Published online Feb 26, 2017. doi: 10.4330/wjc.v9.i2.196
Peer-review started: June 16, 2016
First decision: July 11, 2016
Revised: September 14, 2016
Accepted: November 16, 2016
Article in press: November 18, 2016
Published online: February 26, 2017
We describe a case of very late transcatheter heart valve (THV) thrombosis of a first-generation SAPIEN prosthesis (Edwards Lifesciences, Irvine, CA) implanted in a 64-year-old woman with severe symptomatic aortic stenosis. More than 54 mo after implantation, she presented with severe symptomatic prosthesis dysfunction (stenosis) which was successfully treated with oral anticoagulation. To our knowledge, this is the tardiest case of THV thrombosis ever reported. This case should increase clinical awareness for THV thrombosis even beyond the first two-year period following implantation.
Core tip: We describe the tardiest case of transcatheter aortic valve replacement (TAVR) thrombosis ever reported. A 64-year-old woman with severe symptomatic aortic stenosis underwent TAVR with a first-generation SAPIEN prosthesis. More than four years (> 54 mo) following implantation, she presented with a severe symptomatic prosthesis dysfunction (stenosis) which was successfully treated with oral anticoagulation.
- Citation: Couture EL, Lepage S, Masson JB, Daneault B. Very late transcatheter heart valve thrombosis. World J Cardiol 2017; 9(2): 196-199
- URL: https://www.wjgnet.com/1949-8462/full/v9/i2/196.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i2.196
We describe a case of very late transcatheter heart valve (THV) thrombosis of a first-generation SAPIEN prosthesis (Edwards Lifesciences, Irvine, CA) implanted in a 64-year-old woman with severe symptomatic aortic stenosis. More than 54 mo after implantation, she presented with severe symptomatic prosthesis dysfunction (stenosis) which was successfully treated with oral anticoagulation. To our knowledge, this is the tardiest case of THV thrombosis ever reported. This case should increase clinical awareness for THV thrombosis even beyond the first two-year period following implantation.
A 64-year-old woman with severe symptomatic aortic stenosis and porcelain aorta underwent transcatheter aortic valve replacement (TAVR) using a first-generation balloon-expandable Edwards SAPIEN (Edwards Lifesciences, Irvine, CA) 23 mm THV in January 2011. The patient was discharged home with aspirin and clopidogrel for three months followed by low dose aspirin.
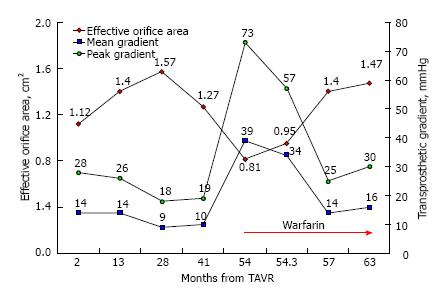
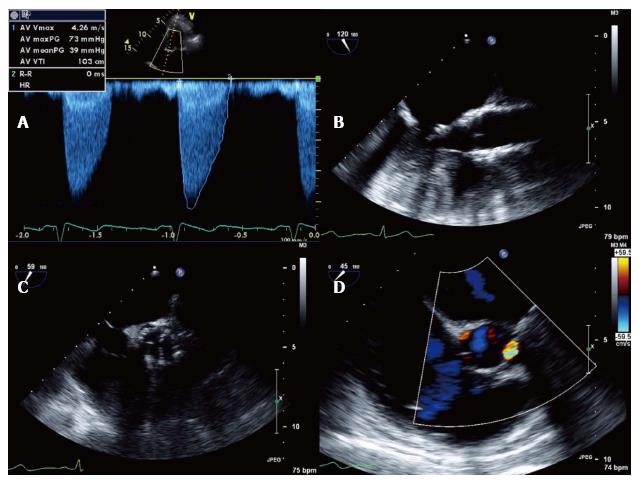
More than 54 mo following TAVR, she presented with progressive dyspnea, angina and dizziness on moderate exertion. Transthoracic echocardiogram (TTE) revealed a severe THV dysfunction with an aortic valve area (AVA) of 0.81 cm2, peak and mean trans prosthetic gradients (TPG) of 76 and 39 mmHg respectively and a preserved left ventricular ejection fraction (Figure 1). Transesophageal echocardiogram (TEE) did not demonstrate abnormal leaflet function neither THV thrombosis (Figure 2) but revealed a moderate paravalvular leak (PVL) (Figure 2D) already known from the immediate post-TAVR TEE. THV thrombosis was suspected given the absence of other explanatory findings and the abrupt progression of TPG. Therefore, anticoagulation with warfarin and unfractionated heparin was empirically started. A coronary angiogram and a cardiovascular magnetic resonance (CMR) were also performed. Angiogram revealed a severe, non-thrombotic, left main mid-shaft stenosis and percutaneous coronary intervention (PCI) with a drug-eluting stent was performed. CMR revealed an aortic regurgitation fraction of 23% consistent with the moderate PVL previously seen on the TEE. No evidence of THV thrombosis other than elevated peak velocity was detected on CMR. Nine days after initiation of anticoagulation, a repeat TTE showed mild improvement in TPG (Figure 1). The patient was discharged home with aspirin, clopidogrel and warfarin for three months, followed by clopidogrel and warfarin. Angina was relieved immediately after PCI, but dyspnea on exertion improved over weeks. After three months, symptoms had resolved completely and TPG returned to their baseline values. They remained unchanged after nine months under chronic anticoagulation (Figure 1).
In two series, less than 30 cases of THV thrombosis have been reported with a median presentation time of 6 mo (range, 3-735 d) with only two cases occurring beyond one year[1,2]. A case of a Direct Flow Medical THV thrombosis three years following TAVR has also been reported recently[3]. To our knowledge, never a THV thrombosis has been described so late after implant (> 54 mo) as in this case. THV thrombosis is a new entity that needs to be recognized not only by TAVR specialists. Even though estimated incidence is low (0.61%), consequences can be catastrophic if appropriate therapy is not initiated promptly[1]. Only reported cases treated with anticoagulation had favorable outcome. Therefore, a sudden increase in TPG should trigger further investigation or therapies to exclude THV thrombosis. Valve hemodynamic deterioration (VHD), defined by an increase in mean TPG of more than 10 mmHg over time, was observed more frequently in patients with smaller THV (23 mm) and those not receiving oral anticoagulation[4]. Most of these patients did not have a progressive deterioration after the first year. VHD does not seem to be part of a continuum towards THV thrombosis and this later remains unpredictable. However, the pathophysiology of VHD may include some degree of sub-clinical leaflet thrombosis.
In our case, TEE evaluation was not diagnostic. In a series of 3 pathology-proven THV thrombosis, TEE was also negative in each cases[2]. However, Makkar et al[5] showed that 4D-CT and TEE had a diagnostic concordance of 100% in 10 patients presenting reduced leaflets motion following TAVR. Whether 4D-CT is the optimal imaging modality remains to be proven. CMR was chosen over CT scan to assess PVL severity but also failed to identify the THV thrombosis. Therefore, negative imaging should not preclude an anticoagulation trial when the diagnostic is highly suspected.
Reports have revealed subclinical leaflet thrombosis detected by TEE and 4D CT scan early after THV implantation[5]. Most of these cases were seen in patients who did not receive anticoagulation. The clinical significance of these findings remains unknown at this point. Studies are ongoing to evaluate the optimal antiplatelet/anticoagulant therapy after TAVR. The ARTE (clopidogrel; NCT01559298) and REAC-TAVI (ticagrelor vs clopidogrel; NCT02224066) trials are evaluating different antiplatelet strategies and the GALILEO (rivaroxaban; NCT02556203) and ATLANTIS (apixaban; NCT02664649) studies are looking at the effect of non-vitamin K oral anticoagulant following TAVR. Similarly, the POPular-TAVI trial (NCT02247128) is evaluating the effect of adding clopidogrel for 3 mo following implantation in patients with and without ongoing vitamin-K oral anticoagulation treatment.
This case is also particular because of the concurrent left main stenosis. Although thrombus migration in the left main could be considered an explanation, the angiographic appearance was more in favor of disease progression of a previous non-significant lesion seen on the pre-TAVR angiogram. Moderate PVL could be associated with a different flow pattern over the leaflets and in the left main that could lead to THV thrombosis as well as accelerated progression of atherosclerosis although this relationship is speculative.
This case should increase clinical awareness for THV thrombosis even beyond the first two-year period following implantation. Risk predictors for THV thrombosis and optimal antiplatelet/anticoagulant therapy post TAVR are still unknown and warrants clinical trials.
More than 54 mo following transcatheter aortic valve replacement, a 64-year-old woman presented with progressive dyspnea, angina and dizziness on moderate exertion.
Prosthesis dysfunction.
Transcatheter heart valve (THV) degeneration; THV thrombosis; THV endocarditis.
Transesophageal echocardiogram (TEE) revealed a prosthesis dysfunction with a severe stenosis. TEE failed to revealed THV thrombosis as well as vegetations.
Empiric treatment with unfractionated intravenous heparin followed by long-term anticoagulation with warfarin.
Less than 30 cases of THV thrombosis have been reported with a median presentation time of 6 mo (range, 3-735 d) with only two cases occurring beyond one year.
This case should increase clinical awareness for THV thrombosis even beyond the first two-year period following implantation. Even if TEE does not reveal THV thrombosis.
The paper is well written.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Grignola JC, Kettering K, Paradis JM, Said SAM, Vermeersch P S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Latib A, Naganuma T, Abdel-Wahab M, Danenberg H, Cota L, Barbanti M, Baumgartner H, Finkelstein A, Legrand V, de Lezo JS. Treatment and clinical outcomes of transcatheter heart valve thrombosis. Circ Cardiovasc Interv. 2015;8:e001779. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 2. | De Marchena E, Mesa J, Pomenti S, Marin Y Kall C, Marincic X, Yahagi K, Ladich E, Kutz R, Aga Y, Ragosta M. Thrombus formation following transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2015;8:728-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 133] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 3. | Regazzoli D, Ancona MB, Mangieri A, Agricola E, Spagnolo P, Mussardo M, Colombo A, Latib A. A Case of Very Late (3 Years) Transcatheter Heart Valve Thrombosis. JACC Cardiovasc Interv. 2016;9:e83-e84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Del Trigo M, Muñoz-Garcia AJ, Wijeysundera HC, Nombela-Franco L, Cheema AN, Gutierrez E, Serra V, Kefer J, Amat-Santos IJ, Benitez LM. Incidence, Timing, and Predictors of Valve Hemodynamic Deterioration After Transcatheter Aortic Valve Replacement: Multicenter Registry. J Am Coll Cardiol. 2016;67:644-655. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 183] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 5. | Makkar RR, Fontana G, Jilaihawi H, Chakravarty T, Kofoed KF, de Backer O, Asch FM, Ruiz CE, Olsen NT, Trento A. Possible Subclinical Leaflet Thrombosis in Bioprosthetic Aortic Valves. N Engl J Med. 2015;373:2015-2024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 782] [Cited by in F6Publishing: 738] [Article Influence: 82.0] [Reference Citation Analysis (0)] |