Published online May 26, 2017. doi: 10.4330/wjc.v9.i5.442
Peer-review started: November 2, 2016
First decision: January 14, 2017
Revised: February 1, 2017
Accepted: March 12, 2017
Article in press: March 13, 2017
Published online: May 26, 2017
Processing time: 203 Days and 22.8 Hours
To study the relationship of jailed polymer jacketed guide wires (PGW) with procedural myocardial infarction (PMI) after bifurcation coronary interventions.
Consecutive bifurcation interventions performed from January 2010 to October 2014 were included in the study. Chart review was performed to obtain demographic, clinical and procedural data. PMI was defined as Creatine Kinase MB > 3 × upper reference limit of normal. Multivariate logistic regression was used to ascertain relationship of PGW use with PMI.
Two hundred and ninety-three patients (age 63.5 ± 12.3 years; 33.8% diabetic) were included in the study. Eighty point two percent (n = 235) were true bifurcation lesions use of PGW was associated with PMI on univariate analysis (OR = 4.1; P = 0.002). This association remained significant after adjusting for other possible risk factors (OR = 3.5; P = 0.02).
Our results suggest that PGW use for side branch protection may be associated with PMI. Randomized studies are needed to validate these findings.
Core tip: This is a retrospective study aiming to investigate the relationship of jailed polymer jacketed guide wires (PGW) with procedural myocardial infarction (PMI) after a bifurcation coronary intervention. There is concern that this causes polymer shearing and distal micro-embolization. Our data suggests that jailed PGW are strongly associated with PMI, even after adjusting for pertinent risk factors. Thus caution should be exercised in routinely jailing PGW until further definitive data are available.
- Citation: Chatterjee A, White JS, Hashim T, Leesar MA. Jailing polymer jacketed guide-wires during bifurcation coronary interventions is associated with procedural myocardial infarction. World J Cardiol 2017; 9(5): 442-447
- URL: https://www.wjgnet.com/1949-8462/full/v9/i5/442.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i5.442
Coronary bifurcation lesions (CBL) are a challenging subset of day to day coronary interventions with a higher adverse event profile as compared to non-bifurcation lesions[1]. In the past decade, multiple studies have investigated the optimum approach to bifurcation lesions vis-à-vis simple (provisional side branch stenting only) vs complex (mandatory main and side branch stenting) approaches[2-4]. These have led to a widespread consensus that the simple approach should be preferred in majority of CBLs as the complex strategy showed higher incidence of adverse cardiac events, mainly myocardial infarction[5].
In the simple approach, a coronary guidewire is frequently inserted into the side-branch (SB) as a strategy to prevent occlusion. This is considered to be an important step as side branch compromise is associated with higher incidence of myocardial infarction and death[6,7]. Stent deployment in the main vessel (MV) “jails” this guidewire which then has to be pulled from underneath the stent struts. Polymer jacketed guidewires (PGW) have the advantage of maximum lubricity which allows them to be easily withdrawn from a jailed position. However there are concerns over wire damage and shearing of the polymer jacket[8] and hence these are not universally recommended for jailing[9]. In addition, studies of pathological specimens have revealed evidence of embolized polymer in the myocardium[10,11]. Guidewires with no or minimal polymer coatings are felt to be safer but run a risk of wire fracture during attempts at withdrawal[12]. In a pilot study using scanning electron microscopy (SEM) at our institution, it was established that polymer shearing is a real phenomenon and that the amount of polymer sheared is weakly correlated with biomarker release post procedure[13]. These studies have posed a question regarding an incremental risk of myonecrosis and possibly procedural myocardial infarction (PMI) with jailing of PGW and polymer shearing.
To try and answer this question, we performed a retrospective analysis of consecutive CBL interventions at our institution to determine if there is any association between type of guidewire jailed and PMI.
All coronary interventions performed between January 2010 and October 2014 at our institution were reviewed to identify CBL interventions. Inclusion criteria were: CBL requiring percutaneous coronary intervention (PCI), MV diameter ≥ 2.5 mm and side branch diameter ≥ 2 mm. Criteria for exclusion were PCI for chronic total occlusions, cases where dual antiplatelet therapy was started after PCI and unavailability of biomarker levels at least 12 h after PCI. The Institutional Review Board of the University of Alabama at Birmingham approved the study. Chart review was performed to extract demographic and clinical parameters. Patients were divided into two groups based on occurrence of PMI as defined below.
Angiograms were reviewed and quantitative measurements made using the CAAS system. A CBL was defined as a lesion located at a major coronary bifurcation point. Lesions were classified according to the Medina classification with a score of “1” or “0” being given to the proximal MV, distal MV and the SB components if they had ≥ 50% diameter stenosis. Lesions were also classified as true bifurcation lesions (Medina type 1,1,1; 1,0,1 or 0,1,1) vs non-true bifurcation lesions (Medina type 1,0,0; 0,1,0 or 0,0,1).
PMI was defined as creatine kinase (CK) MB > 3 × 99th percentile of upper limit of normal post procedure if the pre-procedure levels were normal or a > 20% increase if pre-procedure levels were abnormal but stable or down-trending. If there were any unrelated cause for biomarker elevation, e.g., acute stent thrombosis, no reflow, SB occlusion, < TIMI 3 flow in MV or SB, shock or hypotension in the immediate 24 h post PCI, acute kidney injury, stroke, bleeding requiring transfusion, pulmonary embolism, access complication causing limb ischemia or sustained arrhythmia these cases were classified as not having PMI. This was done to focus only on cases without a clear explanation for cause of PMI.
Continuous variables are represented as mean ± SD and compared using the Welch’s t test as the sample sizes are unequal. Categorical variables were compared using the Fisher’s exact test. Statistical analyses were carried out using SPSS v 22.0 (SPSS, Chicago, Illinois). Multivariate logistic regression was used to ascertain relationship of the following variables with PMI: Age, Diabetes Mellitus, severe lesion calcification, true bifurcation lesion, use of newer antiplatelet agent (Ticagrelor and Prasugrel), Bivalirudin use, upstream Glycoprotein IIb/IIIa use, use of preplanned two stent technique, SB protection with any guidewire and SB protection with PGW.
A total of 293 consecutive patients undergoing CBL interventions were included in the study. Seven point eight percent (n = 23) patients were classified as having had a PMI. Demographic and clinical characteristics of the patients broken down into two groups depending on whether or not PMI occurs are shown in Table 1. There were no statistically significant differences between the two groups. Table 2 shows the angiographic and procedural characteristics of patients with and without PMI. The most common bifurcation lesions included were left anterior descending/diagonal and left circumflex/marginal branch respectively. Proportion of true bifurcation lesions was higher and Bivalirudin use lower in the PMI group but these differences did not reach statistical significance. Seventy-four point four percent of total patients had a wire placed in the side branch and jailed with no difference amongst the two groups. However a jailed PGW was much more common in the PMI group (43.4% vs 15.9%, P = 0.003). There were no instances of wire entrapment or wire rupture in either group. The most common PGW jailed was a Hi Torque Whisper (Abbot Vascular, Abbott Park, IL, United States) while non PGW jailed were Runthrough NS (Terumo Interventional Systems, Somerset, NJ, United States), Cougar LS (Medtronic, Minneapolis, MN, United States) and HT Balance Middle Weight (BMW, Abbot Vascular, Abbott Park, IL, United States).
| No PMI (n = 270) | PMI (n = 23) | P value | |
| Age (yr) | 63.6 ± 12.1 | 62.9 ± 14.4 | 0.80 |
| Male sex | 68.1% | 60.9% | 0.49 |
| Smoking | 55.6% | 52.2% | 0.86 |
| Diabetes mellitus | 33.0% | 43.5% | 0.36 |
| Hypertension | 78.1% | 65.2% | 0.33 |
| Hyperlipidemia | 73.7% | 78.3% | 0.87 |
| Acute coronary syndrome | 45.6% | 52.2% | 0.66 |
| No PMI (n = 270) | PMI (n = 23) | P value | |
| Vessels involved | 0.68 | ||
| LM bifurcation | 15.9% | 21.7% | |
| LAD/Diagonal | 40.0% | 47.8% | |
| LCX/OM | 34.8% | 21.7% | |
| RPDA/RPLA | 8.8% | 4.3% | |
| RCA/RV marginal | 0.003% | 0% | |
| Severe calcification | 57.4% | 65.2% | 0.52 |
| True bifurcation (Medina 1,1,1; 1,0,1; 0,1,1) | 79.3% | 91.3% | 0.27 |
| Main vessel diameter (mm) | 3.3 ± 0.5 | 3.3 ± 0.4 | 0.4 |
| Side branch diameter (mm) | 2.6 ± 0.5 | 2.6 ± 0.4 | 0.94 |
| Antiplatelet therapy | 0.97 | ||
| Plavix | 73.7% | 69.6% | |
| Prasugrel | 7.0% | 8.7% | |
| Ticagrelor | 19.3% | 21.7% | |
| Anticoagulant | 0.08 | ||
| Heparin | 45.2% | 65.2% | |
| Bivalirudin | 54.8% | 34.8% | |
| Upstream GpIIb/IIIa use | 11.5% | 13.0% | 0.74 |
| Planned 2 stent approach | 28.1% | 39.1% | 0.34 |
| Final kissing balloon angioplasty | 45.9% | 56.5% | 0.39 |
| SB protected | 73.3% | 87% | 0.21 |
| PGW jailed | 15.9% | 43.4% | 0.003 |
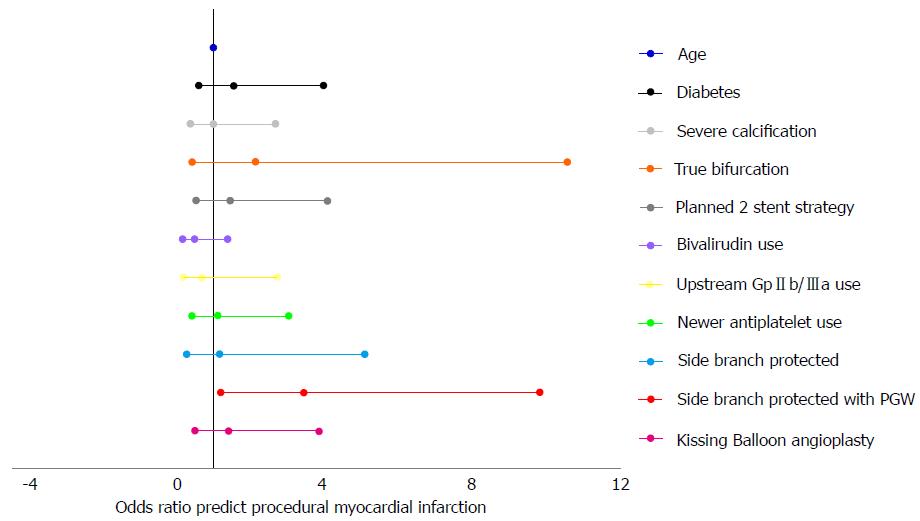
Univariate logistic regression analysis did not reveal any significant association of PMI with age, Diabetes, lesion calcification, use of newer antiplatelet agents, use of Bivalirudin, upstream use of Gp IIb/IIIa use, SB protection, pre-planned use of complex 2 stent strategy or Medina classification as true bifurcation lesion. The use of jailed PGW was strongly associated with PMI with an odds ratio of 4.1 (95%CI: 1.7-9.9; P = 0.002). Performing multivariate logistic regression to adjust for all the aforementioned factors still showed a strong association between jailing of PGW and PMI (Figure 1, Odds ratio 3.5; 95%CI: 1.2-9.9; P = 0.02).
SB protection is of considerable importance during CBL interventions. Occlusion of a SB > 1.0 mm has been associated with a 14% risk of MI[6]. In a large series of 2227 CBL interventions, Hahn et al[7] reported a SB occlusion rate of 8.4% and this increased the rate of major adverse cardiovascular events. The only protective factor found to prevent SB occlusion was the presence of a jailed guide-wire. Similar findings were reported in the Nordic study illustrating the importance of the jailed SB wire[14]. The jailed guide wire provides a physical impediment to closure of the SB ostium and also facilitates re-wiring of the vessel by making the angle between the MV and the SB wider[15]. Thus jailing a wire in the SB during MV stenting is a widely accepted practice for CBL interventions. However there is less consensus on the type of guide-wire to jail.
All coronary guide-wires have some degree of polymer coating on them with varying degrees of polymer cover or jacket. Based on the latter, guide-wires are broadly classified into three categories: (1) Wires with no polymer jacket - minimum lubricity, e.g., HT BMW, Prowater and HT Floppy II; (2) Wires with intermediate polymer jacket - lack polymer jacket at the very distal end only; medium lubricity, e.g., HT BMW Universal, Runthrough NS, Cougar LS; and (3) Wires with full polymer jacket - polymer jacket throughout the length of the wire; maximum lubricity; e.g., HT Whisper, HT Pilot, HT Fielder XT.
PGW (3rd category) offer the attractive quality of lubricity and are easily withdrawn from underneath stent struts. However the interventional community has been wary of these as the initial reports of wire rupture were consistently with hydrophilic PGW[8]. Since then multiple reports of non hydrophilic wires being entrapped have been published as well[16-19]. With the lesser degree of lubricity of a non PGW, greater force may be required to extract the wire and hence risk deep intubation of the guide catheter and injury to the vessel as well.
Some reports have also raised the possibility of shearing of the polymer jacket during extraction of the jailed PGW[20]. Grundeken et al[11] examined the possibility of distal polymer embolization in two ways - they examined the aspirate from patients undergoing aspiration thrombectomy and reported that 45% samples had polymer material in them. Also, examination of autopsy specimens from patients who had undergone PCI showed intramyocardial polymer in 10% subjects. The amount of polymer detected increased as the polymer jacket increased with the maximum embolization noted in cases using HT Whisper wires. This study is especially concerning because polymer embolization occurred even without jailing the guide-wire. It is notable that distal embolization of athero-emboli is considered an important contributor in the etiology of PMI[21] - hence embolization of non-degradable polymer is a plausible hypothetical cause for PMI as well.
To try and quantify the extent of polymer shearing and embolization, we have previously performed a small study examining jailed HT Whisper and Runthrough NS wires with SEM[13]. This revealed polymer shearing in both types of wires but up to 5 fold higher in the HT Whisper, a PGW. Amount of polymer shearing was also weakly correlated with the level of CK MB post procedure. Pan et al[22] randomized 235 patients who underwent CBL interventions with the jailed wire technique to use of PGW or non PGW and examined the jailed wires using an optical microscope. They reported more structural damage to non PGW although no wire fracture was noted. It should be noted though that the study used magnification up to 6.3X only, which is insufficient to detect shearing of polymer and also used wires with no polymer cover as the comparison group, the use of which has gone down in comparison to wires with intermediate polymer cover. Also, the rate of PMI was not different in the two groups.
In this respect, our study is the second study to investigate the relationship of type of wire jailed to PMI. Our results show a strong association of jailed PGW to PMI which are contrary to the results of Pan et al[22]. One reason may be that there are varied reasons why patient have elevated cardiac biomarkers post PCI. Some of these may be no reflow phenomenon, distal athero-embolization, occlusion of SB, coronary perforation, development of cardiogenic (or other types of) shock, access complications causing limb ischemia, arrhythmias, bleeding causing hemodynamic instability, etc. These, at least by our current knowledge of PMI are more likely to be contributors than polymer embolization from jailed PGW. Hence we meticulously excluded all cases which may have had any confounding factor causing a biomarker elevation and categorized these cases as having no PMI. This further strengthens our belief in the credibility of our results.
Our study has all the limitations of a retrospective analysis and the inherent biases. However we have attempted to correct these biases by careful data acquisition, exclusion of cases with potential confounding factors and a multivariate logistic regression analysis. We also note that the definition of PMI used is inconsistent with the 3rd universal definition of MI consensus document[23] which defines PMI as > 5 × ULN of cardiac Troponin (cTn) along with symptoms, electrocardiographic, imaging or angiographic evidence of ischemia. Multiple studies have been done that question the relevance of the 5 × ULN of cTn criterion as a > 3 × ULN of CK-MB cut-off is better correlated with mortality[24] and evidence of new myocardial injury as detected by cardiac MRI[25]. In fact, a cut off of 3 × ULN of CK-MB is equivalent to a cut-offs of 20 × cTn for mortality and 40 × cTn for MRI proven new myocardial injury. Hence while the updated definition is valid in conjunction with clinical evidence of ischemia, CK MB may be a better choice for isolated biomarker analyses.
In conclusion, our study shows that jailed PGW may be associated with a threefold higher risk of PMI. Given the retrospective design, this finding should be treated as hypothesis generating and hopefully will trigger prospective analysis to confirm or refute this association. The etiology for this risk is believed to be polymer shearing and micro-embolization which has been proven by multiple small but rigorously conducted studies[11,13]. We believe that much has to be learned about the potential role of polymer shearing and embolization in myonecrosis post CBL intervention. There is also a need to determine if the wires with intermediate polymer cover may be the best middle path compromise in the argument of lubricity vs fracture and polymer shearing.
Polymer jacketed guide wires (PGW) are frequently used for side branch protection during bifurcation coronary interventions. Their lubricity is an attractive property for this use as it makes them easy to retract from underneath stent struts. However, microscopic shearing of polymer from jailed guide wires has been reported and may be a potential cause of procedural myocardial infarction (PMI) as this may cause distal micro-embolization. Hence, the authors performed a retrospective analysis of bifurcation interventions at this institution to ascertain relationship of PGW use with PMI.
PMI has important prognostic implications in patients undergoing percutaneous coronary intervention. Thus it is important to understand if any procedural factors such as use of PGW have any effect on PMI.
This is only the second study to ascertain if there is a relationship between use of jailed PGW and PMI. In their data there is a strong association of these which translates to a three fold higher risk of PMI if a PGW is jailed.
These results should caution interventional cardiologists from adopting PGW as their go to wire for jailing until prospective data comparing different types of wires are available. Randomized studies are needed to compare newer generation non polymer jacketed, intermediate polymer jacketed and full polymer jacketed coronary guide wires.
PGW: Polymer jacketed guide wires; PMI: Procedural myocardial infarction.
This is an interesting manuscript about the relation of jailing PGW to PMI. The authors demonstrated that jailed PGW might be associated with PMI. This manuscript is nicely structured and well written.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Nunez-Gil IJ, Schoenhagen P, Ueda H S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Lefèvre T, Louvard Y, Morice MC, Dumas P, Loubeyre C, Benslimane A, Premchand RK, Guillard N, Piéchaud JF. Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc Interv. 2000;49:274-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, Sheiban I, Paloscia L, Grube E, Schofer J. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009;119:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 392] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 3. | Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, Bennett L, Holmberg S, Cotton JM, Glennon PE. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121:1235-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 398] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 4. | Maeng M, Holm NR, Erglis A, Kumsars I, Niemelä M, Kervinen K, Jensen JS, Galløe A, Steigen TK, Wiseth R. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J Am Coll Cardiol. 2013;62:30-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 5. | Katritsis DG, Siontis GC, Ioannidis JP. Double versus single stenting for coronary bifurcation lesions: a meta-analysis. Circ Cardiovasc Interv. 2009;2:409-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Arora RR, Raymond RE, Dimas AP, Bhadwar K, Simpfendorfer C. Side branch occlusion during coronary angioplasty: incidence, angiographic characteristics, and outcome. Cathet Cardiovasc Diagn. 1989;18:210-212. [PubMed] |
| 7. | Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, Rha SW, Yu CW, Park JS, Jeong JO. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013;62:1654-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Louvard Y, Lefèvre T, Morice MC. Percutaneous coronary intervention for bifurcation coronary disease. Heart. 2004;90:713-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Latib A, Colombo A. Bifurcation disease: what do we know, what should we do? JACC Cardiovasc Interv. 2008;1:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 195] [Article Influence: 12.2] [Reference Citation Analysis (3)] |
| 10. | Schipper ME, Stella PR, de Jonge N, Virmani R, de Weger RA, Vink A. Embolization of hydrophilic coating material to small intracardial arteries after multiple percutaneous transluminal angioplasty procedures. Int J Cardiol. 2012;155:e45-e46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Grundeken MJ, Li X, Kurpershoek CE, Kramer MC, Vink A, Piek JJ, Tijssen JG, Koch KT, Wykrzykowska JJ, de Winter RJ. Distal embolization of hydrophilic-coating material from coronary guidewires after percutaneous coronary interventions. Circ Cardiovasc Interv. 2015;8:e001816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Owens CG, Spence MS. How should I treat a patient to remove a fractured jailed side branch wire? EuroIntervention. 2011;7:520-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Chatterjee A, Brott BC, Foley R, Alli O, Sasse M, Ahmed M, Al Solaiman F, Reddy G, Ather S, Leesar MA. Safety of hydrophilic guidewires used for side-branch protection during stenting and proximal optimization technique in coronary bifurcation lesions. Cardiovasc Revasc Med. 2016;17:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114:1955-1961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 554] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 15. | Weinstein JS, Baim DS, Sipperly ME, McCabe CH, Lorell BH. Salvage of branch vessels during bifurcation lesion angioplasty: acute and long-term follow-up. Cathet Cardiovasc Diagn. 1991;22:1-6. [PubMed] |
| 16. | Ojeda Delgado JL, Jiménez Mena M, Barrios Alonso V, Pena Tizón J, Fernández Sánchez-Villarán E, Hernández Madrid A, Marín Huerta E, Pey Illera J. [Guide-wire rupture as a complication of coronary angioplasty. Apropos 2 cases and a review of the literature]. Rev Esp Cardiol. 1992;45:141-144. [PubMed] |
| 17. | Sezgin AT, Gullu H, Ermis N. Guidewire entrapment during jailed wire technique. J Invasive Cardiol. 2006;18:391-392. [PubMed] |
| 18. | Bonvini RF, Werner KD, Buettner HJ, Buergelin KH, Zeller T. Retrieval of lost coronary guidewires during challenging percutaneous coronary interventions. Cardiovasc Revasc Med. 2010;11:262.e7-262.10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Balbi M, Bezante GP, Brunelli C, Rollando D. Guide wire fracture during percutaneous transluminal coronary angioplasty: possible causes and management. Interact Cardiovasc Thorac Surg. 2010;10:992-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Pawlowski K, Dorniak W, Klaudel J. Percutaneous evacuation of detached hydrophilic coating of jailed guidewire. J Invasive Cardiol. 2010;22:E193-E195. [PubMed] |
| 21. | Babu GG, Walker JM, Yellon DM, Hausenloy DJ. Peri-procedural myocardial injury during percutaneous coronary intervention: an important target for cardioprotection. Eur Heart J. 2011;32:23-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 22. | Pan M, Ojeda S, Villanueva E, Chavarria J, Romero M, Suarez de Lezo J, Mazuelos F, Segura J, Carrasco F, Hidalgo F. Structural Damage of Jailed Guidewire During the Treatment of Coronary Bifurcation Lesions: A Microscopic Randomized Trial. JACC Cardiovasc Interv. 2016;9:1917-1924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2076] [Cited by in RCA: 2304] [Article Influence: 177.2] [Reference Citation Analysis (0)] |
| 24. | Novack V, Pencina M, Cohen DJ, Kleiman NS, Yen CH, Saucedo JF, Berger PB, Cutlip DE. Troponin criteria for myocardial infarction after percutaneous coronary intervention. Arch Intern Med. 2012;172:502-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 25. | Lim CC, van Gaal WJ, Testa L, Cuculi F, Arnold JR, Karamitsos T, Francis JM, Petersen SE, Digby JE, Westaby S. With the “universal definition,” measurement of creatine kinase-myocardial band rather than troponin allows more accurate diagnosis of periprocedural necrosis and infarction after coronary intervention. J Am Coll Cardiol. 2011;57:653-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |