Published online Sep 28, 2012. doi: 10.4329/wjr.v4.i9.418
Revised: August 21, 2012
Accepted: August 28, 2012
Published online: September 28, 2012
Embolization of collateral veins is often treated with rigid coils (Gianturco and interlocking detachable coils type). However, when dealing with tortuous and dilated collateral veins, there is a high risk for technical failure and coil migration due to inflexibility of the coils. To safely and successfully solve this problem, Guglielmi detachable coils (GDC) can be used for embolization. Their flexibility allows for easy navigation in tortuous veins, low risk of unintended coil release or coil migration, and safe deployment. A 12-year-old girl with a single ventricle had severe cyanosis and a low exercise tolerance 5 years after Fontan procedure. The symptoms were caused by a tortuous and dilated collateral from the left phrenic vein into the left pulmonary vein, forming a right-to-left shunt. The collateral, which had a large diameter and high flow, and therefore a high risk of coil migration, was successfully embolized with 8 GDC. There were no complications such as coil migration or cerebral infarction. Transcatheter embolization increased her systemic oxygen saturation from 81%-84% to 94%-95%, and increased her ability to exercise. The embolization procedure using flexible GDC was low risk compared with other rigid coil embolization techniques when performing embolization of tortuous and dilated collateral veins.
- Citation: Sonomura T, Ikoma A, Kawai N, Suenaga T, Takeuchi T, Suzuki H, Uchita S, Nakai M, Minamiguchi H, Kishi K, Sato M. Usefulness of the Guglielmi detachable coil for embolization of a systemic venous collateral after Fontan operation: A case report. World J Radiol 2012; 4(9): 418-420
- URL: https://www.wjgnet.com/1949-8470/full/v4/i9/418.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i9.418
Systemic venous collaterals, which originate from a high-pressure systemic vein and drain into a low-pressure pulmonary vein or functional left atrium, may develop after the Fontan procedure in single-ventricle patients[1-6]. They can worsen the patient’s cyanosis due to the right-to-left shunt and limit their exercise ability, both of which can be improved by occlusion of systemic venous collaterals. We embolized an abnormal venous collateral from the left phrenic vein into the left pulmonary vein, which had a large diameter and high flow. In this situation there was a high risk of coil migration[7,8] and the veins were too tortuous to navigate the rigid coils safely and successfully. Therefore we used flexible Guglielmi detachable coils (GDC; Stryker Neurovascular, Fremont, CA). Their flexibility allows for easy navigation in tortuous veins and low risk of unintended coil release or coil migration resulting in a successful embolization.
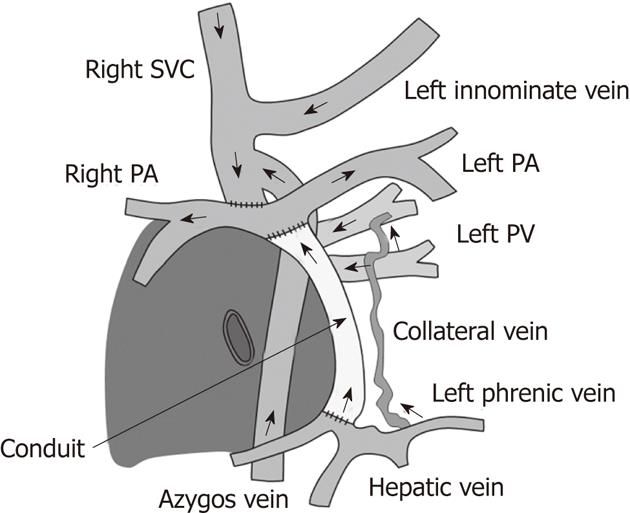
The patient was a 12-year-old girl with multiple anomalies including a single ventricle and atrium, polysplenia, defective inferior vena cava, and a dilated azygos vein flowing into the right superior vena cava (SVC). She underwent the Fontan operation at the age of 5 years and 5 mo. The right SVC was anastomosed to the right pulmonary artery, and hepatic veins were connected to the pulmonary artery using a conduit (Figure 1). At follow-up at the age of 10 years and 4 mo, her systemic oxygen saturation by pulse oximetry (SpO2) had decreased to 81%-84%, and exercise was severely limited. Angiography at the age of 11 years and 11 mo revealed the presence of an abnormal collateral from the left phrenic vein into the left pulmonary vein, which had a large diameter and high flow, and was the main contributing factor of the patient’s cyanosis. Percutaneous transcatheter embolization was selected rather than surgical treatment as a less invasive treatment because of adhesion due to previous multiple surgeries and the nature of the collateral which runs deep into the body.
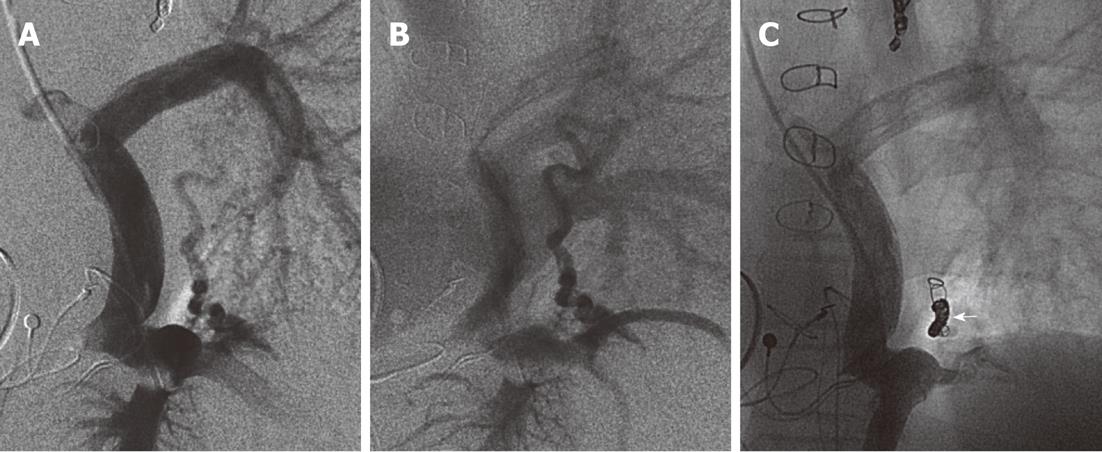
A 4 Fr Judkins (right type) catheter (Goodman, Nagoya, Japan) was advanced into the left phrenic vein via the right internal jugular vein under general anesthesia. A pre-shaped microcatheter (Excelsior SL10 90°, Stryker Neurovascular, Fremont, CA) was inserted with the help of a micro guidewire (GT Reshaped type, Terumo Clinical, Gifu, Japan) into the abnormal venous collateral, which was successfully embolized with 8 GDCs (GDC-10). Initially we used the first GDC (360°Soft SR 7 mm × 9 cm) as an anchor in the collateral. This was followed by progressively smaller GDCs starting with a 2D Soft SR 5 mm × 10 cm GDC to 3 Ultrasoft 4 mm × 8 cm GDCs and finally 3 Ultrasoft 3 mm × 8 cm GDCs (Figure 2). The procedural time of the treatment was 150 min, the fluoroscopic time was 29 min, and the maximum absorption dose at the skin level was estimated to be 98 mGy. There were no complications such as coil migration or cerebral infarction. Following coil embolization, SpO2 increased from 81%-84% to 94%-95% and her exercise limit increased from 3 to 4 according to the following definition: (1) hospital admission is required; (2) exercise is impossible; (3) mild exercise is possible; (4) moderate exercise is possible; and (5) strong exercise is possible or limitless. At follow up 1 year and 5 mo after the procedure, SpO2 was 89%-90% and her exercise limit remained at 4.
Systemic venous collaterals, which originate from a high-pressure systemic vein and drain into a low-pressure pulmonary vein or functional left atrium, may develop after the Fontan operation in single-ventricle patients[1-6]. Weber reported that significant systemic venous collaterals were detected in 7 of 40 patients (18%) after the Fontan operation[2]. Such patients may have severe cyanosis and an increased incidence of cerebrovascular accidents[9] due to the right-to-left shunt. Occlusion of systemic venous collaterals is necessary to improve the cyanosis and to prevent cerebrovascular accidents.
Treatments for occlusion of venous collaterals include surgical ligation[10] and transcatheter embolization[1,3-5], among others. Transcatheter embolization is not only less invasive but often easier and more effective than surgical ligation and has therefore become commonly employed. In this case, transcatheter embolization was selected because of adhesion due to previous multiple surgeries and the nature of the collateral which runs deep into the body. Several reports[1,5] describe embolization of venous collaterals with coils [Gianturco and interlocking detachable coils (IDC) type] and Rashkind occluders. However, no report has described embolization of venous collaterals using GDCs, which are a safe type of coil because there is almost no risk of unintended release or coil migration. GDCs are soft and flexible, whereas other detachable coils and devices are hard and rigid. So, we considered that a thin, flexible GDC (0.0095 or 0.010 inch) was better than a thick, rigid IDC (0.0135 or 0.015 inch) to embolize the collateral vein, because the angle of the left inferior phrenic vein and the tortuous collateral vein was very acute. This makes it difficult to navigate with an IDC, because they are so rigid. A GDC was therefore appropriate because of its greater flexibility. We selected a 360° Soft SR 7 mm × 9 cm GDC as the first coil, because this complex-shaped coil has a larger diameter (7 mm) than that of the collateral vein (4-5 mm), and serves as an anchor to prevent coil migration. Thereafter, we used progressively smaller coils, starting from 5 mm and working down to 3 mm, to achieve compact embolization.
In a retrospective review of the cardiac catheterization data of 50 cyanotic patients after the Fontan operation, Sugiyama identified a total of 68 systemic venous collaterals[5]. Of these, the origin was supracardiac in 36 (53%), cardiac in 12 (18%), and infracardiac in 20 (29%). The most common site of origin was the brachiocephalic vein, in 30 of the 68 collaterals (44%), followed by the left phrenic vein in 17 (25%). Eighteen collaterals drained directly into the pulmonary veins, while the others drained into the functional left atrium. In the present case, the collateral originated from the left phrenic vein and drained into the left pulmonary vein.
In terms of anatomic factors, heterotaxia syndrome is the only predictor for venous collaterals (53% in heterotaxia vs 22% in non heterotaxia, P < 0.01)[6]. The present patient had polysplenia.
The short-term efficacy of occlusion of venous collaterals is reported[1,3,5], but long-term efficacy has not been addressed. Further development of collateral veins may occur in response to the high systemic venous pressure.
We safely and successfully achieved GDC embolization of a tortuous and dilated collateral from the left phrenic vein into the left pulmonary vein in a 12-year-old girl with a single ventricle. The embolization procedure using GDCs was low risk compared with other rigid coil embolization techniques in this case.
Peer reviewers: Roberto Miraglia, MD, Department of Diagnostic and Interventional Radiology, Mediterranean Institute for Transplantation and Advanced Specialized Therapies (IsMeTT), Via Tricomi 1, 90100 Palermo, Italy; Poul Erik Andersen, MD, PhD, Associate Professor, Department of Radiology, Odense University Hospital, Sdr. Boulevard, DK-5000 Odense C, Denmark
S- Editor Cheng JX L- Editor O’Neill M E- Editor Xiong L
| 1. | Hsu HS, Nykanen DG, Williams WG, Freedom RM, Benson LN. Right to left interatrial communications after the modified Fontan procedure: identification and management with transcatheter occlusion. Br Heart J. 1995;74:548-552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Weber HS. Incidence and predictors for the development of significant supradiaphragmatic decompressing venous collateral channels following creation of Fontan physiology. Cardiol Young. 2001;11:289-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Ro PS, Weinberg PM, Delrosario J, Rome JJ. Predicting the identity of decompressing veins after cavopulmonary anastomoses. Am J Cardiol. 2001;88:1317-1320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Kaulitz R, Ziemer G, Paul T, Peuster M, Bertram H, Hausdorf G. Fontan-type procedures: residual lesions and late interventions. Ann Thorac Surg. 2002;74:778-785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Sugiyama H, Yoo SJ, Williams W, Benson LN. Characterization and treatment of systemic venous to pulmonary venous collaterals seen after the Fontan operation. Cardiol Young. 2003;13:424-430. [PubMed] [Cited in This Article: ] |
| 6. | Heinemann M, Breuer J, Steger V, Steil E, Sieverding L, Ziemer G. Incidence and impact of systemic venous collateral development after Glenn and Fontan procedures. Thorac Cardiovasc Surg. 2001;49:172-178. [PubMed] [Cited in This Article: ] |
| 7. | Kung GC, Moore P, McElhinney DB, Teitel DF. Retrograde transcatheter coil embolization of congenital coronary artery fistulas in infants and young children. Pediatr Cardiol. 2003;24:448-453. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Seltzer S, Aboulhosn J, Levi DS. Use of interlock fibered detachable coils for occlusion of collaterals, coronary artery fistulae, and patent ductus arteriosus. Catheter Cardiovasc Interv. 2009;74:770-776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | du Plessis AJ, Chang AC, Wessel DL, Lock JE, Wernovsky G, Newburger JW, Mayer JE. Cerebrovascular accidents following the Fontan operation. Pediatr Neurol. 1995;12:230-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 120] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Fontan F, Deville C, Quaegebeur J, Ottenkamp J, Sourdille N, Choussat A, Brom GA. Repair of tricuspid atresia in 100 patients. J Thorac Cardiovasc Surg. 1983;85:647-660. [PubMed] [Cited in This Article: ] |