Published online Aug 26, 2017. doi: 10.4330/wjc.v9.i8.710
Peer-review started: February 7, 2017
First decision: May 11, 2017
Revised: May 22, 2017
Accepted: June 19, 2017
Article in press: July 17, 2017
Published online: August 26, 2017
We describe the case of a patient presenting with ST-segment elevation myocardial infarction due to very late scaffold thrombosis. The patient was already admitted for an elective percutaneous recanalization of a chronically occluded left anterior descending artery (LAD). The procedure was performed according the sub-intimal tracking and re-entry (STAR) technique with 4 bioresorbable vascular scaffolds implantation. However, even though the coronary flow was preserved at the end of the procedure, the dissected segment was only partially sealed at the distal segment of the LAD. After 18 mo of regular assumption, dual antiplatelet therapy was discontinued for 10 mo before his presentation at the emergency room. This is the first reported case of a very late scaffold thrombosis after coronary chronic total occlusion (CTO) recanalization performed according to the STAR technique. This case raises concerns about the risk of very late scaffold thrombosis after complex CTO revascularization.
Core tip: We describe a case of a 53-year-old male patient who was admitted with anterior ST-elevation myocardial infarction 28 mo after elective percutaneous revascularization of a chronically occluded left anterior descending (LAD) threated with 4 bioresorbable vascular scaffolds (BVS) in order to seal a long flow limiting dissection after sub-intimal tracking and re-entry technique. Coronary angiography showed a large thrombus at the proximal segment of the proximal BVS and a long dissection was evident from mid to distal LAD. In this case, the progressive reduction of both scaffolds radial strength and structure dismantling might have been responsible for both intraluminal thrombosis and reoccurrence of vessel dissection.
- Citation: Di Serafino L, Cirillo P, Niglio T, Borgia F, Trimarco B, Esposito G, Stabile E. Very late bioresorbable scaffold thrombosis and reoccurrence of dissection two years later chronic total occlusion recanalization of the left anterior descending artery. World J Cardiol 2017; 9(8): 710-714
- URL: https://www.wjgnet.com/1949-8462/full/v9/i8/710.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i8.710
Bioresorbable vascular scaffolds (BVS) represents the latest revolution in the field of interventional cardiology. Providing temporary scaffolding and disappearing few years later, BVS results particularly appealing for the treatment of long segments of coronary arteries such as it usually occurs for percutaneous revascularization (PCI) of chronic total occlusions (CTO). However, limited data are available about the long-term efficacy of BVS in this particular setting. Herein we report a case of a very late scaffold thrombosis after CTO revascularization.
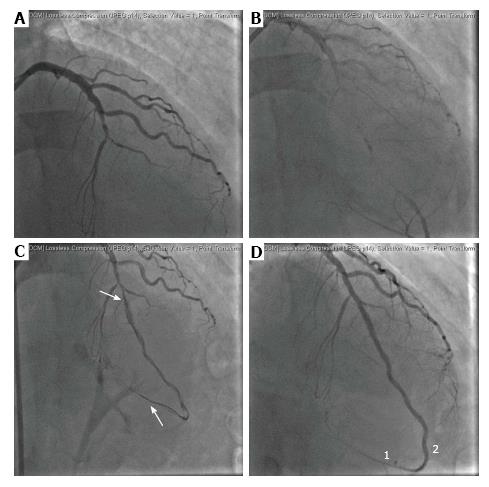
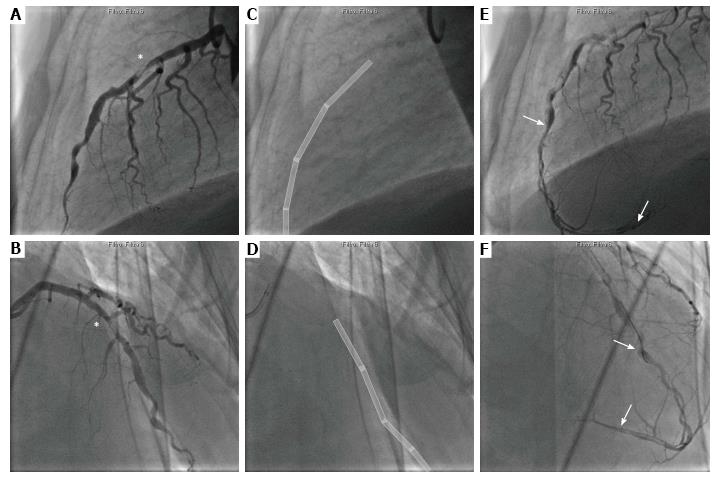
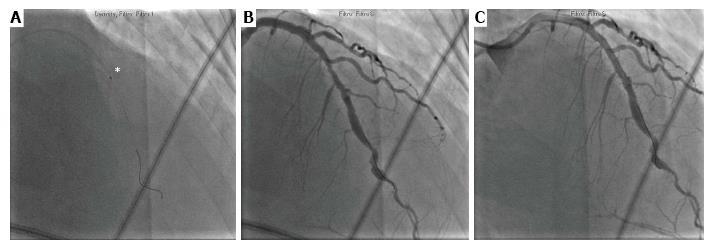
A 53-year-old male patient, with hypertension and dyslipidemia, presented with anterior ST-elevation myocardial infarction, 28 mo after elective percutaneous coronary intervention (PCI) of the chronically occluded left anterior descending artery (LAD), with implantation of 4 marker-to-marker bioresorbable vascular scaffolds (BVS, Absorb Abbott Vascular, Abbott Park, Illinois), performed in another cath-lab. BVS implantation followed chronic total occlusion (CTO) recanalization unintentionally performed according the subintimal tracking and re-entry (STAR) technique. The dissected segment was only partially sealed up to the distal segment of the LAD (Figure 1). The patient completed 18 mo of dual antiplatelet therapy (DAPT) 10 mo before his presentation at the emergency room. The index coronary angiography showed a large thrombus at the proximal segment of the proximal BVS followed by a long dissection up to the very distal LAD segment (Figure 2). Thrombus aspiration and proximal drug eluting stent (DES) implantation was performed, while medical treatment was suggested for the distal chronic dissection (Figure 3). DAPT with ASA and Ticagrelor was finally resumed and clinical follow up planned.
To the best of our knowledge, this is the first clinical case reporting on a very late scaffold thrombosis and reoccurrence of coronary dissection after PCI of a chronic coronary total occlusion. Since neither optical coherence tomography (OCT) nor intravascular ultrasound (IVUS) were available at the time of both baseline and index procedures, the mechanism subtending the BVS failure in this particular case remains unknown. However, we might speculate that intraluminal scaffold dismantling together with scaffold discontinuity and restenosis during the resorption process, might have been responsible of thrombus formation at the mid-LAD, as previously described[1-3]. In addition, the gradual scaffold resorption process, together with the incomplete scaffold coverage of the dissected segment at the time of the CTO PCI, might have been responsible of incomplete dissection healing, with progressive expansion of the subintimal hematoma, resulting in a “dual lumen” coronary artery[4,5]. CTOs are the most challenging coronary lesions for PCI, mainly because of two reasons: (1) Procedure related: CTO remains technically challenging, in fact PCI failure is reported in up to 35% of CTOs and > 40% of CTOs are not attempted and treated either with medical therapy or with CABG; (2) Patient related: Identification of those patients for whom PCI of CTO does not bring any significant clinical benefit, despite successful revascularization, is still debatable[6]. By the way, the use of BVS for CTO revascularization is particularly appealing mainly because PCI normally involves long coronary segments, thereby limiting future surgical interventions and increasing the risk of late malapposition after Drug Eluting Stents (DES) implantation[7,8]. However, limited data are available about the use of BVS for PCI of CTOs. In fact, most of the randomized controlled trials conducted so far compared BVS and DES in simple or intermediate coronary artery stenosis, thereby the long-term efficacy of such new devices for percutaneous revascularization of complex stenosis, such as CTOs is still not clear. Recently, a propensity score adjusted analysis of 537 patients undergoing to PCI of a CTO showed a trend toward a higher adjusted risk of ischemia-driven target lesion revascularization for patients undergoing to BVS implantation as compared with DES[9]. However, larger randomized studies are warrant in order to better define the role of BVS in CTO-PCI.
This case raises concerns about the risk of very late scaffold thrombosis and the use of BVS in complex CTO-PCI, particularly when “full polymer jacket” is not warranted for the entire dissected coronary segment. A prolonged DAPT should be encouraged while a complete sealing of the dissected segment should be considered[10].
A 53-year-old male patient presenting with chest pain for an anterior ST-elevation myocardial infarction.
Anterior ST-elevation myocardial infarction due to very late scaffold thrombosis.
Clinical characteristic, patient’s medical history and echocardiography were useful for differential diagnosis between pericarditis and aortic dissection.
High sensitive Troponin-I increased together with myoglobin and creatine kinase-MB.
Definite diagnosis was possible with invasive coronary angiography which showed a large thrombus at the proximal segment of the proximal bioresorbable vascular scaffolds (BVS) followed by a long dissection up to the very distal left anterior descending segment.
In the acute setting of the coronary syndrome, no thrombus was kept for pathological analysis.
Thrombus aspiration and proximal drug eluting stent implantation was performed, while medical treatment was suggested for the distal chronic dissection.
To the knowledge, there are only few case reports about very late scaffold thrombosis.
This case raises concerns about the use of BVS in complex chronic total occlusion percutaneous revascularization (PCI), thereby suggesting a prolonged dual-antiplatelet therapy tailored according to both patients’ clinical characteristics and PCI procedures.
This case report of late thrombosis after chronic total occlusion recanalization with bioabsorbable scaffold is well organized.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Aggarwal A, Iacoviello M, Kato M, Said SAM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Chan CY, Wu EB, Yan BP. Very Late Bioresorbable Scaffold Thrombosis Caused by Intraluminal Scaffold Dismantling. JACC Cardiovasc Interv. 2016;9:1844-1847. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Räber L, Brugaletta S, Yamaji K, O’Sullivan CJ, Otsuki S, Koppara T, Taniwaki M, Onuma Y, Freixa X, Eberli FR. Very Late Scaffold Thrombosis: Intracoronary Imaging and Histopathological and Spectroscopic Findings. J Am Coll Cardiol. 2015;66:1901-1914. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 173] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 3. | Schiattarella GG, Magliulo F, D’Alise G, Mannacio V, Ilardi F, Trimarco B, Esposito G, Cirillo P. The pitfalls of managing thrombosis of an Absorb™-treated bifurcation. Int J Cardiol. 2014;174:e93-e95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Carlino M, Godino C, Latib A, Moses JW, Colombo A. Subintimal tracking and re-entry technique with contrast guidance: a safer approach. Catheter Cardiovasc Interv. 2008;72:790-796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Carlino M, Figini F, Ruparelia N, Uretsky BF, Godino C, Latib A, Bertoldi L, Brilakis E, Karmpaliotis D, Antoniucci D. Predictors of restenosis following contemporary subintimal tracking and reentry technique: The importance of final TIMI flow grade. Catheter Cardiovasc Interv. 2016;87:884-892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Di Serafino L, Borgia F, Maeremans J, Pyxaras SA, De Bruyne B, Wijns W, Heyndrickx G, Dens J, Di Mario C, Barbato E. The age, creatinine, and ejection fraction score to risk stratify patients who underwent percutaneous coronary intervention of coronary chronic total occlusion. Am J Cardiol. 2014;114:1158-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Galassi AR, Tomasello SD, Reifart N, Werner GS, Sianos G, Bonnier H, Sievert H, Ehladad S, Bufe A, Shofer J. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7:472-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 230] [Cited by in F6Publishing: 233] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 8. | Hong MK, Mintz GS, Lee CW, Park DW, Park KM, Lee BK, Kim YH, Song JM, Han KH, Kang DH. Late stent malapposition after drug-eluting stent implantation: an intravascular ultrasound analysis with long-term follow-up. Circulation. 2006;113:414-419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 263] [Cited by in F6Publishing: 271] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 9. | Azzalini L, Giustino G, Ojeda S, Serra A, La Manna A, Ly HQ, Bellini B, Benincasa S, Chavarría J, Gheorghe LL. Procedural and Long-Term Outcomes of Bioresorbable Scaffolds Versus Drug-Eluting Stents in Chronic Total Occlusions: The BONITO Registry (Bioresorbable Scaffolds Versus Drug-Eluting Stents in Chronic Total Occlusions). Circ Cardiovasc Interv. 2016;9:e004284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Capodanno D, Angiolillo DJ. Antiplatelet Therapy After Implantation of Bioresorbable Vascular Scaffolds: A Review of the Published Data, Practical Recommendations, and Future Directions. JACC Cardiovasc Interv. 2017;10:425-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |