CASE REPORT
A 71-year-old male had felt chest oppression on effort, such as when carrying heavy baggage, for 1 year. Recently, his chest symptoms had occurred more frequently. One month before admission he felt chest squeezing at rest in the early morning. He presented at our institution for an evaluation of his chest symptoms in May 2014. Coronary risk factors such as smoking, hypertension, and diabetes mellitus were all absent, although he had a low level of high-density lipoprotein (HDL) cholesterol. His mother had angina pectoris. He had undergone operations for appendicitis and prostate cancer at the ages of 25 and 69 years, respectively. On medical examination, his height was 1.63 m, his weight was 73 kg, and his body mass index was 27.5. His vital signs were stable with a blood pressure of 110/80 mmHg and a pulse of 59 beats/min. No cardiac murmur or abnormal respiratory sounds in the lungs were detected. Blood examinations revealed elevated levels of creatinine (1.06 mg/dL), uric acid (9.4 mg/dL), and triglycerides (227 mg/dL), and a low level of HDL cholesterol (35 mg/dL). Neither a chest X-P, electrocardiogram, nor echocardiography showed any specific changes. He was admitted to our institution for coronary angiography (CAG) because of the possibility that his chest symptoms were due to myocardial ischemia.
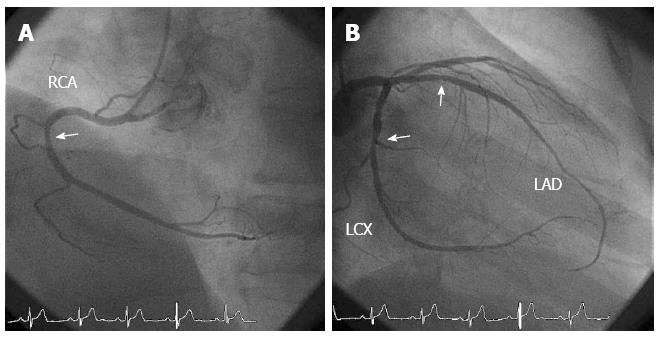
An initial CAG showed mild atherosclerotic changes at the proximal segments of the right coronary artery (RCA), the left anterior descending coronary artery (LAD) and the mid-segment of the left circumflex coronary artery (Figure 1). To clarify the cause of his chest symptoms, we performed spasm provocation testing using acetylcholine (ACh). During the spasm provocation test, a pressure wire (PrimeWire Prestige PLUS, Volcano Therapeutics Inc., Rancho Cordova, CA, USA) was inserted into the distal portion of the RCA and distal portion of the LAD. The ratio of the distal pressure, derived from the pressure wire, to the proximal one, derived from the tip of catheter (Pd/Pa), was continuously monitored.
Figure 1 Coronary angiography before spasm provocation tests.
A: There were mild atherosclerotic changes at the proximal segment of the right coronary artery (RCA); B: There were mild atherosclerotic changes at the proximal segment of the left anterior descending coronary artery (LAD) and at the mid-segment of the left circumflex coronary artery (LCX). The mild atherosclerotic changes are indicated using arrows.
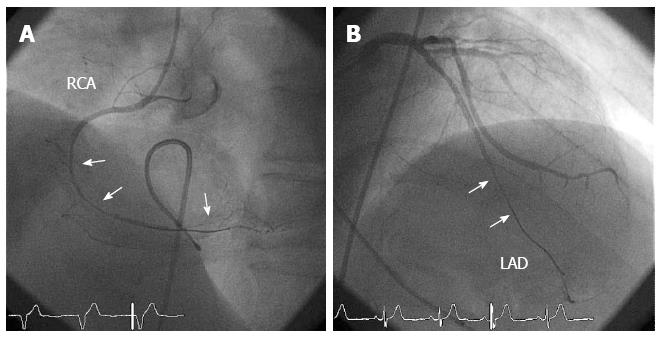
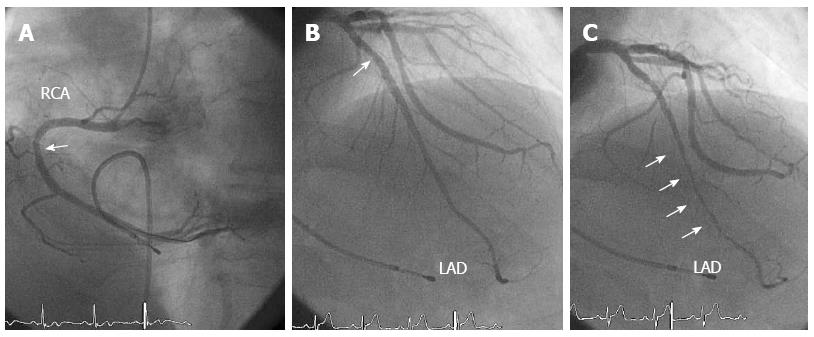
Intracoronary infusion of 50 μg ACh caused a diffuse coronary spasm at the mid-distal portion of the RCA (Figure 2A), which was accompanied by the usual chest symptoms and a reduction in the Pd/Pa from 1.0 to 0.69 at baseline. Because of the prolonged coronary spasm, 600 μg nitroglycerin (NTG) was intracoronarily administered, which relieved the coronary spasm in the RCA (Figure 3A). The subsequent intracoronary infusion of 100 μg ACh in the LCA resulted in no chest symptoms but a diffuse spasm in the mid-distal portion of the LAD (Figure 2B), which was accompanied by a reduction in the Pd/Pa from 0.94 to 0.60 at baseline. The intracoronary infusion of 300 μg NTG relieved the coronary spasm and returned the Pd/Pa to the baseline value of 0.94. A final CAG revealed an MB of the mid-distal segments of the LAD (Figures 3B and C). The length and percent systolic narrowing of the MB segment was 38 mm and 78%, respectively. The fractional flow reserve (FFR) of the LAD, which was assessed using a pressure wire and the intravenous administration of 160 μg/min per kilogram adenosine triphosphate (ATP), was positive at 0.77 from 0.94 at baseline (Figure 4A). It then jumped to 0.90 through the MB segments when the pressure wire was pulled back (Figure 4B). Therefore, multi-vessel coronary spasms and a myocardial bridge may contribute to his chest symptoms at rest and during effort. The following day he was discharged and prescribed diltiazem (300 mg/d). Since then, he has been taking 300 mg/d diltiazem and 15 mg/d nicorandil and his symptoms have been controlled in the outpatient clinic.
Figure 2 Coronary angiography during the spasm provocation tests.
A: In the right coronary artery (RCA), a diffuse coronary spasm occurred at the mid-distal segments after the intracoronary infusion of 50 μg acetylcholine (ACh); B: In the left coronary artery, a diffuse coronary spasm occurred at the mid-distal segments of the left anterior descending coronary artery (LAD) after the intracoronary infusion of 100 μg ACh. The coronary spasm segments are indicated using arrows.
Figure 3 Coronary angiography after the intracoronary infusion of nitroglycerin.
A: There was a mild atherosclerotic change at the proximal segment of the right coronary artery (RCA); B: There was a mild atherosclerotic change (indicated with arrows) in the proximal segment of the left anterior descending coronary artery (LAD) at the end-diastolic phase; C: There was myocardial bridging (indicated with arrows) at the mid-distal segments of the LAD at the end-systolic phase.
Figure 4 The fractional flow reserve using the intravenous infusion of adenosine triphosphate was 0.
77 (A), which jumped up to 0.90 through the myocardial bridging during pullback (B).
DISCUSSION
In this study, we present a case of angina pectoris both during exercise and at rest. These symptoms were due to bilateral coronary spasms and MB-related myocardial ischemia, which was identified using a pressure wire.
Several reports have described MB-related myocardial infarction[14-17] and sudden cardiac death[18-20]. Myocardial ischemia has been suggested to be the main cause of MB-related cardiac events due to mechanical compression of the coronary artery by the MB[21,22] and/or coronary spasm at the MB segments[12,23-25]. It is possible that coronary spasms frequently occur at MB segments because of endothelial dysfunction and/or vascular dysfunction of the coronary artery at MB segments[11,12]. Although the current case had multivessel coronary spasms, the segment of the LAD that underwent coronary spasm was the same as the MB segment, which is consistent with an MB-related coronary spasm. This suggests that cardiologists should consider the possibility of coronary spasm in patients with chest pain and MB on coronary angiograms. Several methods have been used to assess MB-related myocardial ischemia due to mechanical compression of the coronary artery by MB, such as pharmacological stress echocardiography[26], stress myocardial perfusion imaging[27], intracoronary blood flow velocity measurements[21,26], and intracoronary pressure measurements[1,21,26,28]. In the current case, we assessed intracoronary pressure using a pressure wire because this technique has a reliable cutoff value[29] and can be used conveniently in the clinical setting.
Regarding the relationship between intracoronary pressure and MB, reports describing the pressure gradient within the MB segment vary. For example, it has been reported that a pressure gradient within the MB segment is present even at baseline[21], only during pharmacological stress[1,26,28], only within the MB segment[26], or both within and beneath MB[1,21,28]. These different results may have been due to differences in the severity and degree of the MB itself as well as differences in the methods used to measure intracoronary pressure. According to the current results, where Pd/Pa was 0.94 and FFR was 0.77 at baseline and the Pd/Pa increased to 0.90 through the MB segments, a pressure gradient was present only during pharmacological stress and within and beneath the MB.
ATP is used frequently to measure FFR in the clinical setting during the assessment of MB. However, it has been reported that dobutamine is more useful as the stress agent during the assessment of MB[1,26,28] because it causes a more severe and longer compression within the MB[28]. Assessing the FFR of the vessel containing the MB can be challenging[30] because atherosclerotic changes often occur proximal to the MB[1], which may reduce FFR. The present case had a minor atherosclerotic lesion proximal to the MB; however, the FFR increased to 0.90 just proximal to the MB when the pressure wire was pulled back. Therefore, in cases with MB and proximal atherosclerotic lesions, assessing FFR using the combination of the pullback method may be more useful.
β-blockers are the mainstay of treatment for symptomatic patients with MB[1]. However, as shown in the present case, coronary spasms sometimes occur in patients with MB, particularly in the MB segments[12]. In general, monotherapy using β-blockers is prohibited in patients with coronary spasms[31]. Furthermore, the use of NTG, which is very effective for relieving coronary spasms, may exacerbate the systolic narrowing of the MB segments[32]. Therefore, it is important to ascertain the presence of coronary spasms in patients with MB. Furthermore, in cases with both MB and coronary spasms, calcium-channel blockers (CCB) or CCB plus β-blockers may be useful. Patients with coronary spasms and MB should be monitored carefully when these drugs are administered. In the present case, CCB with diltiazem plus nicorandil was used to treat the coronary spasm, which was the main pathology in the present case. When chest symptoms are present during exercise the use of β-blockers should be considered. It was reported that percutaneous coronary intervention is useful to relieve chest symptoms in patients with MB[1,22,30,33]; however, it was also reported that the incidence restenosis is relatively high[1,30]. Therefore, pharmacological treatment should be used even in patients with MB and a significantly reduced FFR.
In conclusion, coronary spasms sometimes consolidate in patients with MB, and the presence of coronary spasms should be assessed in such patients. In addition, intracoronary pressure measurements using a pressure wire may be useful to assess the severity of MB. Interventional cardiologists should keep these concepts in mind.
COMMENTS
Case characteristics
A 71-year-old male presented chest oppression during effort and chest squeezing at rest.
Clinical diagnosis
Angina pectoris due to coronary spasm and myocardial bridging.
Differential diagnosis
Angina pectoris due to significant coronary stenosis, pulmonary thromboembolism.
Laboratory diagnosis
Elevated levels of creatinine (1.06 mg/dL), uric acid (9.4 mg/dL), and triglycerides (227 mg/dL), and a low level of HDL cholesterol (35 mg/dL).
Imaging diagnosis
Coronary angiography showed mild atherosclerotic changes. Spasm provocation testing using acetylcholine showed multi-vessel coronary spasms. Coronary angiography after an intracoronary infusion of nitroglycerin showed myocardial bridging of the left anterior descending coronary artery. The fractional flow reserve using adenosine triphosphate was positive at 0.77.
Treatment
The patient was treated with 300 mg/d diltiazem and 15 mg/d nicorandil.
Related reports
Angina pectoris due to coronary spasms or myocardial bridging is well-known, however, little has been reported regarding angina pectoris at rest and during effort due to both coronary spasms and myocardial bridging.
Term explanation
Myocardial bridging is an anomaly in which the myocardium overlies the intramural course of segments of the epicardial coronary arteries and is associated with cardiac events.
Experiences and lessons
This report presents a case of angina pectoris due to coronary spasm and myocardial bridging. Coronary spasms sometimes consolidate in patients with myocardial bridging, and the presence of coronary spasms should be assessed in such patients. In addition, intracoronary pressure measurements using a pressure wire may be useful to assess the severity of myocardial bridging.
Peer-review
This is an interesting case. The case is well presented and the text well written.