Published online Sep 28, 2017. doi: 10.4329/wjr.v9.i9.359
Peer-review started: January 20, 2017
First decision: May 22, 2017
Revised: June 26, 2017
Accepted: July 14, 2017
Article in press: July 17, 2017
Published online: September 28, 2017
Processing time: 266 Days and 7.3 Hours
To evaluate the reliability of pronator quadratus fat pad sign to detect distal radius fracture and to predict its severity.
Retrospectively we identified 89 consecutive patients (41 female, mean age 49 ± 18 years) who had X-ray (CR) and computed tomography (CT) within 24 h following distal forearm trauma. Thickness of pronator quadratus fat pad complex (PQC) was measured using lateral views (CR) and sagittal reconstructions (CT). Pearson’s test was used to determine the correlation of the PQC thickness in CR and CT. A positive pronator quadratus sign (PQS) was defined as a PQC > 8.0 mm (female) or > 9.0 mm (male). Frykman classification was utilized to assess the severity of fractures.
Forty-four/89 patients (49%) had a distal radius fracture (Frykman I n = 3, II n = 0, III n = 10, IV n = 5, V n = 2, VI n = 2, VII n = 9, VIII n = 13). Mean thickness of the PQC thickness can reliably be measured on X-ray views and was 7.5 ± 2.8 mm in lateral views (CR), respectively 9.4 ± 3.0 mm in sagittal reconstructions (CT), resulting in a significant correlation coefficient of 0.795. A positive PQS at CR was present in 21/44 patients (48%) with distal radius fracture and in 2/45 patients (4%) without distal radius fracture, resulting in a specificity of 96% and a sensitivity of 48% for the detection of distal radius fractures. There was no correlation between thickness of the PQC and severity of distal radius fractures.
A positive PQS shows high specificity but low sensitivity for detection of distal radius fractures. The PQC thickness cannot predict the severity of distal radius fractures.
Core tip: This study evaluated reliability of pronator quadratus fat pad sign (PQS) to detect distal radius fracture and to predict its severity. Therefore correlation of measurements of pronator quadratus complex (PQC) on conventional lateral radiographs (CR) and sagittal reconstructions of computed tomographies (CT), also regarding the severity of fractures were analyzed. In conclusion PQC thickness can reliably be measured on lateral CR and correlates with CT. Sensitivity of PQS for detecting fractures is low, but specificity is high. Therefore a positive PQS in putative negative radiograph should trigger further investigations, e.g., CT scan. PQC thickness cannot predict severity of wrist fractures.
- Citation: Loesaus J, Wobbe I, Stahlberg E, Barkhausen J, Goltz JP. Reliability of the pronator quadratus fat pad sign to predict the severity of distal radius fractures. World J Radiol 2017; 9(9): 359-364
- URL: https://www.wjgnet.com/1949-8470/full/v9/i9/359.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i9.359
Soft tissue alterations or signs may be helpful when radiographs are assessed for fractures and have been used to detect occult bone injuries[1]. Regarding the wrist the “navicular fat stripe” and the “pronator quadratus sign” (PQS) have been described. Mac Ewan was first to characterize the pronator quadratus fat pad sign consisting of a radiolucent (fat containing) stripe which runs parallel to the pronator quadratus muscle covering the distal radius and ulnar (Figure 1)[1,2]. Studies on healthy subjects have shown that thickness of the pronator quadratus complex (PQC) is significantly greater in men (values up to 9 mm) than in women (values up to 8 mm) and increases with age[3,4].
In the case of a trauma to the distal radius or ulna this radiolucent stripe may be deformed or displaced, probably related to edema or hematoma within the pronator quadratus muscle[5,6]. In the majority of lateral conventional radiographs this fat pad can be identified. In the past several studies have analyzed the usefulness of the PQS to detect subtle fractures or inflammation of adjacent e in their detecting[7]. Sensitivity of the PQS measured on lateral X-rays to detect occustructures[3,4,5,7]. While earlier studies described the PQS as a useful adjunctive to detect subtle fractures[1], more recent studies, which used MRI as a reference, have found this sign to be unreliabllt distal forearm fractures has been reported to range between 26% and 65%. Specificity however has been found to be 69%-70%[4,8], indicating that absence of the PQS does not necessarily exclude an (occult) fracture, while its presence should trigger further investigations to rule out an underlying pathology. More recent data suggest that a certain muscle-to-bone ratio (maximum pronator quadratus thickness and distal radial thickness at same levels) might be a useful index for the diagnosis of non-displaced and occult distal forearm fracture[9]. Besides detection of a distal radius fracture, classification and evaluation of the injury extent play a role during work-up of extremity trauma cases. So far conventional X-ray underestimates the severity of distal radius fracture when compared to computed tomography or the intraoperative situs[10,11]. In this context the PQS has not been evaluated for predicting the severity of an underlying fracture to the distal radius up to today.
Therefore the presented study analyzes: (1) the correlation of measurements of the pronator quadratus complex on conventional lateral radiographs and sagittal reconstructions of computed tomographies; (2) the sensitivity and specificity of the PQS on conventional lateral radiographs with computed tomography as the reference; and (3) the reliability of the PQS to predict the severity of an underlying fracture.
Institutional Review Board approval (Ethic votum No. 15-097A) was granted. Between 01/2010 and 08/2013 we retrospectively identified 89 patients (41 women, 48 men, mean age 49 ± 18 years) with conventional radiographs of the wrist, who had undergone an additional computed tomography within 24 h after suffering a forearm trauma. Inclusion criteria for this study were a distal forearm trauma in patients older than 18 years who had both a conventional X-ray as well as a CT scan of the wrist within 24 h of the time of trauma. Exclusion criteria included age below 18 years, diabetic patients, patients under treatment with corticosteroid, patients with previous forearm fractures as well as musculo-skeletal (muscular dystrophy osteoporosis) and neurological disorders (polyneuropathy, multiple sclerosis).
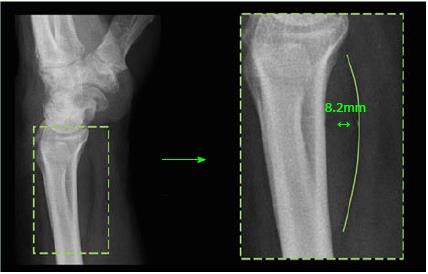
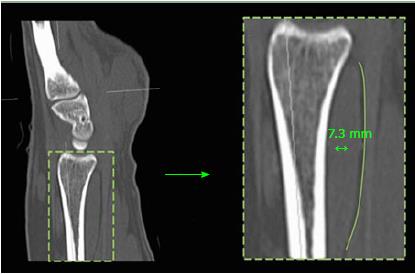
Thickness of the pronator quadratus complex was measured by two radiologists (three and eight years of experience with musculoskeletal imaging) on lateral radiographs (Figure 2) and on sagittal reconstructions of CTs (Figure 3). The thickest part of the pronator quadratus complex was identified, and the musculus pronator quadratus as well as the adjacent layer of fat were measured together. Inter-observer variability between the two readers was analyzed using Cohen’s kappa.
Correlation of measurements of the pronator quadratus complex on conventional lateral radiographs and sagittal reconstructions of computed tomographies was evaluated using the Pearson product-moment correlation coefficient. The Pearson product-moment correlation coefficient is a dimensionless parameter of the strength of the linear relationship between two variables. It can take values between -1 and +1, where +1 (or -1) is a completely positive (or negative) linear relationship between the observed values. Values at 0 indicate no linear correlation.
A (positive) pronator quadratus sign was defined if the pronator quadratus complex measured more than 8 mm in women or 9 mm in men[4]. Severity of distal radius fractures was classified using the Frykman classification[12].
For statistical analysis SPSS (Statistics 21, SPSS Inc, IBM Company) was used. Significance level was set at 0.05. Sensitivity, specificity, positive and negative predictive values for a positive fat pad sign were calculated.
Of 89 patients 44 (49%) had a distal radius fracture. Of these, 24 (55%) patients had a Colles-fracture and ten (23%) patients had a Smith-fracture. Furthermore there were four (9%) patients with dorsal Barton fracture and one (2%) patient with reversed Barton fracture. Two (5%) patients had a Chauffeur fracture and two (5%) had a compressed plurifragmentary fracture. Figures 4 and 5 highlight case examples from the analyzed patient cohort. Table 1 highlights the distribution of fractures according to the Frykman classification.
| Frykman-classification | |
| I | 3 |
| II | 0 |
| III | 10 |
| IV | 5 |
| V | 2 |
| VI | 2 |
| VII | 9 |
| VIII | 13 |
The group without fractures included 45 patients (21 female, 24 male) and served as control group. Mean age was 47.0 ± 17.5 years. One patient had an underlying malignant disease. The group with a fracture consisted of 44 patients (20 female, 24 male) with a mean age of 51.8 ± 18.2 years.
Mean thickness of the pronator quadratus complex on lateral radiographs was 7.5 ± 2.8 mm and 9.4 ± 3.0 mm on sagitally reconstructed CT respectively. Table 2 depicts measurements in patients with and without an accompanying fracture. Cohen’s kappa was used and showed an almost perfect agreement between the measurement of the two radiographs (0.887, P < 0.01).
| Total (n = 89) | With fracture | Without fracture | |
| (n = 44) | (n = 45) | ||
| CR (mm) | 7.5 ± 2.8 | 8.8 ± 2.9 | 6.2 ± 1.8 |
| CT (mm) | 9.4 ± 3.0 | 10.9 ± 3.1 | 7.8 ± 2.0 |
| Correlation | 0.795 | 0.74 | 0.695 |
| coefficient |
Regarding thickness measurements we found a significant correlation (P < 0.01) with a Pearson product-moment correlation coefficient of 0.795 between lateral radiographs and sagittal reconstructions of the CT scans.
Table 3 depicts the distribution of a normal or increased thickness (positive fad pad sign) of the pronator quadratus complex depending on the presence of a fracture (as confirmed or excluded by CT). On lateral radiographs 21/44 patients (47.7%) with a fracture had a positive fad pad sign. On the other hand we found 2/45 patients (4.4%) with a positive fad pad sign in the group without a fracture. Sensitivity and specificity were 48% and 96%, respectively. Positive and negative predictive values for detection of fracture using the fad pad sign was 91% and 65%, respectively (Tables 3 and 4). No significant correlation was found if the thickness of the pronator quadratus complex was used to determine the severity of a fracture, neither on lateral radiographs (Pearson product-moment correlation coefficient 0.038) nor on sagittal reconstructions of CT (0.006) scans.
| CR pronator quadratus fat pad sign | ||||
| Radius fracture | Positive | Negative | Total | |
| Yes | 21 | 23 | 44 | |
| No | 2 | 43 | 45 | |
| Total | 23 | 66 | 89 | |
| Sensitivity | Specificity | Positive | Negative | |
| predictive value | predictive value | |||
| Positive fat pad | 48.00% | 96.00% | 91.00% | 65.00% |
| sign for detection | ||||
| of a fracture |
Based on the results of our study we consider two messages to be of importance: A positive fat pad sign has a high specificity but low sensitivity for detection of a wrist fracture. We found no significant correlation between the thickness of the PQC and the severity of a fracture.
Early reports have suggested that a positive PQS should arouse suspicion of an occult fracture[7]. However more recent studies have reported sensitivity for the positive fat pad sign to detect an occult fracture as low as 26%-65%[4,8], judging it unreliable. One reason may be that in those studies MRI was used as reference - a method which is very sensitive for depicting bone injuries. Moreover, false negative results may be attributed to a dorsal location of the fracture which would not displace the pronator quadratus muscle, or to a poor image quality of the radiographs which do not allow evaluation of the fad pad sign and, last but not least, to a short interval between the injury and the generation of the radiographs so that the soft tissue is not swollen to such a degree that it may be detectable[1]. A recent study has suggested utilization of a muscle-to-bone ratio (maximum pronator muscle thickness divided by the maximum bone thickness of the distal radius at corresponding levels): With a ratio above 0.4 an occult distal forearm trauma seems likely and should be further evaluated[9].
For the first time, but in a setting similar to the above-mentioned studies, the presented evaluation used computed tomography scans as reference standard. CT is also known to be sensitive in detecting fractures and we too found a poor sensitivity of 46% for a positive PQS in predicting a distal radius fracture. Specificity of a positive PQS however has been calculated around 70%[4,8] and thus found to range higher than sensitivity. In our study specificity was 96%, indicating that absence of the PQS does not necessarily exclude an (occult) fracture, while presence of it should trigger further investigations to rule out an underlying pathology, as proposed by others[13].
So far correlation of the PQS on conventional X-rays and CT or MRI has not been evaluated: In this context the presented study found a significant correlation of the thickness of the pronator quadratus complex on lateral radiographs and sagittal reconstruction of CT scans of the wrist. From this one may conclude that measurements on lateral radiographs are reproducible and may therefore be used for further studies.
Radiographs in a.p. and lateral views have been used as standard and been judged to be sufficient for evaluation of wrist fractures[10]. Several classifications have been used to group wrist fractures, with AO and Frykman classification as the most common. However both classifications are unreliable regarding reproducibility[14]. Moreover it has been reported that these systems, when compared to CT or intraoperative evaluation, underestimate the severity of wrist fractures, e.g., involvement of bearing areas, which again may be associated with worse outcome for involved patients[10,11]. In this context the present study aimed at evaluation of PQS as an aid to the assessment of lateral radiographs by predicting the severity of an underlying wrist fracture. As no correlation could be found between the thickness of the PQC and the severity of the underlying fracture as assessed by Frykman classification, there seems to be no relevant role for the evaluating of the PQS in predicting the grade or severity of a wrist fracture.
There are main limitations to this study. First, the sample size is small, which prevents us from generalizing on the basis of the results of our series. Second, this study is retrospective and lacks randomization. Therefore a patient selection bias may have played a role. Third, true lateral radiographs of the distal radius might be hard to achieve constantly throughout a study collective and this circumstance might therefore be a slight source of error.
In conclusion, there is a strong correlation of measurements of the pronator quadratus complex on lateral radiographs and sagittal reconstructions from computed tomography scans. Sensitivity of the PQS for detecting wrist fractures is low, but specificity is high. Therefore a positive PQS in a putative negative radiograph should trigger further investigations, e.g., a CT scan. The thickness of the PQC does not correlate with the severity of wrist fractures.
Conventional radiography is a fast, easy and feasible diagnostic tool to detect fractures. Indirect fracture signs which can be detected on conventional X-ray studies play their role in the detection of occult bone injuries, and might trigger further investigations as, e.g., a computed tomography (CT) scan. The present study evaluates the reliability of such an indirect sign, namely the pronator quadratus fat pad sign, for the detection of distal radius fractures and prediction of its severity.
The main conclusion of the present study is that a positive pronator quadratus sign (PQS) shows high specificity but low sensitivity for detection of distal radius fractures and that the Pronator quadratus complex (PQC) thickness cannot predict the severity of distal radius fractures. However, there are main limitations to this study. First, the sample size is small, which prevents us from generalizing on the basis of the results of our series. Second, this study is retrospective and lacks randomization. Therefore a patient selection bias may have played a role.
For the first time, but in a setting similar to other studies, the presented evaluation used computed tomography scans as reference standard. When compared to other studies we too found a poor sensitivity of 46% for a positive PQS in predicting a distal radius fracture. In this study specificity was 96%, indicating that absence of the PQS does not necessarily exclude an (occult) fracture, while presence of it should trigger further investigations to rule out an underlying pathology, as proposed by other articles. However configuration of the PQS does not give any information on the severity of an underlying fracture.
There is a strong correlation of measurements of the pronator quadratus complex on lateral radiographs and sagittal reconstructions from computed tomography scans. It can therefore be reliably used for further research purposes regarding this topic. Sensitivity of the PQS for detecting wrist fractures is low, but specificity is high. Therefore a positive PQS in a putative negative radiograph should trigger further investigations, e.g., a CT scan. A certain thickness of the PQS cannot help to adjudicate the severity of the underlying fracture.
There are two terms which are important for a clear understanding of this article. First, this study pays attention to the PQC, which consists of the pronator quadratus muscle covering the distal radius and ulnar and can be identified on the lateral view of the wrist and a radiolucent (fat containing) stripe, which runs parallel to the pronator quadratus muscle. Second, the authors analyzed a positive (and negative) PQS. A positive pronator quadratus sign is defined as thickness of the pronator quadratus complex above 9 mm in men and below 8 mm in women.
It is very interesting study which investigated the relationship between pronator quadratus fat pad sign and distal radius fractures.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Liu JY, Zhang L S- Editor: Ji FF L- Editor: A E- Editor: Zhao LM
| 1. | Zimmers TE. Fat plane radiological signs in wrist and elbow trauma. Am J Emerg Med. 1984;2:526-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Macewan DW. Changes due to trauma in the fat plane overlying the pronator quadratus muscle: a radiologic sign. Radiology. 1964;82:879-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Zammit-Maempel I, Bisset RA, Morris J, Forbes WS. The value of soft tissue signs in wrist trauma. Clin Radiol. 1988;39:664-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Fallahi F, Jafari H, Jefferson G, Jennings P, Read R. Explorative study of the sensitivity and specificity of the pronator quadratus fat pad sign as a predictor of subtle wrist fractures. Skeletal Radiol. 2013;42:249-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Sasaki Y, Sugioka Y. The pronator quadratus sign: its classification and diagnostic usefulness for injury and inflammation of the wrist. J Hand Surg Br. 1989;14:80-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Sato J, Ishii Y, Noguchi H, Takeda M, Toyabe S. Sonographic appearance of the pronator quadratus muscle in healthy volunteers. J Ultrasound Med. 2014;33:111-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Curtis DJ, Downey EF Jr, Brower AC, Cruess DF, Herrington WT, Ghaed N. Importance of soft-tissue evaluation in hand and wrist trauma: statistical evaluation. AJR Am J Roentgenol. 1984;142:781-788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Annamalai G, Raby N. Scaphoid and pronator fat stripes are unreliable soft tissue signs in the detection of radiographically occult fractures. Clin Radiol. 2003;58:798-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Sun B, Zhang D, Gong W, Huang S, Luan Q, Yang J, Wang D, Tian J. Diagnostic value of the radiographic muscle-to-bone thickness ratio between the pronator quadratus and the distal radius at the same level in undisplaced distal forearm fracture. Eur J Radiol. 2016;85:452-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Metz VM, Gilula LA. Imaging techniques for distal radius fractures and related injuries. Orthop Clin North Am. 1993;24:217-228. [PubMed] [Cited in This Article: ] |
| 11. | Dahlen HC, Franck WM, Sabauri G, Amlang M, Zwipp H. [Incorrect classification of extra-articular distal radius fractures by conventional X-rays. Comparison between biplanar radiologic diagnostics and CT assessment of fracture morphology]. Unfallchirurg. 2004;107:491-498. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Frykman G. Fracture of the distal radius including sequelae--shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand. 1967;Suppl 108:1-153. [PubMed] [Cited in This Article: ] |
| 13. | Moosikasuwan JB. The pronator quadratus sign. Radiology. 2007;244:927-928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Illarramendi A, González Della Valle A, Segal E, De Carli P, Maignon G, Gallucci G. Evaluation of simplified Frykman and AO classifications of fractures of the distal radius. Assessment of interobserver and intraobserver agreement. Int Orthop. 1998;22:111-115. [PubMed] [Cited in This Article: ] |