Published online Nov 26, 2015. doi: 10.4330/wjc.v7.i11.801
Peer-review started: February 9, 2015
First decision: June 4, 2015
Revised: September 9, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: November 26, 2015
Processing time: 294 Days and 11.5 Hours
AIM: To compare the atrio-ventricular (AV/PV) delay optimization by echocardiography and intra-cardiac electrocardiogram (IEGM) based QuickOpt algorithm in complete heart block (CHB) patients, implanted with a dual chamber pacemaker.
METHODS: We prospectively enrolled 20 patients (age 59.45 ± 18.1 years; male: 65%) with CHB, who were implanted with a dual chamber pacemaker. The left ventricular outflow tract velocity time-integral was measured after AV/PV delay optimization by both echocardiography and QuickOpt algorithm method. Bland-Altman analysis was used for agreement between the two techniques.
RESULTS: The optimal AV and PV delay determined by echocardiography was 155.5 ± 14.68 ms and 122.5 ± 17.73 ms (P < 0.0001), respectively and by QuickOpt method was 167.5 ± 16.73 and 117.5 ms ± 9.10 ms (P < 0.0001), respectively. A good agreement was observed between optimal AV and PV delay as measured by two methods. However, the correlation of the optimal AV (r = 0.0689, P = 0.77) and PV (r = 0.2689, P = 0.25) intervals measured by the two techniques was poor. The time required for AV/PV optimization was 45.26 ± 1.73 min by echocardiography and 0.44 ± 0.08 min by QuickOpt method (P < 0.0001).
CONCLUSION: The programmer based IEGM method is an automated, quick, easier and reliable alternative to echocardiography for the optimization of AV/PV delay in CHB patients, implanted with a dual chamber pacemaker.
Core tip: Optimization of sensed and paced atrio-ventricular (AV/PV) delay is required for better hemodynamics in patients with complete heart block (CHB). Aim of the present study was to compare the AV/PV delay optimization by echocardiography and intra-cardiac electrocardiogram (IEGM) based QuickOpt algorithm in patients with CHB. We prospectively enrolled 20 patients of CHB who were implanted with a dual chamber pacemaker. A velocity time-integral of left ventricular outflow tract was measured following AV/PV delay optimization by both echocardiography and QuickOpt algorithm method. An agreement between the two techniques was assessed by Bland-Altman analysis. Optimal AV and PV delay as assessed by echocardiography was 155.5 ± 14.68 ms and 122.5 ± 17.73 ms (P < 0.0001), respectively and by QuickOpt method was 167.5 ± 16.73 ms and 117.5 ± 9.10 ms (P < 0.0001), respectively. The time required for AV/PV optimization was 45.26 ± 1.73 min by echocardiography and 0.44 ± 0.08 min by QuickOpt method (P < 0.0001). In conclusion, automated programmer based IEGM method is a quick, easy and reliable alternative to echocardiography for optimization of AV/PV delay in CHB patients.
- Citation: Vijayvergiya R, Gupta A. Comparison of echocardiography and device based algorithm for atrio-ventricular delay optimization in heart block patients. World J Cardiol 2015; 7(11): 801-807
- URL: https://www.wjgnet.com/1949-8462/full/v7/i11/801.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i11.801
Pacemaker therapy provides a better hemodynamics in addition to pacing support in patients with bradycardia and complete heart block (CHB). A programmed atrio-ventricular (AV) interval is crucial for adequate diastolic filling, optimal cardiac output and prevention of diastolic mitral regurgitation[1]. Optimal AV delay can be assessed by Doppler diastolic flow measurement across mitral valve, or by an invasive left ventricular pressure measurement. An automated intra-cardiac electrogram (IEGM) algorithm known as “QuickOpt” from St Jude Medical, St Paul, MN, United States has the capability to assess the optimal AV delay in implanted patient[2-4]. QuickOpt algorithm is a good alternative to the standard echocardiographic method for optimal AV delay assessment. A good correlation have been demonstrated between optimal AV/PV and inter-ventricular (VV) intervals in patients with cardiac resynchronization therapy (CRT) as assessed by echocardiography and QuickOpt method[3,4]. We have compared echocardiography and QuickOpt method for AV/PV delay optimization in patients of CHB, who were implanted with dual chamber pacemaker.
It was a prospective, single center, non-randomized, open-label, pilot study. The institute’s ethics committee approval was taken prior to initiation of the study. Twenty consecutive patients of CHB who underwent pacemaker implantation (DDDR Mode, Zephyr XL DR 5826, St Jude Medical, United States) from July 2010 to December 2011 were enrolled in the study. Patients with low intrinsic atrial rate of < 40 bpm, NYHA functional class IV heart failure, permanent or persistent atrial flutter or atrial fibrillation, significant valvular heart disease, pregnancy, age < 18 years, and those enrolled in another study were excluded. All patients underwent optimization of the AV/PV delay by echocardiography and QuickOpt algorithm after at least 8 wk of pacemaker implantation. The order of measurement of the two tests was randomized with the help of a computer generated random number table. A stopwatch was used for time interval measurements for both the optimization methods.
Echocardiography method: AV delay optimization was performed using two-dimensional Doppler echocardiography on iE33 ultrasound system (Philips Medical Systems, WA, United States). A sweep speed of 100 mm/s was used. Doppler measurements were taken at a delay of 30 s after programming new AV and PV intervals. Optimal AV interval was determined in DVI pacing mode, while optimal PV interval was measured in VDD pacing mode. To pace atria in DVI mode, the atrial rate was increased by 10 beats per minute over the baseline atrial rate. Mitral inflow velocity was measured in the apical four-chamber view. First measurement of mitral inflow duration (both diastolic E and A wave duration) was taken at a long AV delay of > 200 ms. Thereafter, AV interval was decreased by 10 ms each time and simultaneously EA duration was measured, during end expiration. An average of three consecutive beats during expiration was taken for EA measurement. The optimal AV/PV interval by echocardiography was the AV/PV interval at which the maximum transmitral inflow duration was documented without the interruption of A wave[5,6]. A velocity time-integral (VTI) of left ventricular outflow tract (LVOT) was measured in an apical five chamber view and an average of three beats was taken. It was measured for each of a programmed AV/PV delay. Measurement by a single echocardiographer (author - Gupta A) ruled out inter-observer bias. Taking measurements of pulsed wave Doppler at fixed points (mitral valve leaflet tips for transmitral inflow duration and 1 cm below the aortic valve for VTI of LVOT) minimized intra-observer bias.
Optimal AV interval was measured by intra-cardiac electrocardiogram (IEGM) method using a St Jude Medical programmer (QuickOpt algorithm in MerlinTM Patient Care System Programmer, St Jude Medical, CA, United States)[2,4]. This algorithm calculates the optimal PV delay by measuring the width of atrial IEGM and adding 30 ms if intrinsic atrial depolarization of ≥ 100 ms and adding 60 ms if intrinsic atrial depolarization is < 100 ms. The off-set factor enables delivery of ventricular pacing after atrial electrical activation and mechanical contraction are completed. An optimal AV delay was calculated as the sum of optimal PV delay and the pacing latency (50 ms). At each AV interval, LVOT VTI was assessed as per the method described above.
Continuous variables are expressed as mean and standard deviation, and categorical variables are expressed as counts. Bland-Altman plots was used for agreement between the two optimization techniques[7-9]. These plots depict the mean difference and 95%CI of the differences (mean difference ± 2 SD of difference). A difference of > 20 ms in the AV or PV interval assessed by two optimization techniques was interpreted as poor agreement[2]. For LVOT VTI, a difference of > 2 cm was considered significant for a poor agreement[2]. Correlation between the two techniques was evaluated using linear regression analysis and Pearson’s correlation coefficient. A P value of < 0.05 was regarded significant. Comparison of LVOT VTI was done using the paired-sample Student’s t test. Statistical analysis was carried out by Statistical Analysis System SAS 17 and Medcalc Medical Calculator.
Thirty CHB patients had dual chamber pacemaker (Zephyr XL DR 5826 model of St Jude Medical, United States) implantation from July 2010 to December 2011. Twenty eligible patients were included in the study. Ten excluded patients had permanent/persistent atrial flutter or atrial fibrillation (n = 6), slower intrinsic atrial activity of less than 40 bpm (n = 2) or NYHA Class IV heart failure (n = 2). The mean age of 20 enrolled patients was 59.45 ± 18.1 years; 13 were males and 7 were females. Seventeen patients had degenerative CHB and 3 had congenital CHB. Presenting complaint of syncope or pre-syncope was present in 17 patients. The mean left ventricular ejection fraction was 59.25% ± 7.8%.
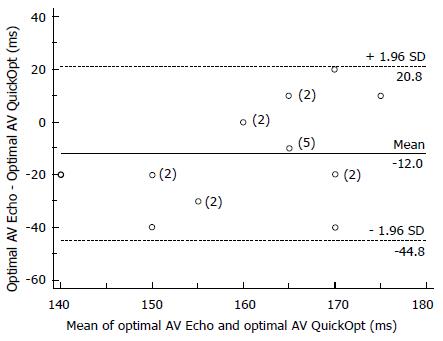
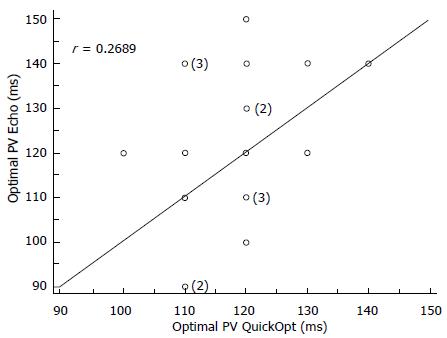
The optimal AV and PV delay determined by echocardiography was 155.5 ± 14.68 ms and 122.5 ± 17.73 ms, respectively and by QuickOpt was 167.5 ± 16.73 ms and 117.5 ± 9.10 ms, respectively (Table 1). The optimal PV delay was significantly shorter than optimal AV delay by both echocardiography and QuickOpt algorithm (P < 0.0001). Mean time required for optimisation for AV/PV delay was 45.26 ± 1.73 min by echocardiography and 0.44 ± 0.08 min by QuickOpt algorithm, P < 0.0001 (Table 2). There was a good agreement between optimal AV delays as assessed by the two techniques. Only 4-patients had > 20 ms difference in optimal AV interval (Figure 1). However, correlation of the optimal AV intervals assessed by two techniques was poor (Figure 2; r = 0.0689, P = 0.77). There was a good agreement of optimal PV delay with just 4-patients having > 20 ms difference in the optimal PV interval (Figure 3) and a poor correlation between the two techniques (Figure 4; r = 0.2689, P = 0.25).
| Optimal AV delay(in ms) | Optimal PV delay(in ms) | P value | |
| Echocardiography | 155.5 ± 14.68 (130-180) | 122.5 ± 17.73 (90-150) | < 0.0001 |
| QuickOpt | 167.5 ± 16.73 (150-190) | 117.5 ± 9.10 (100-140) | < 0.0001 |
| Echocardiography | QuickOpt | P value | |
| LVOT VTI at optimal AV delay (cm) | 18.86 ± 4.11 (11.6-27.7) | 17.82 ± 4.02 (11.46-27.7) | 0.0099 |
| LVOT VTI at optimal PV delay (cm) | 19.26 ± 3.01 (13.7-23.9) | 18.5 ± 2.92 (13.8-23.9) | 0.07 |
| Time required for optimization (min) | 45.26 ± 1.73 (41.5-48.1) | 0.44 ± 0.08 (0.31-0.57) | < 0.0001 |
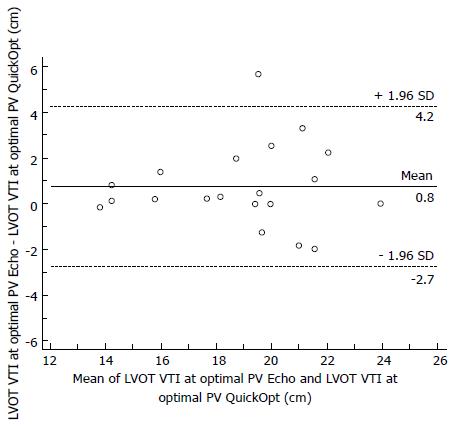
Mean LVOT VTI at optimal AV delay was 18.86 ± 4.11 cm by echocardiography and 17.82 ± 4.02 cm by QuickOpt algorithm (P = 0.0099, Table 2), suggesting a better hemodynamic response by echocardiography. Similarly, mean LVOT VTI at optimal PV delay was 19.26 ± 3.01 cm by echocardiography and 18.5 ± 2.92 cm by QuickOpt algorithm (P = 0.07), suggesting a trend towards better hemodynamic response by echocardiography (Table 2). There was a good clinical agreement between LVOT VTI at optimal AV delay assessed by these two techniques, with 4-patients having > 2 cm difference in the LVOT VTI (Figure 5). Also, the correlation of LVOT VTI measured at optimal AV delay was good by two techniques (r = 0.9216, P < 0.0001). Similarly, there was a good agreement between LVOT VTI at optimal PV delay determined by these two techniques, with just 4 of 20 patients having more than 2 cm difference in the LVOT VTI (Figure 6) and a good correlation of LVOT VTI as assessed at optimal PV delay by two techniques (r = 0.8218, P < 0.0001).
The present study has demonstrated a good agreement and poor correlation between optimal AV and PV delay as assessed by echocardiography and QuickOpt algorithm in patients with CHB. There was also a good agreement and good correlation of LVOT VTI as determined at optimal AV and PV delay by two techniques. Various studies had shown a good correlation between LVOT VTI as determined by echocardiography and QuickOpt algorithm in patients with heart failure on CRT[3,4]. Gold et al[10], demonstrated an excellent correlation between the IEGM method and the maximum achievable invasive LV dP/dt measurement during CRT implantation in both AV and PV modes. Baker et al[3], studied AV/PV and VV delay optimization in heart failure patients implanted with a CRT-D or dual chamber ICD. They measured maximum LVOT VTI guided by echocardiography and QuickOpt algorithm. The concordance correlation coefficient between echocardiography and QuickOpt method for AV, PV and VV delays was 97.5%, 96.1%, and 96.6%, respectively (P < 0.05). Kamdar et al[2], studied AV and VV delay optimization in CRT patients by echocardiography and QuickOpt method. There was a good correlation of two methods for LVOT VTI optimization (R2 = 0.77, P < 0.001), though it was significantly better (P≤ 0.001) with echocardiography compared to QuickOpt method. However, an agreement between the two methods was poor, with 15 out of 26 patients had > 20 ms difference in optimal AV interval and 10 out of 26 patients had > 20 ms difference in the optimal VV interval. The frequent optimization study using the QuickOpt method (FREEDOM trial) studied benefits of frequent AV/PV and VV delay optimisation using the QuickOpt algorithm vs standard of care (physician guided programming or upto 1 non IEGM based optimization like echocardiography within first 4 wk) in 1647 patients implanted with CRT[4]. This trial observed that QuickOpt optimization was as good as the standard of care programming methods which includes either physician guided or non-IEGM optimization methods by echocardiography. In the present study, there was a poor correlation between optimal AV and PV delay but good correlation between LVOT VTI at optimal AV/PV delay as assessed by echocardiography and QuickOpt algorithm. This is attributed to small changes in hemodynamics (measured by LVOT VTI) caused by large variations in AV/PV intervals.
AV synchrony provides hemodynamic benefit in addition to pacing support in CHB patients. An appropriately timed atrial systole prevents rise in mean atrial pressure, facilitates venous return, coordinates AV valve closure; thus reduces diastolic mitral regurgitation and reduces pulmonary capillary wedge pressure[11,12]. The fact that optimal AV delay results in maximum cardiac output, and small deviations can decrease cardiac output has been demonstrated in various previous studies[1,13]. Various echocardiography studies have reported optimal AV delay of 125-200 ms, and an optimal PV delay of 30-50 ms shorter to optimal AV delay[1,5,6]. Similar mean AV/PV delay was observed in present study. Janosik et al[1] studied Doppler derived cardiac output in 24 patients implanted with dual chamber pacemaker. The optimal delay interval during DVI and VDD pacing was 176 ± 44 and 144 ± 48 ms (P < 0.002), respectively. They demonstrated 8% increment in resting cardiac output with optimal AV delay; while same delay with paced P wave (PV delay) did not show maximum cardiac output. Kindermann et al[5] documented optimal AV and PV delay in 53 high degree AV block patients as 136 ± 34 ms and 76 ± 40 ms, respectively. They also reported that AV delay optimization results in 19% increase in stroke volume, compared to fixed AV delay. Similarly, Ritter et al[6] reported an optimal AV and PV delay of 179 ± 25 ms and 124 ± 18 ms, respectively in 19 CHB patients with dual chamber pacemaker. Ovsyshcher et al[14] demonstrated that optimal AV delay is associated with about 30% more cardiac output during DDD pacing, in comparison to VVI pacing.
The present study also documented a good agreement and correlation between LVOT VTI at optimal AV/PV delay by both echocardiography and QuickOpt algorithm. The hemodynamic outcome in term of LVOT VTI was significantly better with echocardiography, in comparison to QuickOpt algorithm. This is possibly because of IEGM based electrical optimization may not be equal to the best mechanical and hemodynamic performance, as achieved by echocardiography. The time required for AV/PV delay optimization in present study was 45.26 ± 1.73 min by echocardiography and 0.44 ± 0.08 min by QuickOpt (P < 0.0001). To best of our knowledge, there is no available published literature about similar comparison between two methods for AV/PV delay optimization in CHB patients. The average time required for VV delay optimization in CRT patients as reported by Hansalia et al[15] was significantly lower with QuickOpt method in comparison to echocardiography (1.5 ± 0.87 min vs 41 ± 8.3 min, P = 0.006). Thus, QuickOpt is a cheap, fast, simple, automatic and more practical method of AV delay optimization in “real world” practice which can be performed within a minute during regular clinical follow-up using the device programmer.
The present study has few limitations such as use of non-invasive echocardiography method for hemodynamic assessment, which have inherent bias. A single echocardiographic method of transmitral inflow duration was used for AV delay optimization, instead of using other methods such as impedance cardiography[5], peak endocardial acceleration[6], left ventricular invasive pressure measurement (LV dP/dtmax)[16], etc. A study with larger number of patients is required to validate the results, as the present study was of small sample size. The effects of upright position and exercise on optimal AV delay were not assessed. We only measured hemodynamic response and not the clinical benefit in enrolled patients.
In conclusion, the present study demonstrated that an automated programmer-based IEGM method is quick, easy and reliable alternative to time consuming echocardiography method for AV delay optimization in patients of CHB, implanted with dual chamber pacemaker.
Optimization of atrio-ventricular (AV/PV) delay is required for better hemodynamics in patients with complete heart block (CHB).
The present study compared the AV/PV delay optimization by echocardiography and intra-cardiac electrocardiogram based QuickOpt algorithm in CHB patients, subjected to dual chamber pacemaker.
The authors found that QuickOpt algorithm is an automated, easy, quick and reliable alternative to echocardiography for AV/PV delay optimization in CHB patients.
In a real world practice, AV/PV delay optimization can be performed within a minute using QuickOpt algorithm.
IEGM: Intra-cardiac electrogram; CHB: Complete heart block; LVOT VTI: Left ventricular outflow tract velocity time integral; AV/PV: Paced atrio-ventricular/ sensed artio-ventricular; CRT: Cardiac resynchronisation therapy.
The authors stated that optimization of sensed and paced atrio-ventricular (AV/PV) delay is required for better hemodynamics in patients with CHB. They studied the AV/PV delay optimization using echocardiography and intra-cardiac electrocardiogram (IEGM) based QuickOpt algorithm in 20 CHB patients. The results revealed a good agreement between optimal AV and PV delay determined by the two methods. Authors concluded that the automated programmer based IEGM method is a quick, easier and reliable alternative to echocardiography for the optimization of AV/PV delay in CHB patients subjected for dual chamber pacemaker. The tables and figures are presented appropriately.
P- Reviewer: Kusmic C, Lin SL S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Janosik DL, Pearson AC, Buckingham TA, Labovitz AJ, Redd RM. The hemodynamic benefit of differential atrioventricular delay intervals for sensed and paced atrial events during physiologic pacing. J Am Coll Cardiol. 1989;14:499-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Kamdar R, Frain E, Warburton F, Richmond L, Mullan V, Berriman T, Thomas G, Tenkorang J, Dhinoja M, Earley M. A prospective comparison of echocardiography and device algorithms for atrioventricular and interventricular interval optimization in cardiac resynchronization therapy. Europace. 2010;12:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Baker JH, McKenzie J, Beau S, Greer GS, Porterfield J, Fedor M, Greenberg S, Daoud EG, Corbisiero R, Bailey JR. Acute evaluation of programmer-guided AV/PV and VV delay optimization comparing an IEGM method and echocardiogram for cardiac resynchronization therapy in heart failure patients and dual-chamber ICD implants. J Cardiovasc Electrophysiol. 2007;18:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34:2281-2329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1437] [Cited by in RCA: 1472] [Article Influence: 122.7] [Reference Citation Analysis (0)] |
| 5. | Kindermann M, Fröhlig G, Doerr T, Schieffer H. Optimizing the AV delay in DDD pacemaker patients with high degree AV block: mitral valve Doppler versus impedance cardiography. Pacing Clin Electrophysiol. 1997;20:2453-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 139] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Ritter P, Padeletti L, Gillio-Meina L, Gaggini G. Determination of the optimal atrioventricular delay in DDD pacing. Comparison between echo and peak endocardial acceleration measurements. Europace. 1999;1:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 142] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. Statistician. 1983;32:307-317. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2449] [Cited by in RCA: 2459] [Article Influence: 58.5] [Reference Citation Analysis (0)] |
| 8. | Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. The Lancet. 1986;327:307-310. [RCA] [DOI] [Full Text] [Cited by in Crossref: 32742] [Cited by in RCA: 32696] [Article Influence: 838.4] [Reference Citation Analysis (3)] |
| 9. | Hanneman SK. Design, analysis, and interpretation of method-comparison studies. AACN Adv Crit Care. 2008;19:223-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 124] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | Gold MR, Niazi I, Giudici M, Leman RB, Sturdivant JL, Kim MH, Yu Y, Ding J, Waggoner AD. A prospective comparison of AV delay programming methods for hemodynamic optimization during cardiac resynchronization therapy. J Cardiovasc Electrophysiol. 2007;18:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Naito M, Dreifus LS, Mardelli TJ, Chen CC, David D, Michelson EL, Marcy V, Morganroth J. Echocardiographic features of atrioventricular and ventriculoatrial conduction. Am J Cardiol. 1980;46:625-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Ishikawa T, Sumita S, Kimura K, Kikuchi M, Kosuge M, Kuji N, Endo T, Sugano T, Sigemasa T, Kobayashi I. Prediction of optimal atrioventricular delay in patients with implanted DDD pacemakers. Pacing Clin Electrophysiol. 1999;22:1365-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Pearson AC, Janosik DL, Redd RM, Buckingham TA, Labovitz AJ. Hemodynamic benefit of atrioventricular synchrony: prediction from baseline Doppler-echocardiographic variables. J Am Coll Cardiol. 1989;13:1613-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Ovsyshcher I, Zimlichman R, Katz A, Bondy C, Furman S. Measurements of cardiac output by impedance cardiography in pacemaker patients at rest: effects of various atrioventricular delays. J Am Coll Cardiol. 1993;21:761-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Hansalia R, Duvall W, Buckley S, Tilton B, Poole K, Lee LY, Fischer A. A comparison of cardiac resynchronization therapy optimization using QuickOpt and echocardiographic Parameters. HFSA. 2009;S59:190. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Morales MA, Startari U, Panchetti L, Rossi A, Piacenti M. Atrioventricular delay optimization by doppler-derived left ventricular dP/dt improves 6-month outcome of resynchronized patients. Pacing Clin Electrophysiol. 2006;29:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |