Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastrointest Pathophysiol. Nov 15, 2014; 5(4): 467-478
Published online Nov 15, 2014. doi: 10.4291/wjgp.v5.i4.467
Published online Nov 15, 2014. doi: 10.4291/wjgp.v5.i4.467
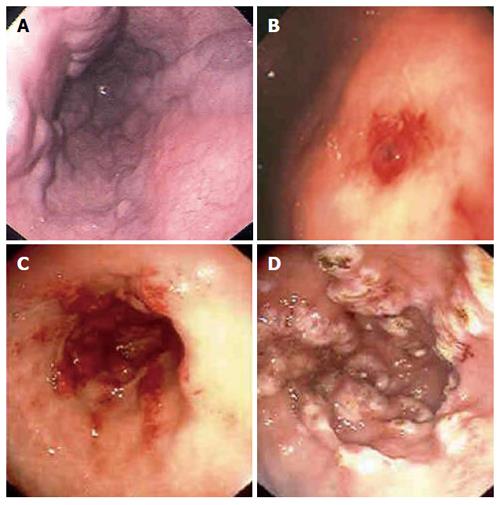
Figure 1 Upper endoscopic findings in patients with suspected upper gastrointestinal bleeding.
Esophageal varices (A), Dieulafoy’s lesion in the stomach (B), gastric antral vascular ectasia (watermelon stomach) in the antrum of the stomach pre and post argon plasma coagulation therapy (C, D).
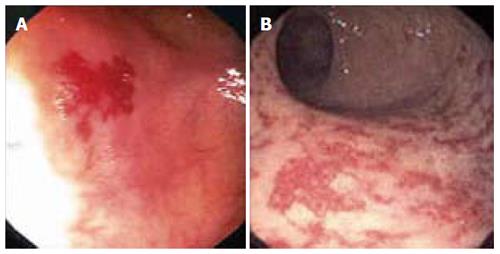
Figure 2 Colonoscopic findings in patients with suspected lower gastrointestinal bleeding.
Colonic angiodysplasia (A) and radiation proctopathy (B).
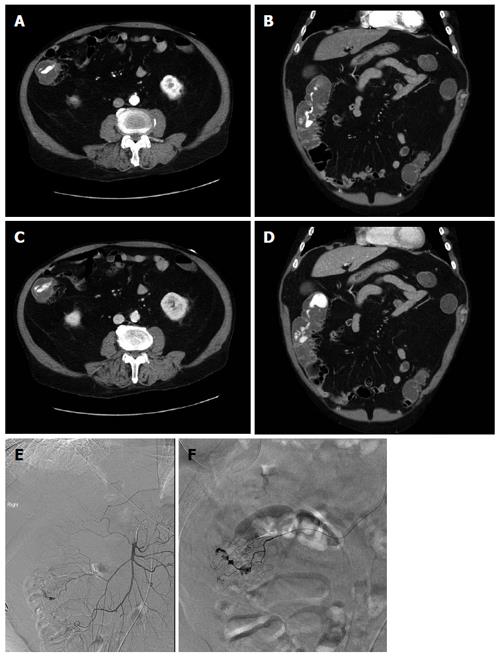
Figure 3 73-year-old man with per rectal bleeding and active gastrointestinal hemorrhage.
Contrast enhanced computed tomography (CT) angiogram images show extravasation of contrast into the lumen of the ascending colon, with pooling of contrast which increases from the arterial phase (A, B) to the delayed venous phase (C, D). Diverticula are seen arising from the medial wall of the ascending colon indicating the etiology of bleeding. Following the CT angiogram, the patient underwent catheter angiography, which demonstrated blush of contrast from the right colic branch of the superior mesenteric artery (E). Selective catheterization of the right colic artery demonstrates the bleeding focus more clearly (F). Gelfoam and coil embolization was subsequently performed.
Figure 4 Jejunal angiodysplasia as seen on capsule endoscopy.
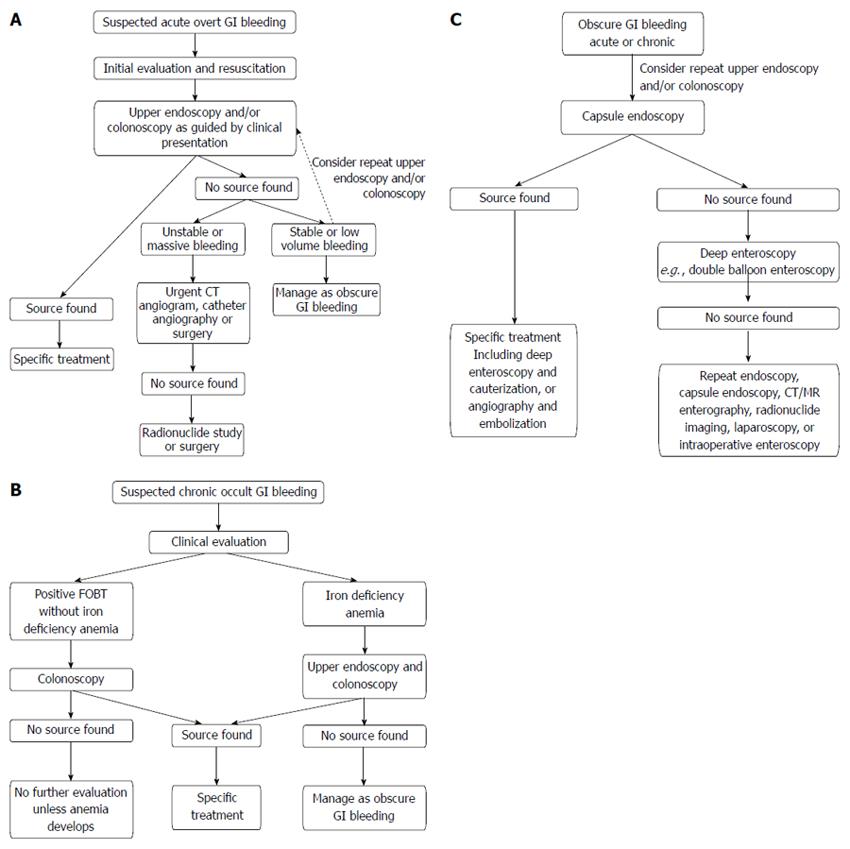
Figure 5 Diagnostic algorithms.
A: Acute overt; B: Chronic occult; C: Obscure. CT: Computed tomography; MR: Magnetic resonance; GI: Gastrointestinal; FOBT; Fecal occult blood test.
- Citation: Kim BSM, Li BT, Engel A, Samra JS, Clarke S, Norton ID, Li AE. Diagnosis of gastrointestinal bleeding: A practical guide for clinicians. World J Gastrointest Pathophysiol 2014; 5(4): 467-478
- URL: https://www.wjgnet.com/2150-5330/full/v5/i4/467.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v5.i4.467