical studies. A biomechanical study done by Lacroix et al[14] comprised of 10 paired human cadaveric femurs and gave significant support that an added hole in the distal part of the IM nail could reduce the mean failure load in torsion by 36% because a stress raiser is a factor for peri-implant fracture.
The pattern of the fracture had a significant effect on the distal interlocking of the nail. In stable IT fractures (31-A1 and 31-A2), the lateral cortex of the femur is unaffected. After anatomical reduction when the proximal locks are inserted from the lateral wall of the distal fracture part into the femoral head and the IM nail is matched well to the medullary canal, then varus deformity of the hip joint and rotational instability are controlled by the nail-proximal lock structure. In stable IT fractures, good cortical connection is established after acceptable reduction, and most of the compressive forces on the fracture site are borne by the bony cortex along the axis of neck of femur after surgery. Thus, performing distal interlocking of the nail was found to be unnecessary.
In unstable IT fractures (31-A3), the lateral cortex of the femur is fractured. This includes reverse oblique and transverse fracture patterns with particular anatomical and mechanical properties. Weight bearing on the affected limb gives rise to shearing movement at the fracture site that results in telescoping of the implant[15]. When IM nailing of this unstable fracture pattern was done without distal interlocking screws, neither longitudinal nor rotational stability was attained. Thus, this fracture is not fixed firmly without a distal interlocking screw. However, we concluded that distal interlocking screws are needed for unstable IT fractures (31-A3), particularly those with subtrochanteric extension of the fracture or those with wide IM canals.
Hardy et al[16] stated that use of two static locking screws during IM fixation of IT fractures is correlated with a higher rate of cortical hypertrophy, while the use of a dynamically locked nail significantly decreases the rate of this complication. On the basis of these findings, we discontinued the use of distal interlocking screws in AO/OTA 31-A1 and 31-A2 IT femur fractures.
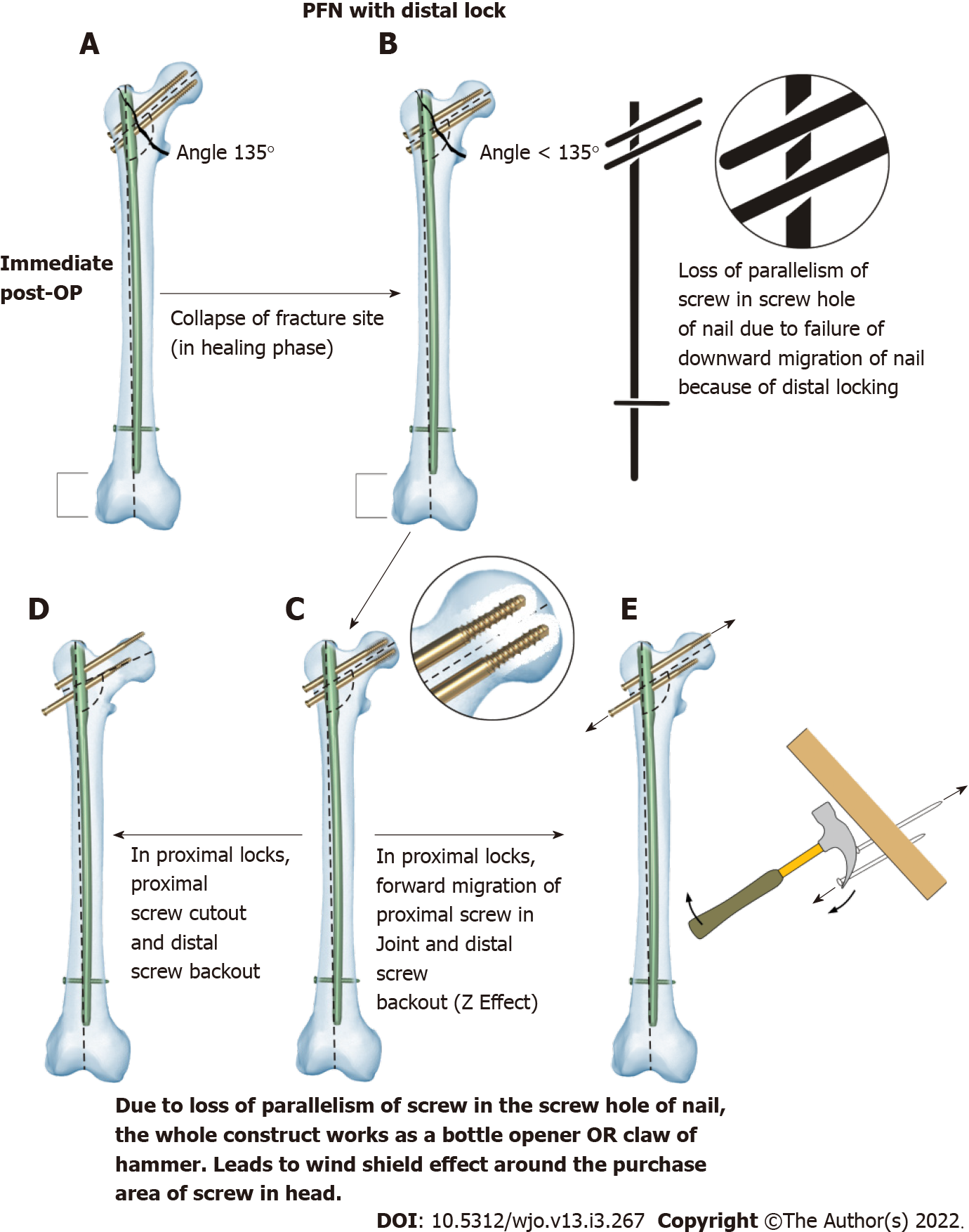
Figure 4 shows a typical case where PFN with distal locking was performed. In the immediate postoperative period (Figure 4A), the proximal femoral neck shaft angle was maintained. In the healing phase, there was collapse of the fracture site, but the proximal femoral neck shaft angle was not maintained. There was loss of parallelism of the screw in the screw hole of the nail due to failure of downward migration of the nail because of distal locking (Figure 4B). The whole construct works as a bottle opener or hammer claw, that leads to a windshield wiper effect around the purchase area of the screw in the head (Figure 4C) resulting in forward migration of the proximal lag screw and back-out of the distal lag screw. Due to this loss of parallelism, there can be screw back-out, screw cut-through from the femoral head (Figure 4D), Z-effect (Figure 4E), reverse Z-effect, and screw breakage.
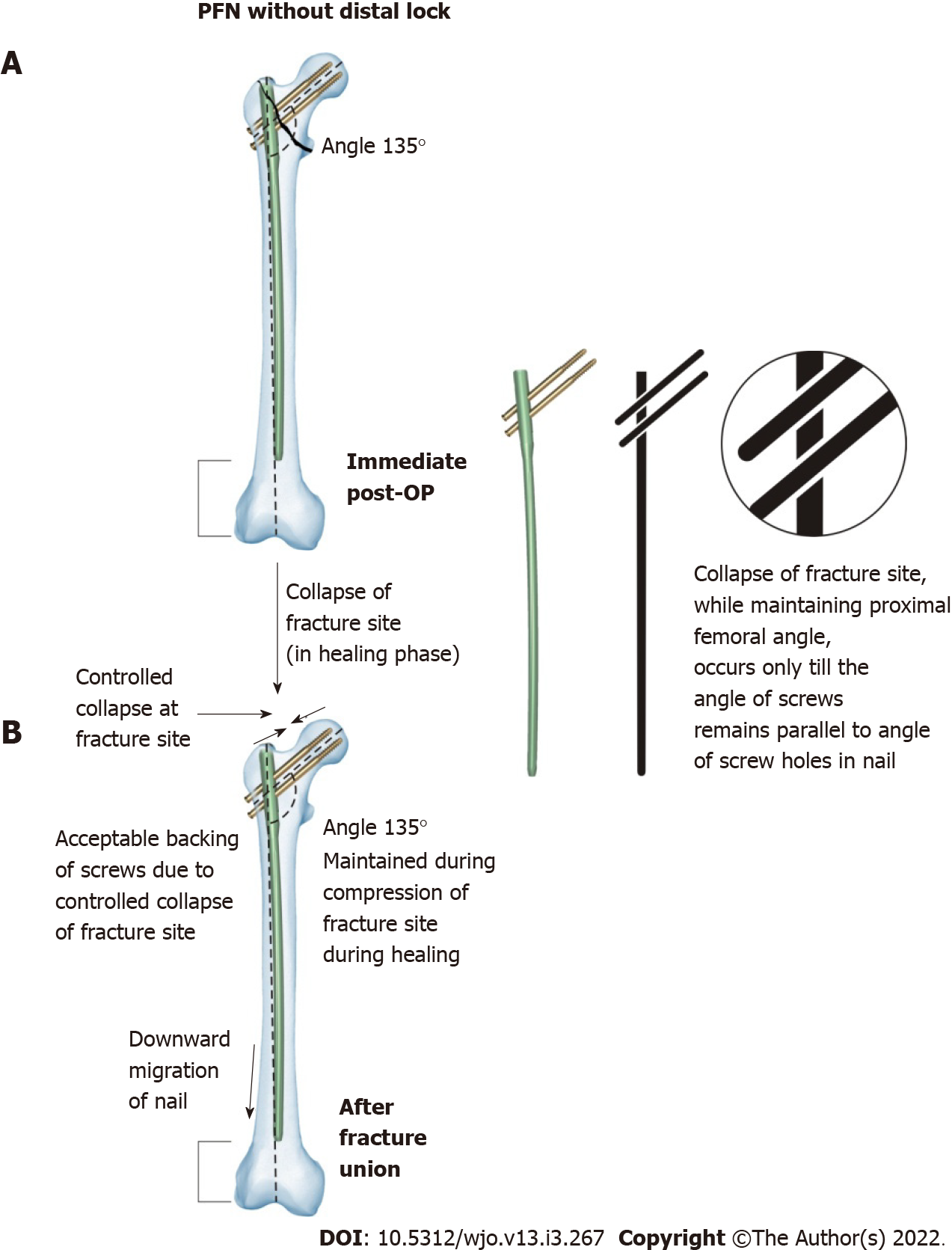
Figure 5 shows a scenario where PFN with distal locking was not performed. It was observed during the postoperative period that the proximal femoral neck shaft angle was maintained. In the healing phase, controlled collapse of the fracture site occurred. During controlled collapse of the fracture site, the proximal neck shaft angle was maintained until the angle of the screws remained parallel to the screw holes in the nail. Parallelism of the screws in the screw holes was maintained due to downward migration of the nail in the canal during the healing phase. Also, there was acceptable backing-out of screws due to collapse of the fracture site.
Metaphyseal fractures heal by direct bone contact and creeping substitution. In comminuted IT femur fracture, controlled collapse at the fracture site is desirable for fracture union because of resorption and comminution at the fracture site. Therefore, in such situations, if there is a static implant bone construct, then there would be an increase in friction at the junction of the nail and screws (Figure 4). This would increase probability of Z-effect, reverse Z-effect, implant breakage, cut-through of screws and back-out of lag screws in the proximal femur. Whereas in cases where distal locking was not performed, the parallelism between the screw hole and screw will be maintained, and the controlled desired collapse with a maintained neck shaft angle would occur, which would increase the chances of fracture union (Figure 5).
In PFN that is done without distal locking, it is desirable to keep the nail length up to the superior border of the patella. A nail with a length up to the intercondylar notch of the femur will not allow downward migration. Therefore, it is desirable to keep a nail short to allow downward migration of the nail with controlled collapse of the fracture.
In our study, it was noted that in the cases for which distal interlocking was performed, there was a gradual decrease in the neck shaft angle, which led to varus collapse and failure of bone implant construct in 21.40% of patients.
There was no significant difference in radiological union, postoperative rotational alignment and proximal femur anatomy between both groups with fracture pattern AO/OTA 31-A1, but the incidence of proximal lock-related complications was increased in group 1 patients with fracture pattern AO/OTA 31-A2 than in group 2 patients with fracture pattern AO/OTA 31-A2 (Table 3).
The limitations of our study were a short follow-up period and a small sample size. We also used only one type of long anatomically designed PFN with two proximal locks.
A 68-year-old female patient sustained an IT femur fracture (AO/OTA 31-A2) on the right side (Figure 6A). A long anatomical PFN with two proximal screws without distal interlocking were used for the operation, as shown in immediate postoperative X-ray (Figure 6B). The X-ray image in Figure 6C showed a complete union at 12 mo with maintained neck shaft angle and distal downward migration of the nail, as compared to that in Figure 6B.
From this study, we concluded that in IT fractures AO/OTA type 31-A1, use of long anatomical PFN with or without distal interlocking screws gives similar results in terms of radiological union, postoperative proximal femur anatomy, and rotational alignment. However, in AO/OTA type 31-A2, use of long anatomical PFN without distal interlocking screws gave better results and less proximal lock-related complications than PFN with distal interlocking screws.
There are few studies comparing clinical and radiological outcomes between proximal femoral nail (PFN) with or without distal interlocking screws in fracture pattern Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 31-A1 and 31-A2.
The motivation of this study was to assess the clinical and radiological outcomes of PFN with or without distal interlocking screws in fracture pattern AO/OTA 31-A1 and 31-A2, which were performed by the same chief surgeon.
The objective of this study was to compare the outcomes of intertrochanteric (IT) fractures (AO/OTA 31-A1 and 31-A2) treated by PFN with and without distal interlocking screws.
We conducted a retrospective study of 140 patients having fracture pattern AO/OTA 31-A1 and 31-A2. We divided the patients into two groups based on distal interlocking. We evaluated patients based on clinical and radiological parameters like fracture type, duration of surgery and IITV radiation time, time for radiological union, proximal lock and distal lock-related complications, femoral neck shaft angle and length and rotation of limb after surgery.
There was no significant difference in radiological union, postoperative radiological alignment and proximal femur anatomy between patients with fracture pattern AO/OTA 31-A1 treated by PFN with or without distal interlocking. However, the incidence of proximal lock-related complications was higher in patients with fracture pattern AO/OTA 31-A2 treated by PFN with distal interlocking than in patients treated by PFN without distal interlocking.
PFN without distal interlocking is a reliable and acceptable option for IT fracture types AO/OTA 31-A1 and 31-A2.
A prospective study with long-term follow-up and a larger number of patients is necessary to draw a definitive conclusion.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Pavone V, Veltman ES S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Ozkan K, Unay K, Demircay C, Cakir M, Eceviz E. Distal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fractures. Int Orthop. 2009;33:1397-1400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Kregor PJ, Obremskey WT, Kreder HJ, Swiontkowski MF; Evidence-Based Orthopaedic Trauma Working Group. Unstable pertrochanteric femoral fractures. J Orthop Trauma. 2005;19:63-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Schipper IB, Steyerberg EW, Castelein RM, van der Heijden FH, den Hoed PT, Kerver AJ, van Vugt AB. Treatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br. 2004;86:86-94. [PubMed] [Cited in This Article: ] |
| 4. | Boldin C, Seibert FJ, Fankhauser F, Peicha G, Grechenig W, Szyszkowitz R. The proximal femoral nail (PFN)--a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 months. ActaOrthopScand. 2003;74:53-58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 139] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Skála-Rosenbaum J, Bartonícek J, Bartoska R. Is distal locking with IMHN necessary in every pertrochanteric fracture? Int Orthop. 2010;34:1041-1047. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Li X, Zhang L, Hou Z, Meng Z, Chen W, Wang P, Zhang Y. Distal locked and unlocked nailing for perthrochanteric fractures--a prospective comparative randomized study. Int Orthop. 2015;39:1645-1652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Grisso JA, Kelsey JL, Strom BL, Chiu GY, Maislin G, O'Brien LA, Hoffman S, Kaplan F. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med. 1991;324:1326-1331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 567] [Cited by in F6Publishing: 585] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 8. | Ahn J, Bernstein J. Fractures in brief: intertrochanteric hip fractures. ClinOrthopRelat Res. 2010;468:1450-1452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Li Z, Liu Y, Liang Y, Zhao C, Zhang Y. Short versus long intramedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. Int J Clin Exp Med. 2015;8:6299-6302. [PubMed] [Cited in This Article: ] |
| 10. | Hoffmann MF, Khoriaty JD, Sietsema DL, Jones CB. Outcome of intramedullary nailing treatment for intertrochanteric femoral fractures. J OrthopSurg Res. 2019;14:360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 11. | Parker MJ. Valgus reduction of trochanteric fractures. Injury. 1993;24:313-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Jung EY, Oh IT, Shim SY, Yoon BH, Sung YB. The Effect of Valgus Reduction on the Position of the Blade of the Proximal Femoral Nail Antirotation in Intertrochanteric Hip Fractures. ClinOrthopSurg. 2019;11:36-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir O, Kuzyk PR. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J. 2014;96-B:1029-1034. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 101] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 14. | Lacroix H, Arwert H, Snijders CJ, Fontijne WP. Prevention of fracture at the distal locking site of the gamma nail. A biomechanical study. J Bone Joint Surg Br. 1995;77:274-276. [PubMed] [Cited in This Article: ] |
| 15. | Ozkan K, Eceviz E, Unay K, Tasyikan L, Akman B, Eren A. Treatment of reverse oblique trochanteric femoral fractures with proximal femoral nail. Int Orthop. 2011;35:595-598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Hardy DC, Drossos K. Slotted intramedullary hip screw nails reduce proximal mechanical unloading. ClinOrthopRelat Res. 2003;176-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |