Published online Dec 28, 2017. doi: 10.4329/wjr.v9.i12.426
Peer-review started: July 20, 2017
First decision: August 4, 2017
Revised: August 11, 2017
Accepted: September 3, 2017
Article in press: September 3, 2017
Published online: December 28, 2017
Acute pulmonary embolism (PE) is the third most common cause of death in hospitalized patients. The development of sophisticated diagnostic and therapeutic modalities for PE, including endovascular therapy, affords a certain level of complexity to the treatment of patients with this important clinical entity. Furthermore, the lack of level I evidence for the safety and effectiveness of catheter directed therapy brings controversy to a promising treatment approach. In this review paper, we discuss the pathophysiology and clinical presentation of PE, review the medical and surgical treatment of the condition, and describe in detail the tools that are available for the endovascular therapy of PE, including mechanical thrombectomy, suction thrombectomy, and fibrinolytic therapy. We also review the literature available to date on these methods, and describe the function of the Pulmonary Embolism Response Team.
Core tip: Endovascular treatment of pulmonary embolism (PE) represents several methods of minimally invasive therapy of this important clinical entity, including mechanical thrombectomy, suction thrombectomy, and fibrinolytic therapy. With this paper, we hope to provide a detailed review of these methods, which is critical to understanding the tools that are available to the clinician for the treatment of PE.
- Citation: Nosher JL, Patel A, Jagpal S, Gribbin C, Gendel V. Endovascular treatment of pulmonary embolism: Selective review of available techniques. World J Radiol 2017; 9(12): 426-437
- URL: https://www.wjgnet.com/1949-8470/full/v9/i12/426.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i12.426
Acute pulmonary embolism (PE) is the third most common cause of death in hospitalized patients[1]. The development of sophisticated diagnostic and therapeutic modalities for PE, including medical and surgical treatment as well as newly developed endovascular therapy, affords a certain level of complexity to the treatment of patients with this important clinical entity.
PE, by definition, involves emboli to the pulmonary arterial circulation, which can induce acute pulmonary arterial hypertension, right heart strain, and in some patients, right ventricular infarction[2]. Angiographic studies have demonstrated that pulmonary artery pressures increase when the embolic load occludes more than 30%-50% of the cross sectional area of the pulmonary arterial bed[3]. Clot burden alone does not determine the degree of pulmonary hypertension. The disruption of the alveolar capillary membrane by thrombus results in disruption of the diffusion of oxygen, with subsequent decreased oxygen binding to hemoglobin. Both hypoxia and the release of vasoconstrictors precipitate vasoconstriction of the pulmonary circulation, which contributes to the acute development of pulmonary hypertension[4]. This pulmonary hypertension leads to right ventricular dilatation and subsequent right ventricular failure. Underlying cardiopulmonary disease influences the ability of the right heart to adapt to increased pulmonary artery pressure.
The majority of pulmonary emboli are clinically silent. This is due to the dual blood supply of the lung through the bronchial and pulmonary arteries, as well as the fact that most emboli to the lung are small and resolve before the manifestation of any physical signs and symptoms. The clinical presentation of PE depends upon its severity, which tends to vary widely. Patients with PE can range from being completely asymptomatic to presenting with cardiovascular collapse[5]. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II (PIOPED II) study, the most commonly occurring complaints in patients with PE were sudden onset dyspnea, pleuritic chest pain, cough, orthopnea, calf/thigh pain with associated swelling, erythema, edema, tenderness and palpable cords, wheezing, and hemoptysis[6]. On physical exam, the most common presenting signs were tachypnea and tachycardia. Less commonly seen, but still significant, were rales, decreased breath sounds, an accentuated pulmonic component of the second heart sound, jugular venous distension, and fever. Patients with massive PE may present with acute right ventricular failure leading to increased jugular venous pressure, a right-sided third heart sound, parasternal lift, cyanosis, hypotension, and shock[7,8].
Cardiovascular collapse is the product of a large sized or saddle embolus, and therefore an uncommon presenting sign, given that most pulmonary emboli are small. It should still be noted, however, that in patients with comorbid severe pulmonary hypertension who suffer a small PE, entry into shock is still a strong possibility[7,8]. Syncope is a less common but clinically significant initial presenting sign of PE that occurs in approximately 10% of patients[9]. As PE causes a ventilation/perfusion (V/Q) mismatch, patients present with hypoxemia that results in hyperventilation, and ultimately hypocapnia, which leads to respiratory alkalosis. These findings, along with a widened alveolar-arterial oxygen gradient, are the most common findings on arterial blood gas analysis. Electrocardiographic abnormalities include nonspecific ST segment or T wave changes[10]. On chest radiography, parenchymal abnormality may be found[10]; however, cardiomegaly is the most common radiographic abnormality associated with acute PE[11]. Myocardial stretching, a marker of increased pulmonary pressures can be detected in the serum via elevated troponin and pro-BNP levels and are markers for increased risk of right heart failure and potentially right ventricular infarct[12].
Of the 80% of patients with PE who are normotensive, it is estimated that 27%-55% have echocardiographic evidence of RV dysfunction[13,14]. Normotensive patients with RV dysfunction have an increased risk of death from PE and recurrent PE[14]. The impact of RV dysfunction on mortality has been demonstrated in two multi-center registries. In the International Cooperative Pulmonary Embolism registry of 2454 patients with PE in the normotensive group with RV hypokinesis, the all-cause mortality was doubled at 3 mo[15]. In the Management Strategy and Prognosis of Pulmonary Embolism Registry, normotensive patients with RV dysfunction had an in-hospital mortality of 7.1% and a rate of recurrent PE of 14%[16].
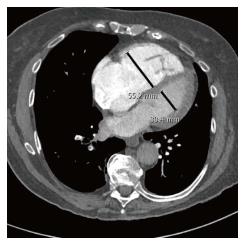
The current mainstays in the imaging diagnosis of PE are computed tomographic pulmonary angiography (CTPA) and echocardiography, which aid in determining the significance of PE on right ventricular function. Historically, the diagnosis was often made by ventilation/perfusion nuclear medicine scans, which is still employed for patients who cannot receive iodinated contrast material. Catheter based pulmonary angiography, the “gold standard” for the diagnosis of PE, has been supplanted by CTPA and is now performed almost exclusively only prior to a catheter based intervention. Depending on the institution, patients with suspected PE who present in shock or are severely ill may be first evaluated with echocardiography in the emergency room. Evidence of right ventricular dysfunction, such as paradoxical septal bowing or an elevated right ventricle to left ventricle ratio (RV/LV) may then be triaged rapidly for CTPA or, if the diagnosis is sufficiently strong clinically and the patient is unstable, straight for angiography and intervention. In these patients, echocardiography may also disclose the presence of free floating clot in the right heart which, if available, may indicate surgical or large bore catheter intervention. More commonly, patients who are more stable will first be evaluated with CTPA. This, along with troponin and pro-BNP assays, permits assignment of patients to massive, submassive or low risk categories of PE. In addition to demonstrating the extent and distribution of PE, the CTPA can provide a sufficient indication of RV dysfunction, in the absence of echocardiography. Signs of RV dysfunction on CTPA include an elevated RV/LV ratio (generally shown to be > 0.9), septal bowing and reflux of contrast into the hepatic veins (Figure 1).
The American Heart Association (AHA) divides PE into three categories: Massive PE, submassive PE, and low risk PE[12]. Massive PE is defined as acute PE with sustained hypotension (systolic BP < 90 mmHg for at least 15 min or requiring inotropic support), pulselessness, or persistent profound bradycardia (heart rate < 40 beats per minute with signs or symptoms of shock). Submassive PE presents with signs of right ventricular dysfunction including right ventricular dilatation on chest CTA (Figure 1), echocardiographic signs of right ventricular (RV) dysfunction, and/or serum markers consistent with myocardial stretching such as troponin and pro-BNP. Low risk PE shows no signs of RV dysfunction or biomarker evidence of strain[12]. Current treatment recommendations are for full anticoagulation for all three categories of PE, with thrombolysis for massive PE and to be considered in submassive PE[12]. Class III, Level B evidence recommends against fibrinolysis for low risk PE[12]. Cathether embolectomy and fragmentation or surgical embolectomy are alternatives for patients with massive PE with a contraindication for fibrinolysis[12]. In general, mechanical embolectomy should be reserved for main and lobar pulmonary arterial branches[12].
Organization of pulmonary emboli begins with adherence of clot to the vessel wall and the formation of a thin lining of endothelial cells over its surface, followed by ingrowth of cells from the intima media and capillary buds into the thrombus[17]. Serial imaging has demonstrated that reduction in amount of thrombus is 10% after 24 h, 40% after 7 d, and 50% after 2 to 4 wk[18]. Complete resolution is likely achieved in 70%-85% of patients at 6 to 12 mo after initial PE diagnosis[19]. The resolution of thrombi appears to plateau after 3 mo of adequate treatment, and only small amounts of improvement are seen after that time[20]. This forms the basis of recommendations for anticoagulation for 6 mo.
Unresolved thrombi can result in persistent perfusion defects and subsequently lead to chronic thromboembolic pulmonary hypertension (CTEPH). CTEPH following 3 mo of effective anticoagulatioin is defined by: (1) invasively measured mean pulmonary artery pressure > 25 mmHg with a pulmonary capillary wedge pressure < 15 mmHg; and (2) at least one segmental perfusion defect[21]. Patients with PE can have residual symptoms of reduced functional status, persistent thrombi, limitations of cardiopulmonary function, and CTEPH. The incidence of CTEPH is low, seen in 3.1% of patients at 1 year and in 3.8% of patients at 2 years in a cohort of 223 patients with confirmed PE, as reported by Pengo et al[22]. Although patients with CTEPH are a very small component of the total PE population, they unfortunately have the most functional impairment, and pulmonary endarterectomy and PAH Group 1 therapies are often discussed in this population[12].
Several surgical treatment options are available for the management of PE. Historically, surgical pulmonary embolectomy has been indicated in patients who are hemodynamically unstable secondary to acute massive PE. Candidates for surgical embolectomy have failed or are not candidates for thrombolytic therapy. Surgical pulmonary embolectomy is also recommended for patients with persistent hemodynamic instability, or in patients with RV dysfunction that persists despite the use of fibrinolytic therapy[23]. There are reports in which surgical embolectomy is shown to be superior in the long term compared to thrombolysis in hemodynamically comparable patients. In a 2006 study by Meneveau et al[24], 488 patients with PE underwent thrombolysis, 40 of whom did not respond to the therapy. Of these 40 patients failing thrombolytic therapy, 14 patients were treated by rescue surgical embolectomy, and 26 were treated by repeat thrombolysis. Ultimately, rescue surgical embolectomy led to a better in-hospital course when compared with repeat thrombolysis in patients with massive PE who did not respond to thrombolysis[24]. In experienced centers, surgical embolectomy is considered to be a safe procedure with low mortality, providing improved postoperative right ventricular function and pulmonary pressure as well as improved long-term outcome[25]. In a study of 37 consecutive cases, Edelman et al[25] demonstrated that elimination of a large portion of the clot burden could be life-saving. They concluded that pulmonary embolectomy should be considered as an initial treatment strategy in patients with massive or submassive pulmonary embolus with a large burden of proximal clot[25].
Catheter directed therapy of PE includes mechanical thrombectomy/fragmentation, mechanical thrombectomy plus thrombolytic therapy, and catheter delivered thrombolytic therapy. The goal of catheter directed therapy is to decrease afterload on the right ventricle while reducing clot burden and long-term sequelae of CTEPH. Displacement of centrally occlusive thrombus to a more peripheral distribution in pulmonary arterial branches may decrease afterload in the right ventricle but may not address clot burden. We will not attempt to discuss all devices but limit discussion to the devices most reported for use in the pulmonary arteries. Given the large number of existing devices, it is clear that an ideal device is not currently available.
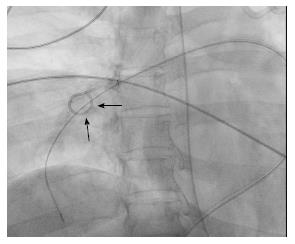
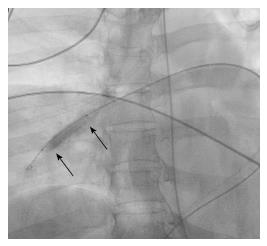
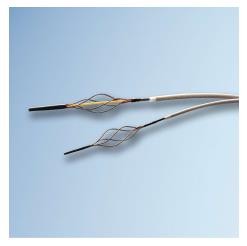
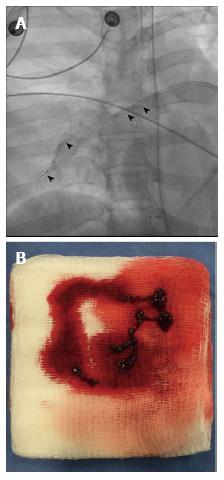
Purely mechanical approaches to central pulmonary emboli include clot fragmentation, fragmentation with aspiration, and rheolytic thrombectomy[26,27]. Clot fragmentation has been achieved with procedures as simple as rotation of a pigtail catheter within the thrombus either manually or with mechanical assistance (Figure 2). Angioplasty balloons inflated within clot provide an alternative approach to fragmentation (Figure 3). Other mechanical devices such as the Trerotola Mechanical Thrombectomy Device (Teleflex Inc., Wayne, PA, United States) designed for use in thrombosed dialysis grafts have been used in the pulmonary arteries with mixed results (Figure 4).
There are several rheolytic thrombectomy devices, which have been used off label in the pulmonary arteries. The Amplatz thrombectomy device (Microvena, White Bear Lake, MN) is a 6-French catheter that incorporates a high-pressure air-driven high-speed impeller, creating a vacuum vortex-pulling clot into the distal tip of the catheter, fragmenting the thrombus, then expelling particles, most of which measure 50 μm or less[26,27].
The Angiojet catheter (Boston Scientific, Marlborough, MA, United States) is one of the most frequently used devices, which provides both clot fragmentation and aspiration of clot fragments. Saline jets directed into the clot at the distal end of the catheter result in clot fragmentation. These jets may also be used to distribute thrombolytic agents into the clot in the “power pulse mode”. At the same time, aspiration of clot fragments is achieved at catheter sideports from high velocity saline looping back into a second lumen creating a Venturi effect (Figure 5). These procedures displace obstructive emboli from a central location into the larger volume peripheral pulmonary arterial vasculature, resulting in reduction of pulmonary artery pressure and afterload on the right heart[28]. Frequently, mechanical approaches are combined with infusion systems delivering low dose thrombolytics into residual thrombus.
Suction thrombectomy was one of the earliest approaches to transcatheter treatment of pulmonary emboli, introduced by Greenfield, using a 12-French catheter with a cup on its distal end. Suction was applied to the catheter hub with a large volume syringe. A portion of thrombus was engaged in the cup and removed along with trailing adherent thrombus through a large diameter vascular sheath in either the femoral or jugular veins.
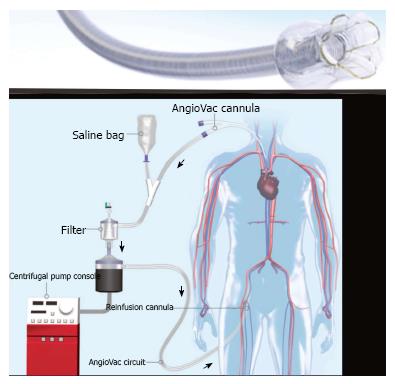
More recent approaches involve aspiration of thrombus into the lumen of an aspiration catheter of varying diameters with discharge into an aspiration container. The Angiovac system (Angiodynamics Inc., Latham, NY) consists of a 22-French coil reinforced cannula with a balloon actuated expandable funnel-shaped distal tip. The catheter is part of a veno-venous recirculation system with aspirated thrombus and blood separated and returned to the patient through a large central venous return cannula (Figure 6). The system requires a perfusionist to be present during the procedure and the added time required to assemble this team.
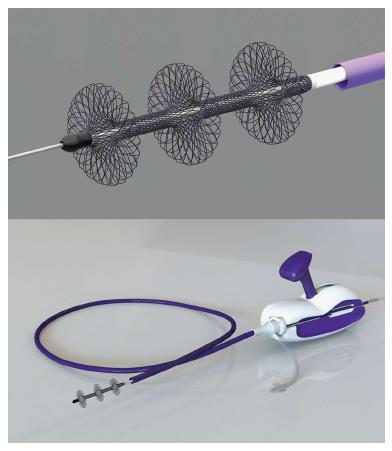
An alternative large lumen suction device is the FlowTriever system (Inari Medical, Irvine, CA, United States), in which a large bore (20-French) sheath is introduced for placement of suction catheter, which is connected to a retraction aspirator, providing a vacuum for clot aspiration. Blood admixed with clot does not have a means to return to the circulation (Figure 7). The advantage of the large bore catheters is the ability to remove large volumes of thrombus rapidly; however, their size and rigidity makes access to pulmonary artery branches more difficult. In addition, stiffness increases the possibility of injury to the heart or to the pulmonary artery.
The Penumbra system (Penumbra Inc., Alameda, CA, United States) is a suction aspiration system first used in the endovascular treatment of stroke. The Penumbra INDIGO CAT 8 system is a flexible 8-French aspiration catheter, which is connected to a continuous suction vacuum system. A wire separator in the catheter lumen facilitates clot retrieval (Figure 8). As with the FlowTriever device, the Penumbra lacks a means to return blood to the patient and can lead to significant blood loss if not embedded in clot. None of the suction systems is FDA approved in the United States for the treatment of PE, and their use is considered “off label”. The FlowTriever system has received approval from the FDA for the FLARE IDE clinical trial for patients with submassive pulmonary emboli and is currently recruiting.
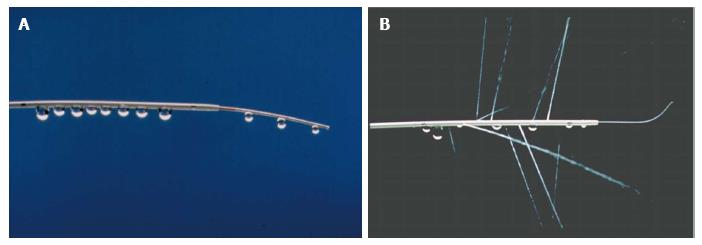
Fibrinolysis is most effective when the agent is delivered directly into the thrombus. There are several catheter systems available for delivery of fibrinolytic agents directly into the thrombus. The Unifuse infusion system (Angiodynamics, Latham, NY, United States) consists of a multi-hole catheter with an end hole and side holes distributed in variable lengths along the distal catheter. Their distribution is defined by radiopaque markers. The catheter is introduced over a standard guidewire. Following desired placement in the clot, an occluding ball guide wire is introduced to obstruct the end hole, thereby forcing the infusate out the side holes. This catheter can be used to simply infuse or pulse spray fibrinolytics by forcible injection at the catheter hub (Figure 9).
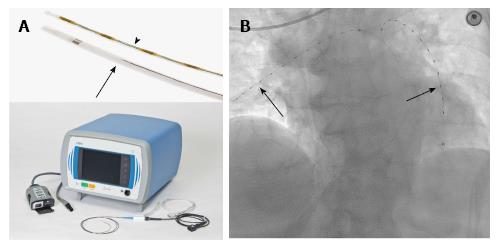
Ultrasound assisted infusion of thrombolytics through the Ekos system (Ekos Corp., Bothel, WA, United States) utilizes an ultrasonic core to generate an acoustic field dispersing the fibrinolytic agent into the clot. In addition, this acoustic field is felt to disaggregate thrombus with separation of fibrin crosslinks, accelerating clot lysis. The system consists of a 5.4-French infusion catheter with markers delineating the active area, an ultrasound core transducer, and a control unit. The catheter has both a drug delivery lumen and a central coolant channel (Figure 10).
In spite of greater than 30 years of experience with catheter directed therapy for acute PE, controversy still exists as to its precise role. This is primarily related to the lack of level I evidence of its safety and effectiveness. Most evidence is based on small non-controlled cohort studies with non-consecutive recruitment and varying criteria for success (Table 1).
| Treatment method | Type of device | No. of patients | Outcomes |
| Suction thrombectomy | Greenfield suction embolectomy catheter | n = 46[32] 33 with massive PE 4 with submassive PE 9 with chronic PE | Mean PAP reduction from 32 to 24 mmHg in 31 patients |
| Angiovac | n = 5[34] 4 with massive PE 1 with submassive PE | Technical success in 2 of the 4 patients with massive PE | |
| Flowtriever | n = 1[35] | Procedure successful | |
| Flowtriever | FLARE trial - ongoing | pending | |
| Penumbra | None | None | |
| Mechanical thrombectomy | Amplatz thrombectomy device | n = 9[36] (5 were treated with tPA) | Reduction of Miller index from 18 to 11 Mean PAP reduction from 57 to 55 mmHg Addition of tPA achieved further mean PAP reduction to 39 mmHg |
| Angiojet | n = 15[37] 10 were treated with tPA | 9 patients - significant clot resolution 5 patients - moderate clot resolution 1 patient - minimal clot resolution | |
| Angiojet | n = 51[38] 22 patients - massive PE 29 patients - submassive PE | 92% technical success Mean reduction of Miller index by 51% | |
| Catheter directed fibrinolysis | USAT | n = 59[47] (ULTIMA trial) 29 patients - UFH alone 30 patients - unfractionated heparin + USAT | Greater mean decrease of RV/LV ratio in the UFH + USAT group vs UFH alone (0.30 vs 0.03) |
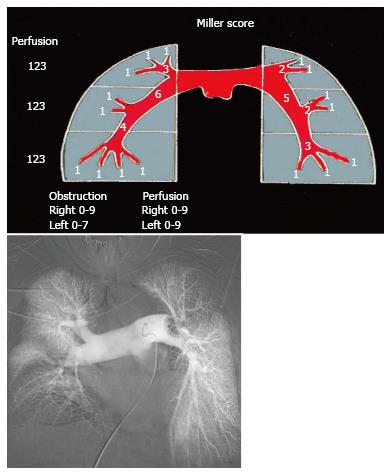
Any review of results of studies dealing with PE treatment should begin with a brief explanation of the Miller score, which is one of several scoring systems that attempt to objectively quantify the magnitude of PE (Figure 11). Described in 1975[29] and based on pulmonary arteriography it is the sum of obstruction and perfusion scores. The obstruction index divides the lung into nine segments on the right and seven on the left. Thrombus in any segment is given a score of 1. Thrombus proximal to segmental branches is given a score of the number of branches peripheral to the thrombus (i.e., right lower lobe pulmonary artery = 4, saddle embolus = 16). The perfusion index divides each lung into upper, middle and lower zones scored as no perfusion (3), severely reduced perfusion (2), mildly reduced perfusion (1), and normal perfusion (0). Therefore the worst Miller index combining obstruction and perfusion is 34.
The earliest reports were those describing suction embolectomy with the Greenfield suction embolectomy catheter. Greenfield reported 46 patients treated with the 12-French suction catheter[30]. Of these patients, 33 had sustained massive pulmonary emboli, 4 submassive, and 9 chronic. Mean pulmonary arterial pressure was reduced from 32 to 24 mmHg in 31 patients, in whom it was measured with clinical success in 36/46 patients. After the adoption of prophylactic inferior vena cava (IVC) filters following the procedure, the 30 d survival increased from 50% in the first 10 patients to 70% in the subsequent 36 patients. Because of the size and difficulty of placement of the Greenfield suction embolectomy catheter, the device fell out of favor.
Currently, two large bore aspiration catheters are available. The Angiovac system, approved for use in treating thrombi in the venous system, is being used off-label in the pulmonary arteries. There have been case reports and small series reporting the use of this device with mixed results[31]. A retrospective review of five consecutive patients in whom the Angiovac was used included four patients with massive PE and one with submassive PE[32]. Technical success, defined as successful removal of some thrombus combined with reduction of the Miller score by greater than or equal to 5 was achieved in two of the four patients with massive PE. Four patients died at a mean of 7.3 d, all having presented with massive PE. One death was related to catheter perforation of the right ventricular free wall. In another small series of three patients in whom thrombectomy of the pulmonary arteries was attempted, the procedure was unsuccessful in two of the three patients. Lack of success was attributed to size, stiffness and lack of maneuverability of the device.
There is even less information on the use of the FlowTriever device in the pulmonary arteries. A single case of success in a saddle embolus in the pulmonary artery was recently reported[33]. It is uncertain if similar problems with stiffness and lack of maneuverability are encountered with this device. The FlowTriever FLARE trial will help clarify these issues in a larger cohort of patients. Unfortunately this trial excludes patients with massive PE - a group of patients in whom suction embolectomy is most appropriate.
The Penumbra device is another suction device currently available in an 8-French system, providing the flexibility for placement in segmental branches of the pulmonary artery. However, luminal diameter limits the volume of clot aspirated. There is no evidence available at the current time to support its use.
The Amplatz thrombectomy device has been used in the pulmonary arteries and reported about in small series. A report by Muller-Hulsbeck included 9 patients, out of which, 5 were treated with additional tPA[34]. Miller index was reduced from 18 to 11. Of interest, the mean pulmonary arterial pressure was reduced from 57 to 55 mmHg after mechanical thrombectomy. The addition of fibrinolytic therapy achieved further reduction of mean pulmonary arterial pressure to 39 mmHg, raising question of the value of the mechanical component of the procedure.
The Angiojet device is the most studied rheolytic thrombectomy device. A study by Nassiri et al[35] reviewed experience with 15 consecutive patients, one with massive and 14 with submassive pulmonary emboli. Adjunctive tPA was administered in 10 patients. Completion angiography was used to assess success. Significant clot resolution (> 75%) was observed in 9 patients, moderate (50%-75%) in 5 patients, and minimal (< 50%) in 1 patient. All patients receiving adjunctive tPA had significant or moderate clot resolution. There were no in-hospital deaths or recurrent pulmonary emboli. Two patients had post procedural renal failure and there was one case of cardiopulmonary arrest.
Chechi retrospectively reviewed 51 patients presenting with massive (in 22 patients) or submassive (in 29 patients) pulmonary emboli[36]. Technical success determined by angiography was achieved in 92% of cases, with mean reduction of the Miller index by 51%. Adjunctive fibrinolytic therapy was performed in 21% of patients. The in-hospital mortality was 42% in patients presenting with shock, 12% in patients with hypotension, and 3.4% in patients with submassive pulmonary emboli. Renal failure was reported in 24% of patients, while bradycardia requiring transvenous pacing was reported in 8%.
Systemic complications of renal insufficiency, bradycardia, and asystole are frequently reported with the Angiojet device. Both complications stem from red blood cell destruction leading to the release of adenosine, causing bradycardia and asystole. Some operators limit activation of the device to five-second intervals, separating the intervals to limit the amount of adenosine in the circulation. Renal insufficiency is felt to result from hemoglobinuria and resultant acute tubular necrosis. Aggressive hydration and administration of bicarbonate to raise urine pH to above 6.5 may diminish the tubular toxicity of hemoglobin[37].
Patients with massive PE who have failed systemic thrombolysis, have absolute contraindications to thrombolysis, or cannot await the two hour time interval for administration of systemic thrombolytics are clearly candidates for either catheter directed therapy or surgical thrombo-embolectomy. Unfortunately few centers are equipped for urgent surgical thrombo-embolectomy and few will achieve the survival outcomes of centers with expertise in pulmonary thrombo-embolectomy.
A meta-analysis of catheter directed treatment of PE by Tafur[38] included 24 studies, enrolling 700 patients, of who 653 received endovascular treatment. Pooled data estimated risk of death in non-ultrasound assisted thrombolysis (USAT) studies at 9% and 4% in the USAT group. In studies using risk stratification, the Miller index decreased from 19.4 to 9.9 following intervention. In studies including pulmonary artery pressures, mean pressures were reduced from 57 to 36 mmHg. The main safety outcome of major bleeding was 4% in the USAT studies and 10% in the non-USAT group.
A review of data of a nationwide inpatient sample of 72230 patients with PE who were considered unstable reported a case fatality rate of 47% in patients not receiving thrombolytic therapy and 15% in patients receiving thrombolytics. However 70% of these patients were denied thrombolytics for various reasons[39]. Given this data randomization of patients with massive PE and contraindications to systemic thrombolysis to catheter directed intervention vs no therapy raises both ethical concerns and recruitment challenges and is unlikely to occur.
There is evidence supporting the use of catheter directed therapy in patients with massive PE. A meta-analysis of catheter directed therapy in 2009[40] identified a subset 594 patients from 35 uncontrolled studies treated for massive PE defined by hypotension. Clinical success was determined by stabilization of hemodynamics, resolution of hypoxia, and survival. Ninety six percent of patients did not receive thrombolytics before catheter directed therapy. Thirty three percent of patients received mechanical thrombectomy alone, while 60%-67% received both mechanical thrombectomy and pharmacologic thrombolysis. Mechanical technique most often used was pigtail catheter fragmentation in 69% of patients; used alone in 53%. Clinical success was achieved in 86.5% of patients. Clinical success was higher in studies in which patients received catheter directed thrombolytic therapy compared to those in which thrombolytic was less frequently given. The pooled risk of minor complications was 7.9% and major complication 2.4%. Of interest, five procedural related deaths were all associated with use of the Angiojet device.
Given the fatality rate that approaches 50%, as reported for untreated patients with massive PE, and subset analysis of catheter directed therapy in patients with massive PE reporting mortality rates as low as 15%, this therapy appears to be appropriate. Since many if not most of these patients had received both mechanical as well as pharmaco-mechanical treatment, it is therefore difficult to predict the effectiveness of mechanical thrombo-dispersion-thrombectomy alone. Certainly the next generation of thrombectomy devices will facilitate access to the main pulmonary arteries and segmental branches, improving the efficacy of mechanical thrombectomy. Currently, there is no data supporting the addition of catheter directed therapy to systemic therapy for patients who have responded to systemic therapy in spite of its ability to further decrease clot burden and the sequelae of CTEPH.
For patients with submassive PE, there is controversy as to the role of both systemic or catheter directed therapy. A meta-analysis of randomized controlled trials comparing systemic thrombolytic therapy with heparin alone in patients with PE showed a benefit only in patients with massive PE[41]. In contrast, the MAPPET-3 trial[42] randomized 256 patients with sub-massive PE into heparin plus tPA (118 patients) vs heparin plus placebo (138 patients). The primary endpoint of in hospital mortality or clinical deterioration requiring an escalation of treatment was significantly higher in the heparin plus placebo group primarily due to the need for treatment escalation (26% vs 10%). Mortality in both groups was low: 3.4% in the heparin plus tPA group and 2.2% in the heparin plus placebo group. No fatal or intracranial hemorrhage was observed.
The PEITHO trial[43] randomized 1006 patients with submassive PE to systemic tenecteplase (30-50 mg) as a single bolus or placebo with both groups receiving intravenous heparin. The primary endpoints were death, hemodynamic decompensation, confirmed recurrent PE within 7 d, death within 30 d, and major adverse events within 30 d. Death or hemodynamic decompensation occurred in 2.6% of patients in the tenecteplase group and in 5.6% in the placebo group (P = 0.02). Extracranial bleeding occurred in 6.3% of the tenecteplase group and in 1.2% of the placebo group (P ≤ 0.001). Stroke occurred in 2.4% of the tenecteplase group and in 0.2% of the placebo group. At 30 d, the mortality was 2.4% and 3.2% in the tenecteplase and placebo groups, respectively. Thrombolytic therapy decreased the need for escalation of care with no difference in mortality but at the expense of increased bleeding complications including hemorrhagic stroke.
The MOPETT trial[44] randomized 121 patients with moderate PE to receive a “safe dose” of systemic thrombolytic (50 mg tPA) in 61 patients or anticoagulation alone in 60 patients. The primary end point was pulmonary hypertension and composite endpoints of pulmonary hypertension and recurrent PE at 28 mo. Secondary endpoints included total mortality, duration of hospital stay, and bleeding during hospitalization. Pulmonary hypertension and the composite endpoint of pulmonary hypertension and recurrent PE occurred in 16% of the thrombolytic group and in 57% of the control group (P ≤ 0.001). Death and recurrent PE occurred in 1.6% and 10% of the tPA and control groups respectively. There was no major bleeding in either group. When death or recurrent PE were assessed independently there was no difference between the groups. There have been numerous papers published on the delivery of fibrinolytic agents through infusion catheters placed directly into pulmonary artery thrombus. The most compelling evidence for the effectiveness of catheter directed treatment of PE comes from the ULTIMA trial[45]. In this prospective randomized trial, USAT was compared to heparin alone in patients with submassive PE. A dose of 10-20 mg recombinant tissue plasminogen activator (rtPA) was infused over 15 h (approximately 0.75 to 1.5 mg/h) in the USAT group. RV/LV ratio showed a mean decrease at 24 h of 0.30 vs 0.03 in the heparin alone group (P < 0.001). At 90 d, there was one death from pancreatic cancer in the heparin group. There was no major bleeding and 4 episodes of minor bleeding: 3 in the USAT group, 1 in the heparin alone group (P = 0.61). Criticism of this trial includes failure to randomize patients with perhaps the greatest need for catheter directed therapy, the elderly and those with cancer; a low recruitment rate; and failure to follow patients to 6 mo when the heparin alone group may have additionally benefited from physiologic thrombolysis.
There is conflicting evidence as to whether ultrasound assisted delivery of fibrinolytic agents is more effective than infusion alone. In the PREFECT registry[46], 101 consecutive patients were enrolled at 7 sites. Twenty-eight patients had massive PE (28%) and 73 had submassive PE (73%). Patients with massive PE were treated with mechanical thrombectomy or pharmaco-mechanical thrombectomy with clinical success in 24/28 patients and 14% mortality. Clinical success in the submassive group was 97% with 3% mortality. While the device choices for mechanical thrombectomy are not mentioned in the study, the Angiojet device was not used because of reported complications. In a subgroup analysis, comparing USAT with CDT there was no difference in post treatment pulmonary artery pressures, average pressure change, thrombolytic dose, raising the question of the added expense of USAT.
Looking at the evidence of systemic and catheter directed therapy in patients with submassive PE, it appears that patients receiving lytic therapy have a decreased need for escalation of care compared to those with heparin administration alone, a more rapid resolution of afterload on the right heart, but no significant survival advantage. However, there may be greater improvement in pulmonary artery pressures in the long term. The advantages of catheter directed therapies over systemic administration are thrombolytic delivery directly into the clot and the requirement of a lower dose of thrombolytics, which may decrease hemorrhagic complications. In light of the effectiveness of thrombolytics alone, one questions the need for mechanical thrombectomy in submassive PE, unless there is a contraindication to thrombolysis.
As treatment options for patients with PE have evolved, the concept of bringing together experts from different disciplines in an urgent manner to create the best treatment plan for patients presenting with PE has led to the creation of Pulmonary Embolism Response Teams (PERT)[47]. Similar multidisciplinary collaborations have been employed to facilitate patients presenting with stroke (the “Stroke Team”)[48] or cardiac events (the “Heart Team”).
The manner in which clinicians are summoned to make decisions about treatment varies considerably from institution to institution. It may involve alerting the members of the team through a beeper system that a patient has presented, or it may involve protocols which dictate how triage should be accomplished, with the necessary members alerted as needed[49]. Members involved typically include pulmonary/critical care, cardiology, vascular/cardiothoracic surgery and interventional radiology or cardiology. Additional members who may be involved include anesthesiologists, perfusionists, diagnostic radiologists, and pharmacists. Activation may involve several or all of the members converging at the patient’s bedside. In some instances, this may be done via videoconference with subsequent in-person activation of the physicians relevant to the particular patient’s situation[50].
An important function of the PERT process is data collection and the refinement of treatment protocols. By examining outcomes and correlating them with initial data collected, such as high and low heart rates, blood pressure, oxygen saturation, number of segments with thrombus, RV/LV ratio, etc., triage of patients to different treatment arms may be optimized. Ideally, patients may subsequently be seen in follow up in a dedicated PERT clinic. Long term follow up can then be introduced to the PERT database. Centers with PERT programs have the opportunity to share data with each other allowing for more rapid determination of critical treatment parameters. Collaboration regarding data sharing is evolving through multicenter affiliations such as the PERT Consortium[51].
In addition to streamlined treatment, another function of the PERT process is data collection, which will lead to the refinement of treatment protocols. Members of the national PERT Consortium will have the opportunity to share data advancing the understanding of PE and its treatment. The success of a PERT program requires extensive education of referring physicians, house staff, nursing staff, ED and ICU staff, pharmacy, and the community.
Currently, the precise role of catheter directed therapy in the treatment of both massive and submassive PE remains to be established through well-designed prospective controlled trials. For patients with massive PE in whom there is an absolute contraindication for systemic thrombolysis, a failure of systemic thrombolysis or no time for the 2 h of administration of systemic thrombolytic agents, mechanical thrombectomy provides the primary alternative to surgical thrombectomy. With respect to submassive PE, catheter directed therapy decreases the need for treatment escalation, decreases the time for clinical improvement, but does not increase overall survival. An overall reduction in clot burden may decrease the incidence of CETPH and improve quality of life.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Gao BL, Gumustas OG, Shen J, van Beek EJR, Yazdi HR S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Pulido T, Aranda A, Zevallos MA, Bautista E, Martínez-Guerra ML, Santos LE, Sandoval J. Pulmonary embolism as a cause of death in patients with heart disease: an autopsy study. Chest. 2006;129:1282-1287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | McIntyre KM, Sasahara AA. The hemodynamic response to pulmonary embolism in patients without prior cardiopulmonary disease. Am J Cardiol. 1971;28:288-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 333] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | McIntyre KM, Sasahara AA. Determinants of right ventricular function and hemodynamics after pulmonary embolism. Chest. 1974;65:534-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 101] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Stratmann G, Gregory GA. Neurogenic and humoral vasoconstriction in acute pulmonary thromboembolism. Anesth Analg. 2003;97:341-354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 147] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Corrigan D, Prucnal C, Kabrhel C. Pulmonary embolism: the diagnosis, risk-stratification, treatment and disposition of emergency department patients. Clin Exp Emerg Med. 2016;3:117-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Stein PD, Beemath A, Matta F, Weg JG, Yusen RD, Hales CA, Hull RD, Leeper KV Jr, Sostman HD, Tapson VF, Buckley JD, Gottschalk A, Goodman LR, Wakefied TW, Woodard PK. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120:871-879. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 315] [Cited by in F6Publishing: 233] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 7. | Guidelines on diagnosis and management of acute pulmonary embolism. Task Force on Pulmonary Embolism, European Society of Cardiology. Eur Heart J. 2000;21:1301-1336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 433] [Cited by in F6Publishing: 332] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Kucher N, Goldhaber SZ. Management of massive pulmonary embolism. Circulation. 2005;112:e28-e32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 9. | Castelli R, Tarsia P, Tantardini C, Pantaleo G, Guariglia A, Porro F. Syncope in patients with pulmonary embolism: comparison between patients with syncope as the presenting symptom of pulmonary embolism and patients with pulmonary embolism without syncope. Vasc Med. 2003;8:257-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Stein PD, Terrin ML, Hales CA, Palevsky HI, Saltzman HA, Thompson BT, Weg JG. Clinical, laboratory, roentgenographic, and electrocardiographic findings in patients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease. Chest. 1991;100:598-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 58] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Elliott CG, Goldhaber SZ, Visani L, DeRosa M. Chest radiographs in acute pulmonary embolism. Results from the International Cooperative Pulmonary Embolism Registry. Chest. 2000;118:33-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 140] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123:1788-1830. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1460] [Cited by in F6Publishing: 1447] [Article Influence: 111.3] [Reference Citation Analysis (0)] |
| 13. | Grifoni S, Olivotto I, Cecchini P, Pieralli F, Camaiti A, Santoro G, Conti A, Agnelli G, Berni G. Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation. 2000;101:2817-2822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 535] [Cited by in F6Publishing: 505] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 14. | Kreit JW. The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest. 2004;125:1539-1545. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 156] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999;353:1386-1389. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1917] [Cited by in F6Publishing: 1759] [Article Influence: 70.4] [Reference Citation Analysis (0)] |
| 16. | Kasper W, Konstantinides S, Geibel A, Olschewski M, Heinrich F, Grosser KD, Rauber K, Iversen S, Redecker M, Kienast J. Management strategies and determinants of outcome in acute major pulmonary embolism: results of a multicenter registry. J Am Coll Cardiol. 1997;30:1165-1171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 714] [Cited by in F6Publishing: 615] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 17. | Wagenvoort CA. Pathology of pulmonary thromboembolism. Chest. 1995;107:10S-17S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 105] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Dong BR, Hao Q, Yue J, Wu T, Liu GJ. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev. 2009;8:CD004437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Alonso-Martínez JL, Anniccherico-Sánchez FJ, Urbieta-Echezarreta MA, García-Sanchotena JL, Herrero HG. Residual pulmonary thromboemboli after acute pulmonary embolism. Eur J Intern Med. 2012;23:379-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Stein PD, Yaekoub AY, Matta F, Janjua M, Patel RM, Goodman LR, Gross ML, Denier JE. Resolution of pulmonary embolism on CT pulmonary angiography. AJR Am J Roentgenol. 2010;194:1263-1268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Lang IM, Pesavento R, Bonderman D, Yuan JX. Risk factors and basic mechanisms of chronic thromboembolic pulmonary hypertension: a current understanding. Eur Respir J. 2013;41:462-468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 258] [Cited by in F6Publishing: 283] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 22. | Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, Albanese P, Biasiolo A, Pegoraro C, Iliceto S. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350:2257-2264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1236] [Cited by in F6Publishing: 1109] [Article Influence: 55.5] [Reference Citation Analysis (0)] |
| 23. | Moorjani N, Price S. Massive pulmonary embolism. Cardiol Clin. 2013;31:503-518, vii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Meneveau N, Séronde MF, Blonde MC, Legalery P, Didier-Petit K, Briand F, Caulfield F, Schiele F, Bernard Y, Bassand JP. Management of unsuccessful thrombolysis in acute massive pulmonary embolism. Chest. 2006;129:1043-1050. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 177] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 25. | Edelman JJ, Okiwelu N, Anvardeen K, Joshi P, Murphy B, Sanders LH, Newman MA, Passage J. Surgical Pulmonary Embolectomy: Experience in a Series of 37 Consecutive Cases. Heart Lung Circ. 2016;25:1240-1244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Sharafuddin MJ, Hicks ME. Current status of percutaneous mechanical thrombectomy. Part I. General principles. J Vasc Interv Radiol. 1997;8:911-921. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Sharafuddin MJ, Hicks ME. Current status of percutaneous mechanical thrombectomy. Part II. Devices and mechanisms of action. J Vasc Interv Radiol. 1998;9:15-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Dawson CA, Rickaby DA, Linehan JH, Bronikowski TA. Distributions of vascular volume and compliance in the lung. J Appl Physiol (1985). 1988;64:266-273. [PubMed] [Cited in This Article: ] |
| 29. | Tibbutt DA, Fletcher EW, Thomas L, Sutton GC, Miller GA. Evaluation of a method for quantifying the angiographic severity of major pulmonary embolism. Am J Roentgenol Radium Ther Nucl Med. 1975;125:895-899. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Greenfield LJ, Proctor MC, Williams DM, Wakefield TW. Long-term experience with transvenous catheter pulmonary embolectomy. J Vasc Surg. 1993;18:450-457; discussion 457-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Donaldson CW, Baker JN, Narayan RL, Provias TS, Rassi AN, Giri JS, Sakhuja R, Weinberg I, Jaff MR, Rosenfield K. Thrombectomy using suction filtration and veno-venous bypass: single center experience with a novel device. Catheter Cardiovasc Interv. 2015;86:E81-E87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 32. | Al-Hakim R, Park J, Bansal A, Genshaft S, Moriarty JM. Early Experience with AngioVac Aspiration in the Pulmonary Arteries. J Vasc Interv Radiol. 2016;27:730-734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Weinberg AS, Dohad S, Ramzy D, Madyoon H, Tapson VF. Clot Extraction With the FlowTriever Device in Acute Massive Pulmonary Embolism. J Intensive Care Med. 2016;3:676-679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Müller-Hülsbeck S, Brossmann J, Jahnke T, Grimm J, Reuter M, Bewig B, Heller M. Mechanical thrombectomy of major and massive pulmonary embolism with use of the Amplatz thrombectomy device. Invest Radiol. 2001;36:317-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Nassiri N, Jain A, McPhee D, Mina B, Rosen RJ, Giangola G, Carroccio A, Green RM. Massive and submassive pulmonary embolism: experience with an algorithm for catheter-directed mechanical thrombectomy. Ann Vasc Surg. 2012;26:18-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Chechi T, Vecchio S, Spaziani G, Giuliani G, Giannotti F, Arcangeli C, Rubboli A, Margheri M. Rheolytic thrombectomy in patients with massive and submassive acute pulmonary embolism. Catheter Cardiovasc Interv. 2009;73:506-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Dukkipati R, Yang EH, Adler S, Vintch J. Acute kidney injury caused by intravascular hemolysis after mechanical thrombectomy. Nat Clin Pract Nephrol. 2009;5:112-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Tafur AJ, Shamoun FE, Patel SI, Tafur D, Donna F, Murad MH. Catheter-Directed Treatment of Pulmonary Embolism. Clin Appl Thromb Hemost. 2016;1:1076029616661414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 39. | Stein PD, Matta F. Thrombolytic therapy in unstable patients with acute pulmonary embolism: saves lives but underused. Am J Med. 2012;125:465-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 184] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 40. | Kuo WT, Gould MK, Louie JD, Rosenberg JK, Sze DY, Hofmann LV. Catheter-directed therapy for the treatment of massive pulmonary embolism: systematic review and meta-analysis of modern techniques. J Vasc Interv Radiol. 2009;20:1431-1440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 334] [Cited by in F6Publishing: 313] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 41. | Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials. Circulation. 2004;110:744-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 411] [Cited by in F6Publishing: 356] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 42. | Konstantinides S, Geibel A, Heusel G, Heinrich F, Kasper W; Management Strategies and Prognosis of Pulmonary Embolism-3 Trial Investigators. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002;347:1143-1150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 706] [Cited by in F6Publishing: 607] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 43. | Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, Bluhmki E, Bouvaist H, Brenner B, Couturaud F. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014;370:1402-1411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 921] [Cited by in F6Publishing: 918] [Article Influence: 91.8] [Reference Citation Analysis (0)] |
| 44. | Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol. 2013;111:273-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 356] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 45. | Kucher N, Boekstegers P, Müller OJ, Kupatt C, Beyer-Westendorf J, Heitzer T, Tebbe U, Horstkotte J, Müller R, Blessing E. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014;129:479-486. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 550] [Cited by in F6Publishing: 628] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 46. | Kuo WT, Banerjee A, Kim PS, DeMarco FJ Jr, Levy JR, Facchini FR, Unver K, Bertini MJ, Sista AK, Hall MJ, Rosenberg JK, De Gregorio MA. Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis (PERFECT): Initial Results From a Prospective Multicenter Registry. Chest. 2015;148:667-673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 312] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 47. | Dudzinski DM, Piazza G. Multidisciplinary Pulmonary Embolism Response Teams. Circulation. 2016;133:98-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 48. | Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3356] [Cited by in F6Publishing: 3179] [Article Influence: 289.0] [Reference Citation Analysis (0)] |
| 49. | Provias T, Dudzinski DM, Jaff MR, Rosenfield K, Channick R, Baker J, Weinberg I, Donaldson C, Narayan R, Rassi AN. The Massachusetts General Hospital Pulmonary Embolism Response Team (MGH PERT): creation of a multidisciplinary program to improve care of patients with massive and submassive pulmonary embolism. Hosp Pract (1995). 2014;42:31-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 105] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 50. | Kabrhel C, Jaff MR, Channick RN, Baker JN, Rosenfield K. A multidisciplinary pulmonary embolism response team. Chest. 2013;144:1738-1739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 51. | PERT. The National Consortium of Pulmonary Embolism Response Teams: Developing effective solutions to a devastating illness. Available from: http://pertconsortium.org. [Cited in This Article: ] |