Copyright
©The Author(s) 2022.
World J Radiol. Jun 28, 2022; 14(6): 137-150
Published online Jun 28, 2022. doi: 10.4329/wjr.v14.i6.137
Published online Jun 28, 2022. doi: 10.4329/wjr.v14.i6.137
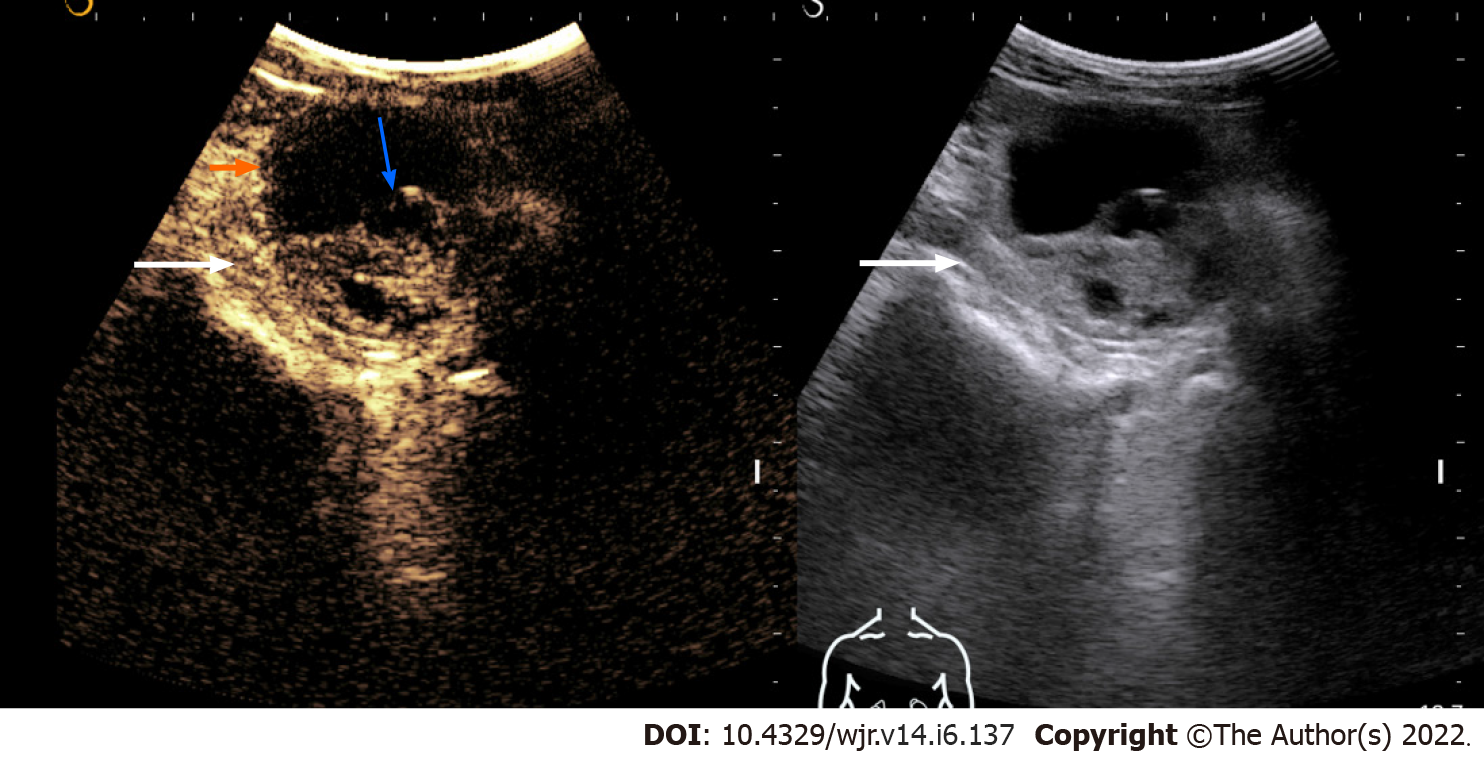
Figure 1 Contrast-enhanced ultrasonography images of a solid-cystic lesion in the left kidney showing thick nodular septal enhancement (blue arrow) and enhancement of solid component (long arrow).
Consistent with Bosniak category 4 lesion/malignant lesion. The lesion was resected and histology revealed clear cell renal cell carcinoma.
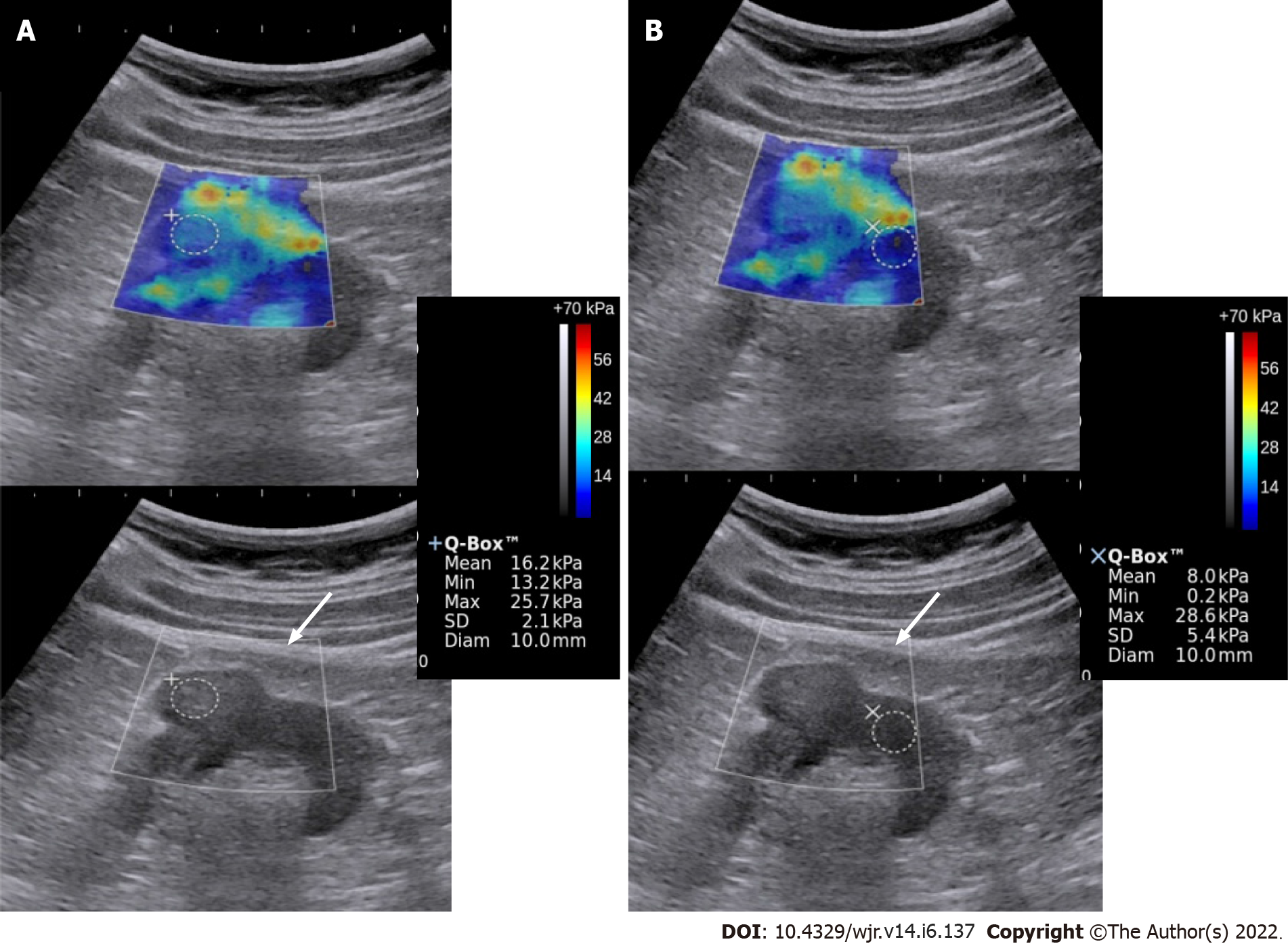
Figure 2 Elastography & gray-scale images of the renal mass (A) and the normal kidney (B).
The mass showed greater stiffness relative to the surrounding kidney. Biopsy showed high-grade renal cell carcinoma.
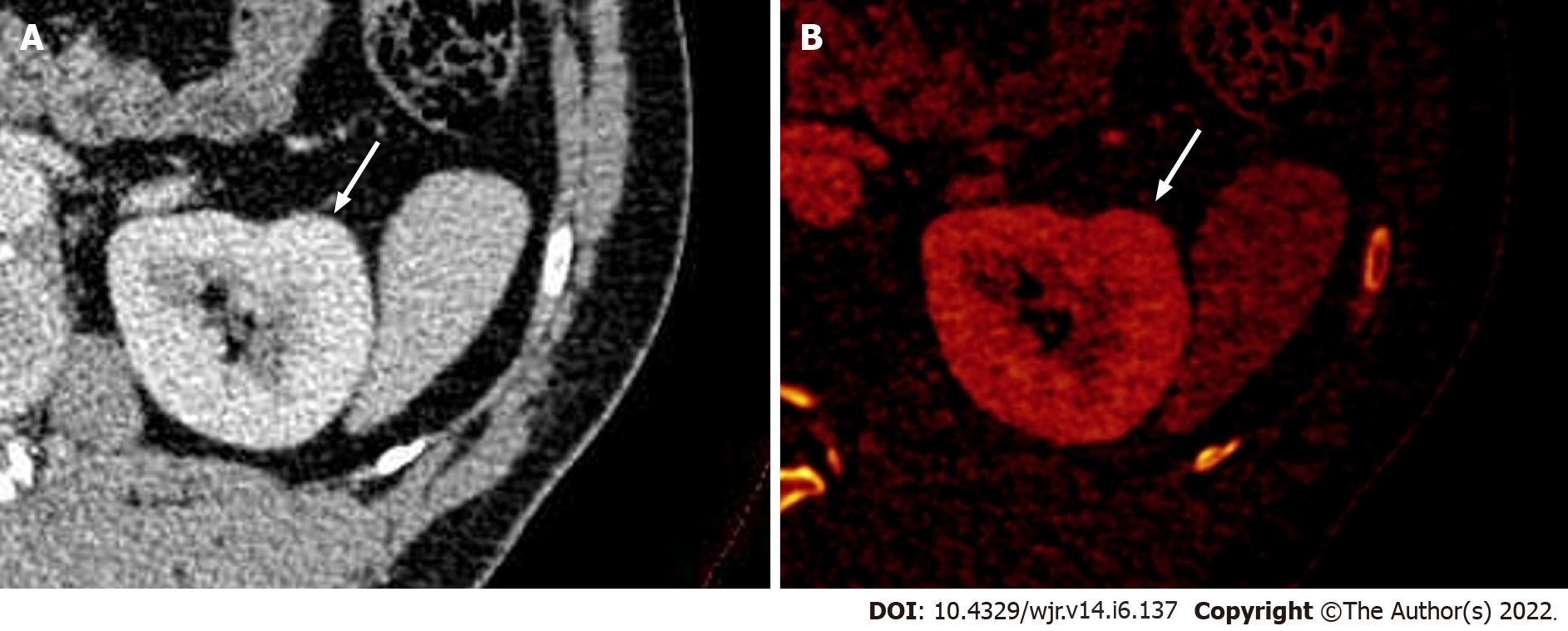
Figure 3 Dual-energy computed tomography images.
A: Contrast-enhanced axial dual-energy computed tomography image showing contour bulge from the lateral cortex of the interpolar region of the left kidney, enhanced similar to background parenchyma; B: Iodine overlay image confirming the absence of any differential iodine distribution, suggesting the lesion to be a dromedary hump.
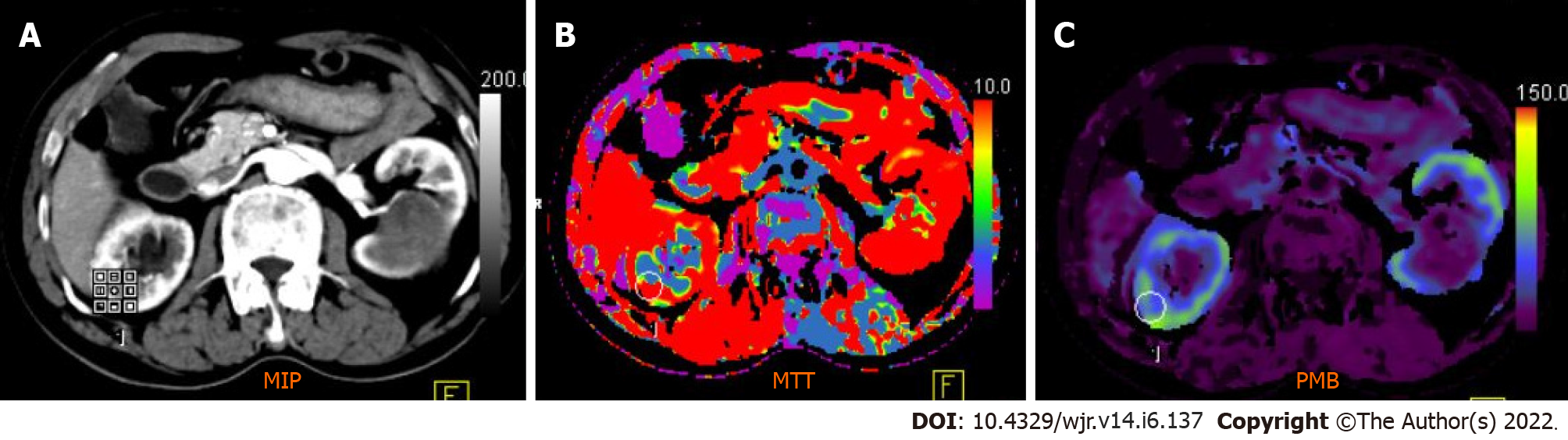
Figure 4 Computed tomography perfusion images (A-C) reveal a significant difference in permeability and mean transit time values between normal renal cortex and malignant lesions.
Mean transit time (MTT) and permeability (PMB) in normal renal cortex were 10.48 s and 55.56 mL/100 mL/min, respectively, which were significantly different from those of renal cell carcinoma (RCC) (MTT: 9.06 s; PMB: 237.09 mL/100 mL/min). A cut-off of 2.5 mL/100 g/min yielded a 100% sensitivity and 95.92% accuracy to predict RCC.
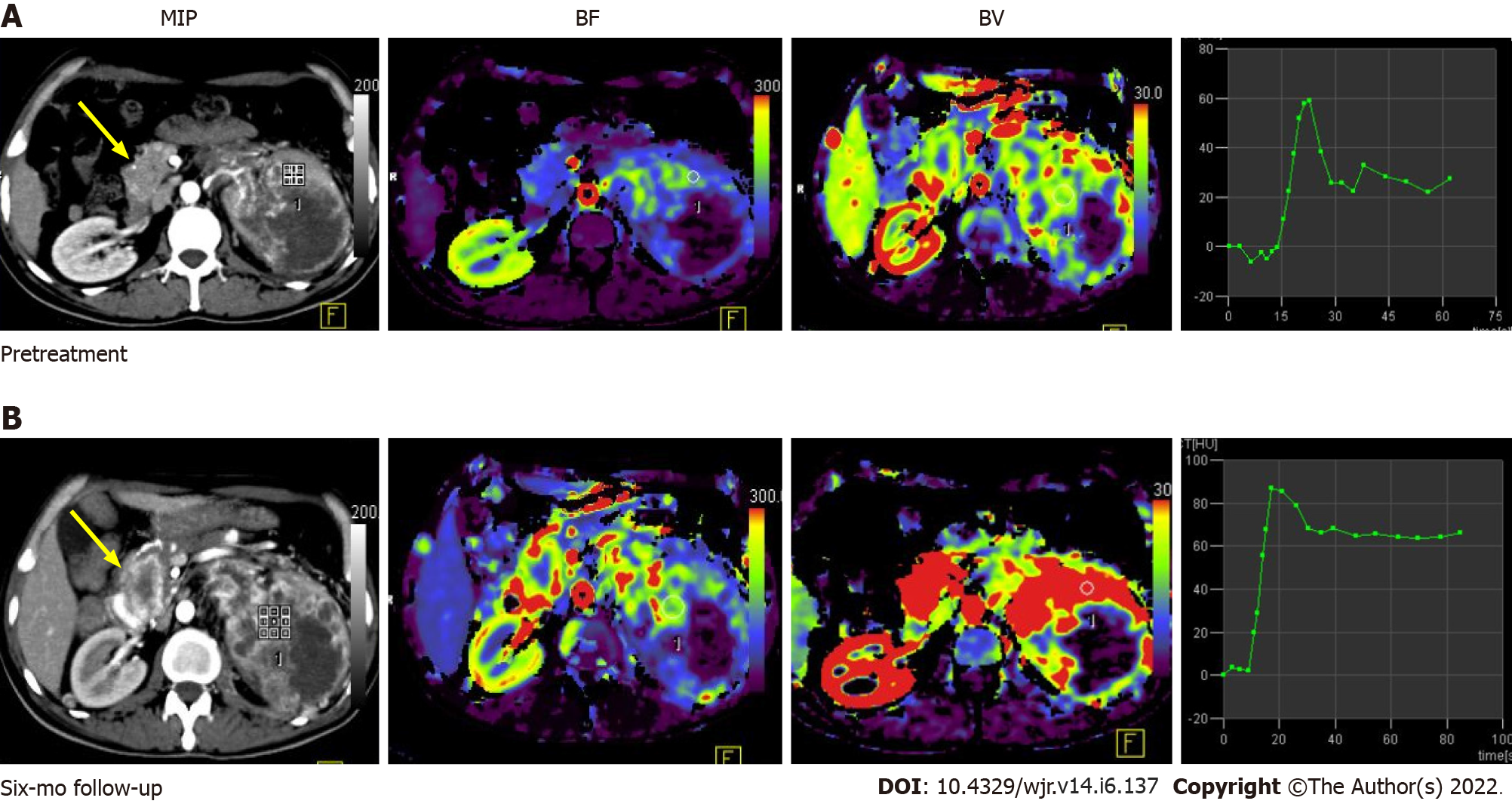
Figure 5 Pre-treatment (A) and post-treatment (B) computed tomography perfusion images in a case of large left renal cell carcinoma with metastasis to the uncinate process of the pancreas (yellow arrow).
Comparison of perfusion parameters at the 6-mo follow-up after anti-angiogenic therapy showed that there was an increase in BF and BV, which was suggestive of progressive disease. No significant change in lesion size would have qualified this case as a stable disease as per size criteria.
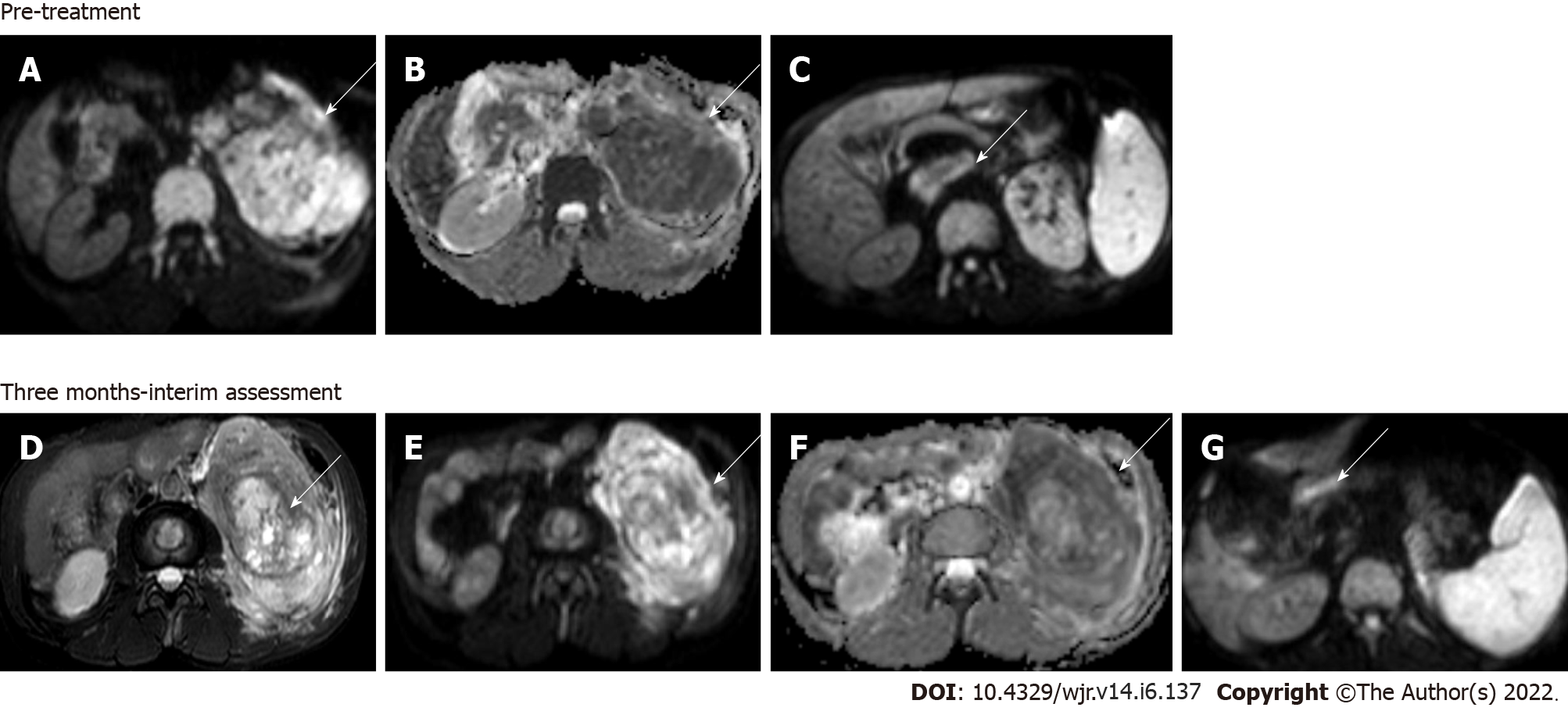
Figure 6 Magnetic resonance images.
Diffusion-weighted imaging (DWI) at b = 800 s/mm2 (A) and apparent diffusion coefficient (ADC) map (B) showed large clear cell renal cell carcinoma replacing the left kidney showing markedly restricted diffusion; DWI image (C) showing a malignant thrombus extending to the inferior vena cava (arrow) Axial T2W FS image (D) showing that 3 mo after treatment with sorafenib (a tyrosine kinase inhibitor), there was no significant change in the size of the lesion; however, there was increased necrosis in the mass; Resultant increase in ADC value on the corresponding DWI at b = 800 s/mm2 (E) and ADC map (F); DWI (G) also revealed partial recanalization of the malignant thrombus (arrow)—overall features suggestive of partial response.
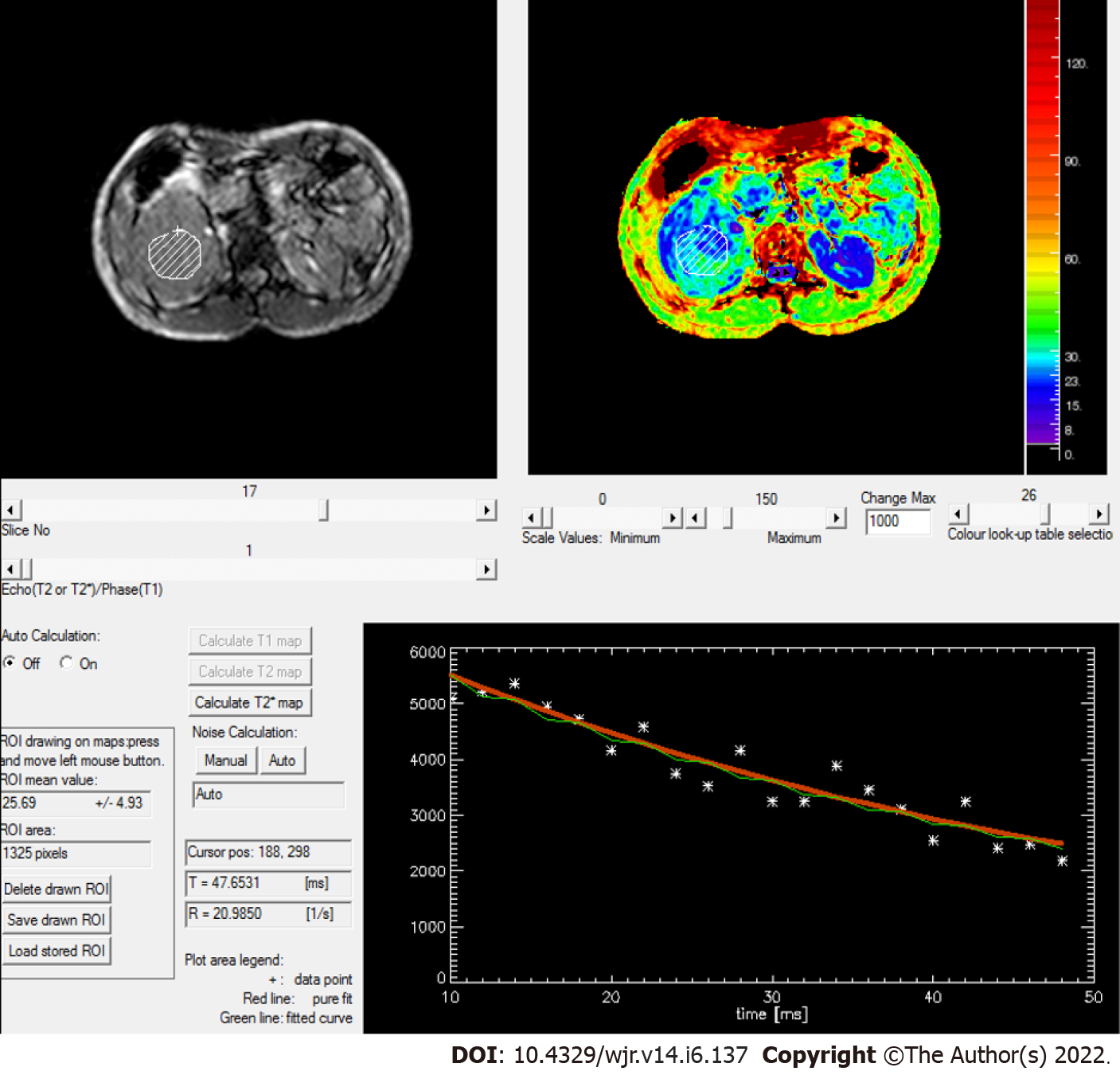
Figure 7 Rate of spin dephasing (R2* map) showing R2* value of right renal cell carcinoma (20.
9/s), which was lower than that of a normal kidney (25.5/s).
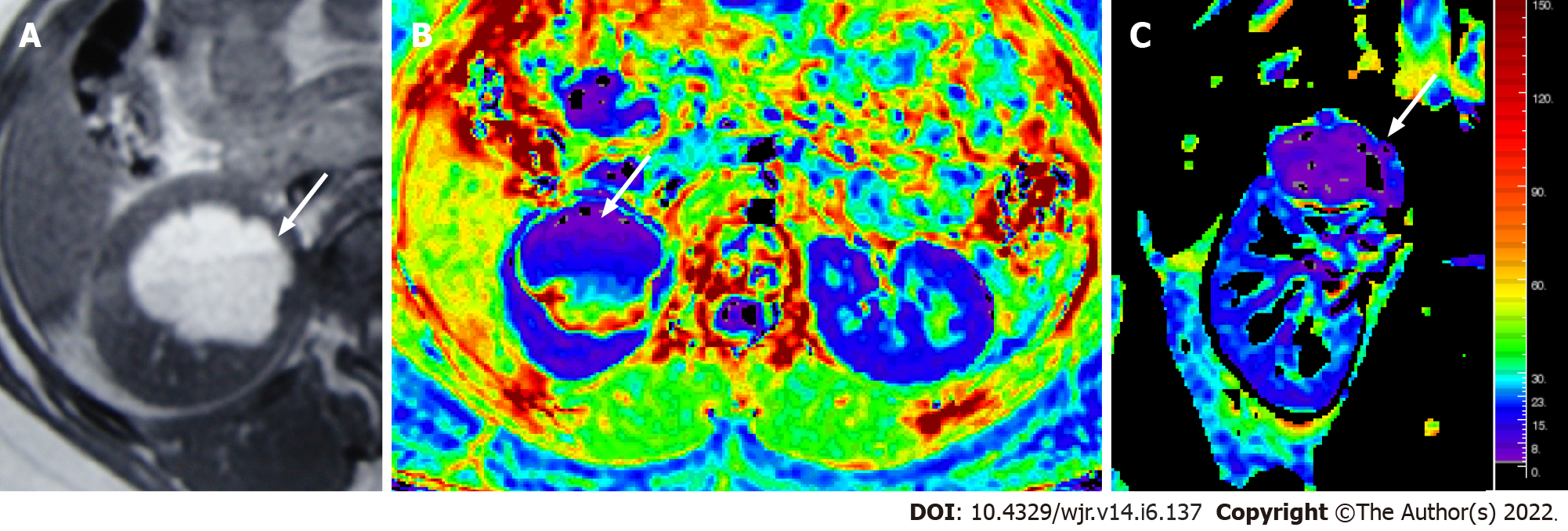
Figure 8 Magnetic resonance images.
T1W axial MR image (A) showing a hyperintense lesion in the upper pole of the right kidney, with fluid-fluid level, suggestive of a hemorrhagic cyst; Axial & coronal R2* maps (B and C) showing an R2* value of 6.1/s.
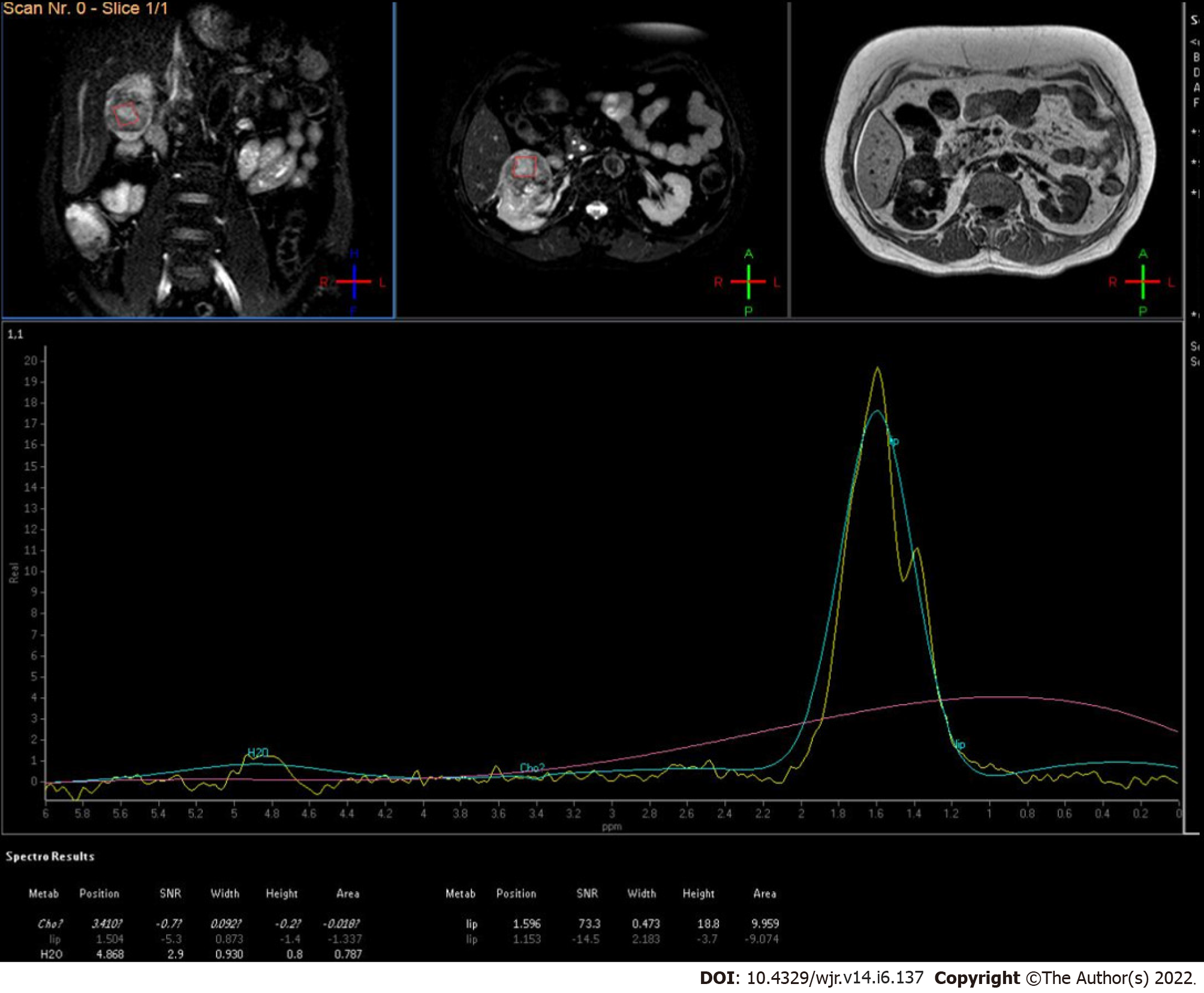
Figure 9
MR spectroscopy of low-grade renal cell carcinoma showed increased lipid-lactate peak.
- Citation: Aggarwal A, Das CJ, Sharma S. Recent advances in imaging techniques of renal masses. World J Radiol 2022; 14(6): 137-150
- URL: https://www.wjgnet.com/1949-8470/full/v14/i6/137.htm
- DOI: https://dx.doi.org/10.4329/wjr.v14.i6.137