Published online Oct 10, 2016. doi: 10.5306/wjco.v7.i5.406
Peer-review started: February 22, 2016
First decision: March 25, 2016
Revised: June 18, 2016
Accepted: August 11, 2016
Article in press: August 13, 2016
Published online: October 10, 2016
To identify factors associated with Papanicolaou-smear (Pap-smear) cervical cancer screening rates in a safety net population.
From January 2012 to May 2013, the use of Pap-smear was determined for all patients seen at the breast clinic in a safety net hospital. Health literacy assessment was performed using the validated Newest Vital Sign. The records of patients were reviewed to determine if they had undergone Pap-smears for cervical cancer screening. Sociodemographic information was collected included age, education, monthly income, race/ethnicity, employment, insurance status, and primary care provider of the patient. Logistic regression analysis was then performed to determine factors associated with utilization of Pap-smears. Crude and adjusted odds ratios derived from multivariate logistic regression models were calculated as well as the associated 95%CIs and P-values.
Overall, 39% had Pap-smears in the prior 15 mo, 1377 consecutive women were seen during the study period and their records were reviewed. Significantly more patients with adequate health literacy underwent Pap-smears as compared to those with limited health literacy (59% vs 34%, P < 0.0001). In multivariate analysis, patients with adequate health literacy, younger patients, and those with later age of first live birth were more likely to undergo Pap-smears. Patients whose primary care providers were gynecologists were also significantly more likely to have Pap-smears compared to other specialties (P < 0.0001). Patients younger than 21 years or older than 65 years underwent screening less frequently (11% and 11%, respectively) than those 21-64 years (41%, P < 0.0001). Race, ethnicity, language, and insurance status were not associated with Pap-smear screening rates.
Patient health literacy and primary care physician were associated with Pap-smear utilization. Development of interventions to target low health literacy populations could improve cervical cancer screening.
Core tip: Patient health literacy and type of primary care physician were associated with Papanicolaou-smear utilization. Development of interventions to target low health literacy populations could improve cervical cancer screening and therefore improve screening in populations most at risk for cervical cancer.
- Citation: Heberer MA, Komenaka IK, Nodora JN, Hsu CH, Gandhi SG, Welch LE, Bouton ME, Aristizabal P, Weiss BD, Martinez ME. Factors associated with cervical cancer screening in a safety net population. World J Clin Oncol 2016; 7(5): 406-413
- URL: https://www.wjgnet.com/2218-4333/full/v7/i5/406.htm
- DOI: https://dx.doi.org/10.5306/wjco.v7.i5.406
Cervical cancer is one of the most preventable and treatable female cancers. While cervical cancer death rates have decreased, it remains a significant burden in all countries. Cervical cancer screening rates are most suboptimal among recent immigrants to developed countries, in countries without screening programs, among racial and ethnic minorities, women from low socioeconomic backgrounds, and underinsured populations[1-3]. Most studies show higher rates of cervical cancer and lower compliance with cervical cancer screening in these populations[1-3].
Previous studies have found that patients do not understand the concept of screening or did not realize that Pap-smears are a test for cervical cancer. One population studied was less likely to undergo screening because they “didn’t have problems/symptoms”[4]. A second study found that patients thought Papanicolaou-smear (Pap-smears) were for infections, gonorrhea, or HIV[5]. Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions[6]. In 2003, the National Assessment of Adult Literacy (NAAL) reported that over 89 million American adults have limited health literacy skills and that individuals with limited health literacy come from all parts of society[7,8]. In fact, the NAAL survey, which rated health literacy skills in four levels ranging from “below-basic” to “proficient”, showed that more than 40% of high school graduates and 13% of college graduates have health literacy skills at the lowest two levels and are thus considered to have limited health literacy[8,9]. Similarly, the 2011 Programme for the International Assessment of Adult Competencies which evaluated adults in 23 industrialized countries indicated continuing issues: A significant proportion of adults scored below average for literacy, numeracy, and problem solving in technology-rich environments[10]. The number of patients with low health literacy is increasing and is more common among those with low educational attainment, immigrants, elderly, and racial/ethnic minorities[7,11]. These individuals are less able to navigate the health care system and less likely to participate in preventive health care[12-16]. The current study was performed to identify factors that influence use of Papanicolaou cytology smears for cervical cancer screening in a safety net population.
This study was conducted at Maricopa Medical Center in Phoenix, Arizona, and reviewed and approved by the medical center’s institutional review board. The institutional review board also granted a waiver of informed consent for this study. Maricopa Medical Center is the safety net hospital for Maricopa County, which includes the city of Phoenix and the surrounding metropolitan area. Maricopa County is the state’s most populous area with nearly four million of Arizona’s 6.5 million inhabitants. Maricopa Medical Center serves a patient population of which 78% of patients are from racial/ethnic minority groups and 79% are underinsured, uninsured, or insured by Medicaid.
Beginning on January 1, 2012 and continuing until May 31, 2013, every patient seen in the Breast Clinic underwent a health literacy assessment as part of their routine history and physical examination. Health literacy assessment involves the use of validated instruments. The Newest Vital Sign was chosen because it can be administered in about 2 min, and therefore is feasible for use in clinical practice rather than strictly a research setting. In addition, it has the advantage of having been validated in both English and Spanish[17-19].
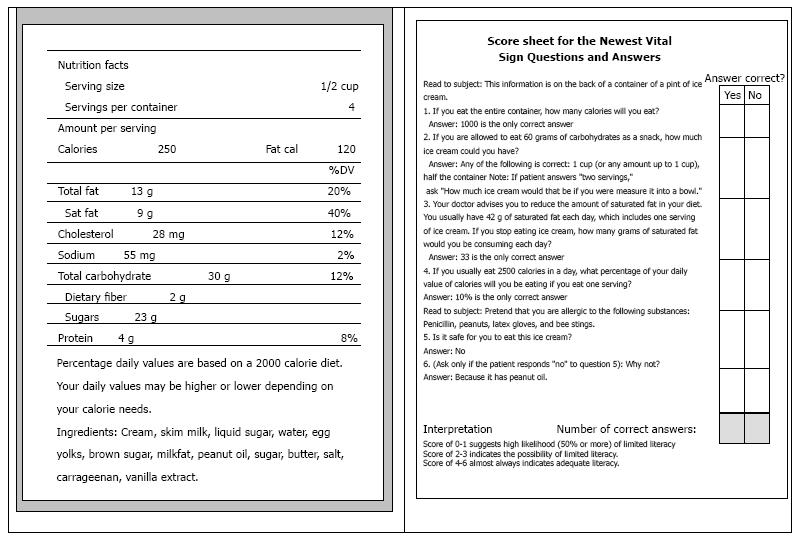
The Newest Vital Sign uses a nutrition label, similar to the nutrition label present on all packaged food in the United States. The nutritional label was tested as one of many scenarios developed by a panel of health literacy experts based on concepts and types of scenarios used in health literacy research and in general literacy assessments. The candidate scenarios tested involved both reading and numeracy skills as this was driven by research indicated that these skills are highly correlated with one another, plus an intuitive understanding that patients must be able to use and understand both text and numbers if they are to successfully deal with today’s health care system. Of the candidate scenarios tested, the nutritional label performed the best and has been validated and correlates well with more complicated health literacy instruments[17].
The assessment involves asking the patient five questions (and a sixth qualifier question, if needed) about the nutrition label (Figure 1). One point is awarded for each correct answer. Instructions accompanying the nutrition label specify what the interviewer should ask and they list the only acceptable answer(s). Scoring instructions for the Newest Vital Sign place patients into 3 groups, depending on how many of the 6 questions are answered correctly. A score of 0-1 indicates a high likelihood of limited health literacy. A score of 2-3 indicates the possibility of limited health literacy. Score of 4-6 indicate adequate health literacy. The instrument validation, including its sensitivity and specificity among Spanish speakers has been previously described[17].
The details of incorporating routine health literacy assessment as part of the standard history and physical examination have been described previously[19]. In short, the assessment was performed by the clinician during the history and physical examination. However, if the patient was Spanish speaking, the assessment was performed by a hospital certified Spanish translator or a clinician who was a native-Spanish speaker. No special personnel or other resources were used for performance of the health literacy assessment. Patients were excluded from health literacy assessment if they did not speak English or Spanish, had visual impairment that prevented them from viewing the nutritional label, or had cognitive limitations due to developmental delay, dementia, psychiatric illness, or head injury.
The records of patients receiving care during the study period were reviewed to determine if they had undergone Papanicolaou cytology smears (Pap-smears) for cervical cancer screening. If there was no record in the medical system of a Pap-smear, the patient was asked about their last screening and documentation was obtained via contact with prior health facilities or providers to confirm the date and results.
Patients were excluded and no attempt was made to obtain Pap-smear results on patients if they had undergone hysterectomy for reasons other than cervical cancer or had not yet initiated sexual activity. All other patients were considered to have undergone screening if they had done so in the year based on the more guidelines and recommendations for annual Pap-smears as of January 2012. Many insurance payors, however, will not pay for repeat screenings in durations even one day less than one calendar year. Therefore patients will often be scheduled for subsequent screenings in 13 or 14 mo. To account for this issue, a 15 mo time period was chosen to give some room for error on the “annual screening”.
For all patients, sociodemographic information was collected and included age, education, self-reported monthly income, race/ethnicity, employment status, and insurance status. Patients were also queried about their reproductive status, height and weight, current smoking status, and use of alcohol. Finally, data were collected on whether or not the patient had a primary care provider and the type of provider.
Age, education, body mass index (height/weight2), number of live births, and estimated monthly income were analyzed as continuous variables. Race/ethnicity (non-Hispanic white vs other, Hispanic vs non-Hispanic), employment status, insurance status (uninsured vs insured), and primary care provider were analyzed as categorical variables. Adequacy of health literacy was analyzed as a categorical variable. Patients with Newest Vital Sign 4-6 were categorized as having “adequate health literacy”. Patients with Newest Vital Sign scores of 0-1 and 2-3 had similar use of Pap-smears and were therefore combined into a single group labeled “low health literacy”. Analysis of the data did not demonstrate differences when the patients were categorized in three groups or in the two groups as presented. A two-sample t-test was used to determine if there were significant differences in continuous variables between women who did and did not undergo Pap-smears. A Fisher’s exact test was used to assess differences in the categorical variables. All statistical tests were two sided and significance levels were set at 0.05.
Logistic regression analysis was then performed with the dependent variable being whether or not a patient had undergone Pap-smears. Independent variables included health literacy (adequate vs low literacy) and the sociodemographic variables listed in Table 1. Factors shown to have P < 0.1 in univariate analysis were included in the multivariate model. Crude and adjusted odds ratios (ORs) derived from multivariate logistic regression models were calculated as well as the associated 95%CIs and P values.
| All patients (n = 1318) | |
| Mean age, years (SD) | 45.0 (13.1) |
| Race/ethnicity | |
| Non-Hispanic White | 230 (17%) |
| African American | 131 (10%) |
| Hispanic | 888 (67%) |
| Other | 69 (5%) |
| Language, English | 591 (45%) |
| Mean age of menarche (SD) | 12.8 (1.88) |
| Mean pregnancies (SD) | 3.3 (2.32) |
| Mean live births (SD) | 2.7 (1.97) |
| Mean age of first live birth (SD) | 21.0 (4.43) |
| Education, years | |
| 6 or less | 286 (22%) |
| 7-11 | 340 (26%) |
| High school/equivalent | 324 (25%) |
| Some college | 368 (28%) |
| Adequate health literacy | 229 (17%) |
| Body mass index in kg/m2 (SD) | 29.3 (7.57) |
| Marital status - married | 555 (42%) |
| Employment, employed | 456 (35%) |
| Insurance status | |
| Commercial | 60 (5%) |
| Medicare | 45 (3%) |
| Medicaid | 312 (24%) |
| None | 900 (68%) |
| Monthly income $US (SD) | 1099 (878.46) |
| Screening mammography (age ≥ 40 yr) | 253/899 (28%) |
| Pap smear in last 15 mo | 514 (39%) |
The statistical methods of this study were performed and reviewed by a biomedical statistician (CHH).
A total of 1377 consecutive patients were seen from January 1, 2012 and continuing until May 31, 2013. Fifty-nine patients were excluded because they were not yet sexually active or had hysterectomy for an indication other than cervical cancer. The remaining 1318 patients made up the study population (Table 2). The average age of the women was 45 years and the minority was non-Hispanic White (17%), while 10% were African American and 67% were Hispanic. Only 45% spoke English as their primary language. The vast majority (92%) were underinsured (24% Medicaid and 68% uninsured). The mean monthly income was $1099. Patients completed an average of 10 years of education.
| Variables | Unadjusted | Adjusted2 | |||
| Rate | OR | P-value1 | OR | P-value | |
| Age (per year) | 45.17 ± 12.64 | 0.97 (0.96, 0.98) | < 0.0001 | 0.97 (0.96, 0.99) | < 0.0001 |
| Non-Hispanic White race | 0.92 (0.68, 1.23) | 0.6029 | - | ||
| No | 429/1088 | ||||
| Yes | 86/230 | ||||
| Hispanic ethnicity | 1.16 (0.91, 1.47) | 0.2294 | - | ||
| No | 158/430 | ||||
| Yes | 357/888 | ||||
| Pregnancies (per pregnancy) | 3.31 ± 2.28 | 0.95 (0.90, 0.99) | 0.0277 | 1.07 (0.95, 1.20) | 0.2537 |
| Live births (per birth) | 2.70 ± 1.95 | 0.91 (0.85, 0.96) | 0.0011 | 0.90 (0.77, 1.04) | 0.1556 |
| Age of 1st live birth (per year) | 20.96 ± 4.42 | 1.05 (1.02, 1.07) | 0.0013 | 1.04 (1.01, 1.08) | 0.0121 |
| Body mass index, kg/m2 (per unit) | 29.29 ± 7.57 | 0.988 (0.972, 1.003) | 0.1224 | - | |
| Language | 1.09 (0.87, 1.36) | 0.4622 | - | ||
| English | 235/619 | ||||
| Other | 280/699 | ||||
| Education (per year) | 10.40 ± 3.80 | 1.05 (1.02, 1.08) | 0.0012 | 1.00 (0.96, 1.04) | 0.9472 |
| Low HL | 368/1056 | 2.73 (2.04, 3.66) | < 0.0001 | 2.05 (1.38, 3.03) | 0.0003 |
| Adequate HL | 136/229 | ||||
| Married | 1.19 (0.95, 1.48) | 0.1375 | |||
| No | 285/763 | - | |||
| Yes | 230/555 | ||||
| Menopausal | 0.42 (0.32, 0.54) | < 0.0001 | 0.88 (0.58, 1.31) | 0.5192 | |
| No | 410/909 | ||||
| Post | 105/409 | ||||
| Employed | 1.39 (1.11, 1.76) | 0.0053 | 1.04 (0.78, 1.37) | 0.8023 | |
| No | 313/862 | ||||
| Yes | 202/456 | ||||
| Income (per $1000US/mo) | 1.10 ± 8.78 | 1.44 (1.26, 1.64) | < 0.0001 | 1.29 (1.09, 1.51) | 0.0024 |
| Insured | 141/418 | 1.40 (1.10, 1.78) | 0.0076 | 1.22 (0.90, 1.65) | 0.1977 |
| Uninsured | 374/900 | ||||
| Current smoker | 0.80 (0.60, 1.06) | 0.1211 | |||
| No | 423/1054 | - | |||
| Yes | 92/264 | ||||
| Screening mammography | 1.46 (1.11, 1.92) | 0.0081 | 1.69 (1.22, 2.35) | 0.0018 | |
| No | 397/1064 | ||||
| Yes | 118/254 | ||||
| Primary care provider | 427/1182 | 3.24 (2.24, 4.70) | < 0.0001 | 2.81 (1.84, 4.29) | < 0.0001 |
| Others gynecologist | 88/136 | ||||
Overall, 39% underwent a Pap-smear in past year. Table 1 shows the rates of Pap-smear use according to various sociodemographic variables, health literacy, and other factors. Several factors were significantly associated with Pap-smear uptake, including age, education, employment status, number of pregnancies, age at first live birth, and menopausal status. When evaluated by health literacy, significantly more patients with adequate health literacy underwent Pap-smears as compared to those with low health literacy (59% vs 34%, P < 0.0001). Although patients without a primary care provider had Pap-smear rates similar to those with such a provider, the type of provider made a difference. Women who had a gynecologist for their primary care provider were significantly more likely to have Pap-smears (65%) as compared to those who had an internist (23%) or family practitioner (42%, P < 0.0001). Patients less than 21 years of age and those older than 65 years underwent screening less frequently (11% and 11%, respectively) than those age 21-54 years (41%, P < 0.0001).
In multivariate analysis, older age was significantly associated with lower likelihood of undergoing Pap-smear use (P < 0.001), whereas older age of first live birth (P < 0.01) and higher income were associated with higher use (P < 0.0096). Patients who underwent screening mammography were more likely to undergo Pap-smears (OR = 1.69; 95%CI: 1.22-2.35, P = 0.0018). The type of primary care provider also had a significant effect as patients whose primary care provider was a gynecologist were significantly more likely (OR = 2.81; 95%CI: 1.84-4.29, P < 0.0001) to undergo screening than those with other types of providers. Level of health literacy also affected use of Pap-smears as those with adequate health literacy were twice as likely to participate as those with low health literacy (OR = 2.05; 95%CI: 1.38-3.03, P = 0.0003).
Results of this study show that the use Pap-smears in this underinsured population was suboptimal, at 39%. We identified several factors that were independently associated with Pap-smear utilization. Younger patients, patients with later first live birth, and those who participated in screening mammography were more likely to utilize Pap-smears. Women with a gynecologist as their primary care provider and those with adequate health literacy were most likely to undergo Pap-smears.
The finding that Pap-smear screening is underutilized in an underinsured population is not new[20]. However, the factors associated with low screening rates within these populations can provide insight into factors that may improve compliance or to provide targeted screening. In particular, women with adequate health literacy underwent Pap-smear screening twice as much as those with low health literacy. On the other hand, many sociodemographic factors which are thought to influence use of preventative services, such as race/ethnicity, education, employment, and insurance status were not found to be associated with Pap-smear use in the current study[21-23]. We previously reported that limited health literacy was the strongest predictor of non-use of breast cancer screening[14]. In that study, 57% of patients did not realize they should undergo screening mammography or did not understand the concept of screening[14]. In the current study, we found that participation in screening mammography was associated with higher rates of Pap-smear screening, suggesting that understanding the concept of preventive care and the ability to navigate the health care system - both key components of health literacy - are critical to Pap-smear screening. Since it is unclear whether an individual’s level of health literacy can be modified, development of strategies to increase awareness of the importance of prevention in populations with health disparities and limited literacy are critical to improve compliance[24].
In our population comprised of a significant proportion Hispanic women, ethnicity was not a predictor of use of Pap-smears. It is possible that level of acculturation, which we did not assess, may influence screening uptake in these women. However, health literacy may be an adequate proxy for acculturation, as it has been associated with factors related to acculturation (i.e., language, education, employment)[19]. In the current population, patients with adequate health literacy, had reproductive behavior consistent with higher levels of acculturation (fewer pregnancies 2.7 vs 3.6; fewer live births 1.8 vs 3.1; and later age of first live birth 22 years vs 20 years; P < 0.01 for all three factors). Patients with characteristics associated with higher levels of acculturation, were more likely to utilize Pap-smears suggesting that acculturation might play a role[25].
Although having a primary care provider did not influence Pap-smear use, the type of provider was significant. Patients whose primary provider was a gynecologist were three times as likely to undergo screening with Pap-smears compared to those with other providers. It also appears that Pap-smears were not over-utilized as patients under the age of 21 years or over the age of 65 years were less likely (both 11%) to undergo Pap-smears compared to the rest of the population (41%). The time frame of this study was 3 years after the 2009 American College of Obstetrics and Gynecology (ACOG) Practice Bulletin, which was when these age recommendations were changed[26]. This study indicates reasonable assimilation of the 2009 recommendations.
There are limitations to the current study. First, because we asked patients about their use of Pap-smears prior to verifying use, it is possible that some patients were unable to recall this information, and this could underestimate the use of Pap-smears. Not being able to recall that the test was completed or the results, however, somewhat defeats the purpose of screening, since not knowing the results would make patients unaware of necessary follow-up. A second limitation is that in November 2012, there was a change in recommendations for screening to every 3 years[20]. It is possible that clinicians and practitioners immediately instituted the recommendations and could have contributed to the low use. Implementation of new guidelines into clinical practice, however, is frequently inefficient and often requires several years to be implemented[27,28]. Further, there were no differences in the use of Pap-smears before (38%) or after (41%) the change in recommendations, indicating this did not affect the results. A third limitation is that Human papilloma virus testing was not included as part of the study and results may have been different had we included this evaluation. Human papilloma virus testing alone, however, is not recommended for cervical cancer screening in any age group. Pap-smear cytology alone remains the recommended (age 21-29 years) or acceptable (age 30-65 years) method for screening[20].
Most clinicians feel that patients with limited health literacy do not exist in their practice. Surveys in the United States and internationally, however, demonstrate that significant proportions of adults in all countries have limited health literacy skills[7-11]. Patients with limited health literacy are found in all clinical practices and the number of patients with limited health literacy is increasing, particularly with the aging population, increasing number of immigrants, and patients with low educational attainment[7,8,10,11]. No strategies have yet been proven to improve or increase health literacy. Therefore increased awareness of patients with limited health literacy is important in all clinical settings.
The current study found that specialty of the primary care physician, health literacy, along with the patient’s age and older age at first childbirth were associated with Pap-smear utilization. Patients with low health literacy exist in all countries and clinical practices and their numbers are increasing. Development of interventions to target low health literacy populations could improve cervical cancer screening.
Cervical cancer is one of the most preventable and treatable female cancers. Cervical cancer screening rates are most suboptimal among recent immigrants to developed countries, in countries without screening programs, among racial and ethnic minorities, women from low socioeconomic backgrounds, and underinsured populations. Most studies show higher rates of cervical cancer and lower compliance with cervical cancer screening in these populations.
Previous studies have found that patients do not understand the concept of screening or did not realize that Papanicolaou-smears (Pap-smears) are a test for cervical cancer. The number of patients with low health literacy is increasing worldwide and these individuals are less able to navigate the health care system and less likely to participate in preventive health care. The current study is the largest series of consecutive patients at a single institution to evaluate the association of Pap-smear utilization with health literacy and other sociodemographic factors.
This study found that specialty of the primary care physician, health literacy, along with the patient’s age and older age at first childbirth were associated with Pap-smear utilization. Patients with low health literacy exist in all countries and clinical practices and their numbers are increasing. Development of interventions to target low health literacy populations could improve cervical cancer screening.
Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions. In 2003, the National Assessment of Adult Literacy reported that over 89 million American adults have limited health literacy skills and that individuals with limited health literacy come from all parts of society. Similarly, the 2011 Programme for the International Assessment of Adult Competencies which evaluated adults in 23 industrialized countries indicated similar issues: A significant proportion of adults scored below average for literacy, numeracy, and problem solving in technology-rich environments.
Few papers have examined the association of health literacy and use of Pap-smears for cervical cancer screening. The authors of the current study evaluated sociodemographic factors which affected use of Pap-smears. This study found that patients with adequate health literacy and specialty of their primary care provider were more likely to use Pap-smears than other patients.
Manuscript source: Invited manuscript
Specialty Type: Oncology
Country of Origin: United States
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Camacho J, Tsikouras PPT, Yokoyama Y, Zafrakas M S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Arbyn M, Castellsagué X, de Sanjosé S, Bruni L, Saraiya M, Bray F, Ferlay J. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22:2675-2686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 689] [Cited by in F6Publishing: 699] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 2. | Froment MA, Gomez SL, Roux A, DeRouen MC, Kidd EA. Impact of socioeconomic status and ethnic enclave on cervical cancer incidence among Hispanics and Asians in California. Gynecol Oncol. 2014;133:409-415. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Sancho-Garnier H, Tamalet C, Halfon P, Leandri FX, Le Retraite L, Djoufelkit K, Heid P, Davies P, Piana L. HPV self-sampling or the Pap-smear: a randomized study among cervical screening nonattenders from lower socioeconomic groups in France. Int J Cancer. 2013;133:2681-2687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: Cultural influences or access to care? Cancer. 2006;107:184-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 147] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Daley E, Perrin K, Vamos C, Hernandez N, Anstey E, Baker E, Kolar S, Ebbert J. Confusion about Pap smears: lack of knowledge among high-risk women. J Womens Health (Larchmt). 2013;22:67-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Healthy People 2010; US Department of Health and Human Services. Health Communication. 2nd ed. Washington DC: US Government Printing Office 2000; . [Cited in This Article: ] |
| 7. | American Medical Association. AMA Foundation: Health Literacy and Patient Safety. Available from: http// www.ama-assn.org/resources/doc/ama-foundation/healthlitclinicians.pdf. [Cited in This Article: ] |
| 8. | Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. USA: US Department of Education, National Center for Education Statistics (NCES) 2016; . [Cited in This Article: ] |
| 9. | NAAL. Highlights of Findings. Available from: http// nces.ed.gov/naal/health_results.asp. [Cited in This Article: ] |
| 10. | Organisation for Economic Cooperation and Development (OECD). OECD Skills Outlook 2013: First Results from the Survey of Adult Skills. Available from: http// www.oecd-ilibrary.org/education/oecd-skills-outlook-2013_9789264204256-en. 2013. [Cited in This Article: ] |
| 11. | Health literacy: report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281:552-557. [PubMed] [Cited in This Article: ] |
| 12. | Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 759] [Cited by in F6Publishing: 825] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 13. | Weiss BD, Palmer R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board Fam Pract. 2004;17:44-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 147] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Komenaka IK, Nodora JN, Hsu CH, Martinez ME, Gandhi SG, Bouton ME, Klemens AE, Wikholm LI, Weiss BD. Association of health literacy with adherence to screening mammography guidelines. Obstet Gynecol. 2015;125:852-859. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Peterson NB, Dwyer KA, Mulvaney SA, Dietrich MS, Rothman RL. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J Natl Med Assoc. 2007;99:1105-1112. [PubMed] [Cited in This Article: ] |
| 16. | Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 323] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 17. | Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514-522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1443] [Cited by in F6Publishing: 1426] [Article Influence: 75.1] [Reference Citation Analysis (0)] |
| 18. | The Newest Vital Sign. A Health Literacy Assessment Tool for Patient Care and Research. Available from: http//www.pfizer.com/health/literacy/public_policy_researchers/nvs_toolkit. [Cited in This Article: ] |
| 19. | Komenaka IK, Nodora JN, Machado L, Hsu CH, Klemens AE, Martinez ME, Bouton ME, Wilhelmson KL, Weiss BD. Health literacy assessment and patient satisfaction in surgical practice. Surgery. 2014;155:374-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | The American College of Obstetricians and Gynecologists. Screening for Cervical Cancer. Practice Bulletin. 2012;131:1-18. [Cited in This Article: ] |
| 21. | Damiani G, Federico B, Basso D, Ronconi A, Bianchi CB, Anzellotti GM, Nasi G, Sassi F, Ricciardi W. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: a cross sectional study. BMC Public Health. 2012;12:99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 113] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 22. | Stanley SL, Thomas CC, King JB, Richardson LC. Predictors of never being screened for cervical cancer by metropolitan area. J Community Health. 2014;39:400-408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2012;1-207. [PubMed] [Cited in This Article: ] |
| 24. | Thompson B, Vilchis H, Moran C, Copeland W, Holte S, Duggan C. Increasing cervical cancer screening in the United States-Mexico border region. J Rural Health. 2014;30:196-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Nodora JN, Gallo L, Cooper R, Wertheim BC, Natarajan L, Thompson PA, Komenaka IK, Brewster A, Bondy M, Daneri-Navarro A. Reproductive and hormonal risk profile according to language acculturation and country of residence in the Ella Binational Breast Cancer Study. J Womens Health (Larchmt). 2014;23:532-540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | The American College of Obstetricians and Gynecologists. Screening for Cervical Cancer. Practice Bulletin. 2009;109:1-12. [Cited in This Article: ] |
| 27. | Grol R, Grimshaw J. Evidence-based implementation of evidence-based medicine. Jt Comm J Qual Improv. 1999;25:503-513. [PubMed] [Cited in This Article: ] |
| 28. | Green LA, Seifert CM. Translation of research into practice: why we can’t “just do it”. J Am Board Fam Pract. 2005;18:541-545. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |