Published online Aug 26, 2013. doi: 10.4330/wjc.v5.i8.313
Revised: May 1, 2013
Accepted: July 17, 2013
Published online: August 26, 2013
Processing time: 170 Days and 0.7 Hours
Second generation drug eluting stents (DES) have shown better safety and efficacy in comparison to first generation DES, because of thinner struts, nondurable polymers and coating with better anti-proliferative drugs. The newer DES with cobalt alloy base have demonstrated a greater trackability, deliverability, conformability, flexibility and radio-opacity. However, these thin strut stents have a downside of poor longitudinal axial strength, and therefore get easily deformed/compressed at their end with a slight trauma during exchange of various catheters. We hereby report two cases of “longitudinal stent compression (LSC)” of everolimus-eluting stent, which happened during percutaneous coronary intervention of right coronary artery. Both the cases were successfully managed with non-compliant balloon dilatation. Various reasons for LSC and its management are discussed in the article.
Core tip: The newer second generation drug eluting stent (DES) have shown a greater safety and efficacy compared to first generation DES, because of thinner struts, nondurable polymers and coating with better anti-proliferative drugs. Though their performance is excellent for various type of coronary lesions, one downside is that they are susceptible for compression/ deformation because of poor longitudinal axial strength. We came across longitudinal stent compression (LSC) of everolimus-eluting stent in two cases, which was successfully managed by balloon dilatation. Various reasons for LSC and its management are discussed in the article.
- Citation: Vijayvergiya R, Kumar A, Shrivastava S, Kamana NK. Longitudinal stent compression of everolimus-eluting stent: A report of 2 cases. World J Cardiol 2013; 5(8): 313-316
- URL: https://www.wjgnet.com/1949-8462/full/v5/i8/313.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i8.313
Second generation drug eluting stents (DES) have shown better safety and efficacy in comparison to first generation DES, because of thinner struts, nondurable polymers and coating with better anti-proliferative drugs[1,2]. A change in stent platform from stainless steel to cobalt alloy and a change in stent design have improved the performance of newer DES in terms of trackability, deliverability, conformability, flexibility and radio-opacity. However, these thin-strut stent have a downside of poor longitudinal axial strength, resulting into a newly described observation of “longitudinal stent compression (LSC)”[3]. We hereby report two cases of LSC with everolimus-eluting PROMUS Element stent.
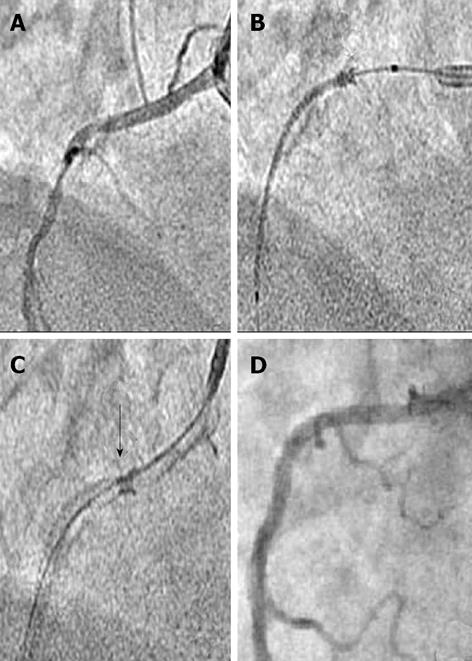
A 62-year-old hypertensive male presented with acute anterior wall myocardial infarction (MI) in July 2012. He underwent primary angioplasty and stenting of mid left anterior descending (LAD) artery. Five days later, he had elective percutaneous coronary angioplasty (PCI) of right coronary artery (RCA). The dominant mid RCA showed a 90% type C, eccentric, calcified lesion (Figure 1A). The RCA was cannulated with JR 3.5, 6F guide catheter, lesion was crossed with 0.014 inch guide wire (Zinger-Support wire; Medtronic, Inc., Minneapolis, Minnesota), and dilated with 2.5 mm × 15 mm semi-compliant balloon (Sprinter balloon, Medtronic). Thereafter, a 3.5 mm × 38 mm PROMUS ElementTM stent (Boston Scientific, Natick, MA, United States) was taken for deployment, but it could not be pushed across the calcified mid RCA lesion. During forceful manipulations to push it, the distal end of stent got stuck-up at mid RCA. Thereafter, an attempt to pull it back into the guide catheter resulted into longitudinal compression of proximal end of the stent (Figure 1B and C). The stent got dislodged from the stent balloon at its proximal position (Figure 1B). At this point, the stent was deployed at same position without any further manipulation. Following stent deployment, the stented segment was post-dilated with 3.5 mm × 15 mm non-compliant (NC) balloon (Sprinter balloon, Medtronic). The residual mid RCA lesion, distal to the deployed stent was dilated with 3.0 mm × 15 mm NC balloon, and a 3.5 mm × 25 mm bare-metal stent (Skylor stent, Medtronic-Invatec, Roncadelle, Italy) was deployed, overlapping the proximal stent. The whole stented segment was post-dilated with 3.5 mm × 15 mm NC balloon at 18 atmospheres. RCA had a thrombolysis in myocardial infarction (TIMI)-3 flow at the end of procedure (Figure 1D). There was no hemodynamic instability during the intervention. He remained asymptomatic during follow-up and a check angiogram at 9-mo showed patent RCA and LAD stents.
A 65-years-old male presented with 15-d old anterior wall MI in July 2012. He was in gross congestive heart failure, which improved with diuretic therapy. Echocardiography revealed akinetic anterior wall, no mitral regurgitation and ejection fraction of 0.30. Coronary angiogram revealed 100% occluded proximal LAD with thrombus, and a 90% eccentric, calcified, type C lesion at proximal RCA (Figure 2A). He was subjected for PCI to LAD. The left coronary artery was cannulated with JL 3.5, 6 F guide catheter and proximal LAD lesion was crossed with 0.014 inch guide wire (Zinger-Support wire, Medtronic). The lesion was dilated with 2.5 mm × 15 mm balloon and thrombus aspiration with 6F Export aspiration catheter (Medtronic) was performed. There was TIMI-0 flow despite repeated thrombus aspiration and intra-coronary bolus of abciximab. He was put on abciximab infusion and shifted back to coronary care unit. Later, a check angiogram showed occluded proximal LAD. This time no further intervention was performed to LAD considering it as a non-viable territory; and was taken up for PCI to RCA. The RCA was cannulated with JR 3.5, 6 F guide catheter and proximal RCA lesion was crossed with 0.014 inch guide wire (Zinger-Support wire, Medtronic). The lesion was dilated with 2.5 mm × 15 mm semi-compliant balloon (Sprinter, Medtronic). Thereafter, a 2.75 mm × 38 mm PROMUS ElementTM stent (Boston Scientific) was taken for deployment, but it could not be pushed across calcified proximal RCA lesion. During forceful manipulations to push it, the distal end of stent got stuck-up at proximal lesion site. Thereafter, an attempt to pull it back into the guide catheter resulted into longitudinal compression of proximal end of the stent (Figure 2B and C). The stent got dislodged from the stent balloon at its proximal position (Figure 2C). The stent was deployed at same position without any further manipulation. Post stent deployment, the stented segment was post-dilated with 2.75 mm × 15 mm NC balloon (Sprinter, Medtronic). The residual RCA lesion, distal to the deployed stent was dilated with 2.75 mm × 15 mm NC balloon and a 2.75 mm × 16 mm PROMUS ElementTM stent (Boston Scientific) was deployed, overlapping the proximal stent. The whole stented segment was post-dilated with 2.75 mm × 15 mm NC balloon at 18 atmospheres. He remained hemodynamically stable during PCI and had a TIMI-3 flow in RCA (Figure 2D). Twenty-four hours later, he had an episode of massive hematemesis followed by hypotension, which was appropriately managed. There was no chest pain and no ST-segment elevation in inferior electrocardiogram leads, which rule out a possibility of acute stent-thrombosis. Later in the course, he had recurrent ventricular tachycardia followed by asystole, from which he could not be revived and expired.
Longitudinal stent compression has been described by various authors in newer generation cobalt alloy stents. It is commonly reported with PROMUS Element stent, though isolated report of other stents such as Taxus Liberte (Boston Scientific Co., Natick, MA, United States), Biomatrix (Biosensors Interventional Technologies, Singapore), Endeavor (Medtronic Inc., Minneapolis, Minnesota) and Xience (Abbott Vascular, Santa Clara, CA, United States) is also available[4,5]. Our incidence of 0.8% LSC (2 out of 250 deployed PROMUS Element stents in 6 mo, from July 2012-December 2012) is similar to the reported incidence of 0.6%-0.8% by other authors[4-6]. A bench testing for longitudinal strength of various DES as studied by Ormiston et al[7] and Prabhu et al[8], have demonstrated that a 2-link offset peak-to-peak stent design of PROMUS Element has the lowest resistance for longitudinal compression. A relatively better radio-opacity of PROMUS Element is another reason for frequent recognition of LSC during fluoroscopy[9]. The incidence can be much higher with various stents, if a routine intra-vascular ultrasound (IVUS) or optical coherence tomography (OCT) is performed[3,10]. Various reasons for LSC can be guide catheter induced deformation of a stent at osteal or proximal lesions and a compression by un-inflated balloon or IVUS catheter[3,4]. In both of our cases, the stent got stuck up in calcified RCA lesion, and during attempted withdrawal of stent in guide catheter, it got longitudinally compressed at proximal end by catheter tip. A guide catheter induced compression was the reason for stent deformation in all the three reported cases by Hanratty et al[3]. We personally feel that a better plaque modification in a calcified/hard lesion is mandatory prior to stent deployment to avoid such complication. Proper handling and a resistance free passage of various catheters across the stented segment can prevent LSC. The treatment of LSC includes dilatation of deformed segment with adequate size non-compliant balloon and if required another stent for favorable end results[4]. In both the cases, we had favorable outcome after non-compliant balloon dilatation and without putting an additional stent at deformed site. Though, fluoroscopy has a limited value in comparison to IVUS or OCT for diagnosis of mal-apposition of deformed stent segment, we did not perform it in both the cases. Willims et al[4] have reported a case of stent thrombosis following LSC at mid LAD. The reasons for death of 2nd index case were multi-factorial including upper gastro-intestinal bleed, hypotension secondary to blood loss, ischemic heart failure, and recurrent ventricular tachycardia; however a possible acute stent thrombosis of RCA could not be ruled out.
In conclusion, LSC is a rare phenomenon, which is observed with most of newer thin-strut DES. PROMUS Element having a 2-link offset peak-to-peak stent design is more prone to longitudinal compression in comparison to other stents. A meticulous PCI technique with proper handling of various catheters across the ostio-proximal lesions and stented segment is important to avoid such complication. A timely recognition with available imaging modality such as fluoroscopy, IVUS or OCT and an appropriate treatment is essential to avoid unfavorable clinical outcome.
P- Reviewers Cheng XS, Prashanth P, Teng RJ S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Kedhi E, Gomes ME, Lagerqvist B, Smith JG, Omerovic E, James S, Harnek J, Olivecrona GK. Clinical impact of second-generation everolimus-eluting stent compared with first-generation drug-eluting stents in diabetes mellitus patients: insights from a nationwide coronary intervention register. JACC Cardiovasc Interv. 2012;5:1141-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Planer D, Smits PC, Kereiakes DJ, Kedhi E, Fahy M, Xu K, Serruys PW, Stone GW. Comparison of everolimus- and paclitaxel-eluting stents in patients with acute and stable coronary syndromes: pooled results from the SPIRIT (A Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System) and COMPARE (A Trial of Everolimus-Eluting Stents and Paclitaxel-Eluting Stents for Coronary Revascularization in Daily Practice) Trials. JACC Cardiovasc Interv. 2011;4:1104-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Hanratty CG, Walsh SJ. Longitudinal compression: a “new” complication with modern coronary stent platforms--time to think beyond deliverability? EuroIntervention. 2011;7:872-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Williams PD, Mamas MA, Morgan KP, El-Omar M, Clarke B, Bainbridge A, Fath-Ordoubadi F, Fraser DG. Longitudinal stent deformation: a retrospective analysis of frequency and mechanisms. EuroIntervention. 2012;8:267-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Shannon J, Latib A, Takagi K, Chieffo A, Figini F, Sacco F, Ferrarello S, Montorfano M, Colombo A. “Procedural trauma risks longitudinal shortening of the Promus Element™ stent platform”. Catheter Cardiovasc Interv. 2013;81:810-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Leibundgut G, Gick M, Toma A, Valina C, Löffelhardt N, Büttner HJ, Neumann FJ. Longitudinal compression of the platinum-chromium everolimus-eluting stent during coronary implantation: predisposing mechanical properties, incidence, and predictors in a large patient cohort. Catheter Cardiovasc Interv. 2013;81:E206-E214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Ormiston JA, Webber B, Webster MW. Stent longitudinal integrity bench insights into a clinical problem. JACC Cardiovasc Interv. 2011;4:1310-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 8. | Prabhu S, Schikorr T, Mahmoud T, Jacobs J, Potgieter A, Simonton C. Engineering assessment of the longitudinal compression behaviour of contemporary coronary stents. EuroIntervention. 2012;8:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Finet G, Rioufol G. Coronary stent longitudinal deformation by compression: is this a new global stent failure, a specific failure of a particular stent design or simply an angiographic detection of an exceptional PCI complication? EuroIntervention. 2012;8:177-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Bartorelli AL, Andreini D, Pontone G, Trabattoni D, Ferrari C, Mushtaq S, Ormiston JA. Stent longitudinal distortion: strut separation (pseudo-fracture) and strut compression (“concertina” effect). EuroIntervention. 2012;8:290-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |