Copyright
©The Author(s) 2015.
World J Cardiol. Dec 26, 2015; 7(12): 829-842
Published online Dec 26, 2015. doi: 10.4330/wjc.v7.i12.829
Published online Dec 26, 2015. doi: 10.4330/wjc.v7.i12.829
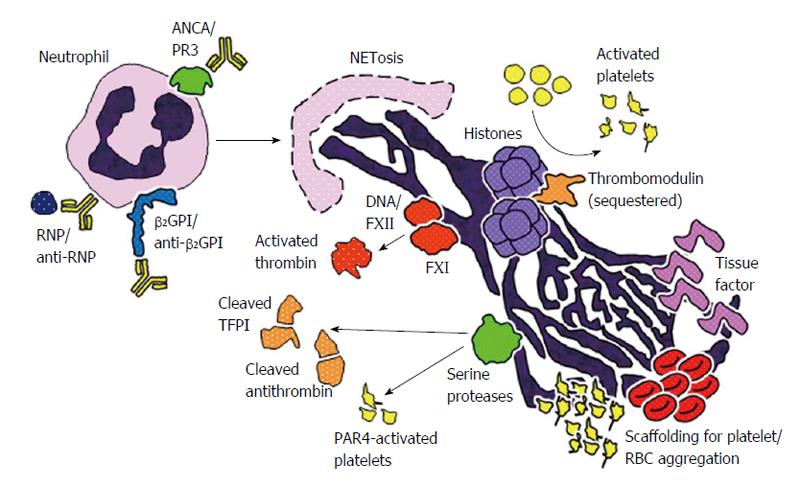
Figure 1 Schematic representation of potential mechanisms by which neutrophil extracellular traps may promote thrombosis in systemic autoimmune diseases.
First, a number of stimuli may promote NETosis in systemic autoimmune diseases including ribonucleoprotein (RNP)/anti-RNP complexes in systemic lupus erythematosus, anti-neutrophil cytoplasmic antibody (ANCA) engagement with surface proteinase 3 (PR3) in vasculitis, and the interaction of anti-beta-2 glycoprotein I (β2GPI) with surface β2GPI in antiphospholipid syndrome. The DNA component of NETs activates factor XII (FXII), initiating a cascade (along with factor XI) that ultimately leads to the formation of thrombin. Histones in NETs activate platelets and sequester certain anticoagulant molecules like thrombomodulin and protein C. Neutrophil serine proteases present in NETs, such as neutrophil elastase and cathespin G, cleave the anticoagulant molecules tissue factor pathway inhibitor (TFPI) and antithrombin, and also activate platelets through various pathways including protease-activated receptor 4. NETs also may present procoagulant tissue factor in some contexts. Finally, NETs serve as scaffolding for the assembly and aggregation of platelets and red blood cells (RBCs). NET: Neutrophil extracellular trap.
- Citation: Rao AN, Kazzaz NM, Knight JS. Do neutrophil extracellular traps contribute to the heightened risk of thrombosis in inflammatory diseases? World J Cardiol 2015; 7(12): 829-842
- URL: https://www.wjgnet.com/1949-8462/full/v7/i12/829.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i12.829