Revised: October 29, 2011
Accepted: November 5, 2011
Published online: January 26, 2012
AIM: To investigate the prognostic significance of resting heart rate in patients with acute coronary syndrome (ACS), independent of other known factors.
METHODS: Patients 40 years of age or older who had been admitted with acute coronary syndrome (ACS) to one of the 94 hospitals participating in the Prevalence of Peripheral Arterial Disease in Patients with Acute Coronary Syndrome (PAMISCA) study were included. Patients were divided into two groups based on their resting heart rate (HR ≥ or < 70 bpm). Complications were recording during a follow-up period of 1 year.
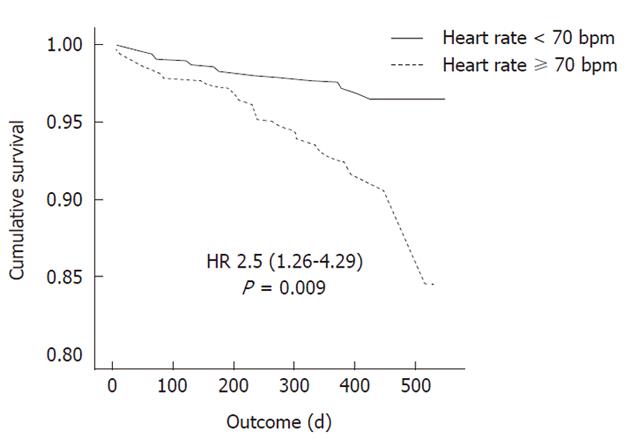
RESULTS: There were 1054 ACS patients analyzed (43.5% with ST segment elevation and 56.5% without elevation). Mean age was 66.6 ± 11.7 years, 70.6% were male and 29.4% of subjects were female. During follow-up, more patients in the HR ≥ 70 bpm group were hospitalized for heart failure and they also had a higher mortality rate. In the multivariate analysis, a heart rate of ≥ 70 bpm was independently related to overall mortality during the follow-up period (hazard ratio 2.5; 95% confidence interval, 1.26-4.97, P = 0.009).
CONCLUSION: A resting heart rate ≥ 70 bpm in patients who survive an ACS is an indicator of a high risk of suffering cardiovascular events during follow-up.
- Citation: Fácila L, Morillas P, Quiles J, Soria F, Cordero A, Mazón P, Anguita M, Martín-Luengo C, Gonzalez-Juanatey JR, Bertomeu V, Investigators OBOT&POPADIPWACS(. Prognostic significance of heart rate in hospitalized patients presenting with myocardial infarction. World J Cardiol 2012; 4(1): 15-19
- URL: https://www.wjgnet.com/1949-8462/full/v4/i1/15.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i1.15
Heart rate (HR) is increasingly being postulated as a modifiable risk factor for cardiovascular disease. Previous studies have shown a relationship between elevated resting HR and the risk of cardiovascular disease in the general population[1] and in patients with stable coronary artery disease with or without hypertension[2-6]. However, the threshold at which risk increases in coronary patients and the quantitative relationship between HR increase and outcome are less well defined. Data from the Coronary Artery Surgery Study suggested that risk increases at around 83 beats per minute (bpm) and above[2], whereas analysis by the International Verapamil SR/Trandolapril Study suggested increased risk above 75 bpm, well below the conventional definition of tachycardia (> 90 bpm)[7]. The results of the BEAUTIFUL study (Evaluation of the if inhibitor ivabradine in patients with coronary disease and left ventricular dysfunction) have recently demonstrated that, in a large population with coronary artery disease and left-ventricular systolic dysfunction who were well treated in terms of cardiovascular prevention, a resting HR at baseline of ≥ 70 bpm is a marker for subsequent cardiovascular death and morbidity[8]. Results were recently published in patients with heart failure and ventricular dysfunction in whom treatment with ivabradine to decrease HR was effective and reduced cardiovascular risk[9].
There are few observational studies[10] which have analyzed the prognostic impact of resting HR in patients with acute coronary syndrome (ACS), independent of the presence of factors associated with advanced arteriosclerotic heart disease (peripheral artery disease and kidney disease). The objective of this study is to analyze the prognostic impact of resting HR in patients who have survived the acute phase of a coronary syndrome, establishing the cut-off point at 70 bpm as in the BEAUTIFUL study.
The PAMISCA registry (Prevalence of Peripheral Arterial Disease in Patients with Acute Coronary Syndrome), is an observational, prospective, multicenter study, designed to investigate the prevalence of peripheral arterial disease in patients admitted to Spanish hospitals with a diagnosis of ACS. A detailed description of the method used in the PAMISCA registry has been published previously[11]. Informed consent was obtained from all patients and the study was carried out following the principles of the Declaration of Helsinki (Edinburgh Amendment, 2000). The study was approved by an ethics committee. Data on risk factors, cardiovascular history and medical treatment of ACS patients were collected at discharge using a standard questionnaire. Cardiovascular risk factors included hypertension, diabetes mellitus, hypercholesterolemia, smoking habit, previous ischemic events (ACS, stable angina, stroke) and previous heart failure (hospital admission). Left ventricular ejection fraction was obtained by trans-thoracic echocardiography or ventriculography during catheterization. Glomerular filtration rate, assessed by the Modification of Diet in Renal Disease Study equation, was also recorded. HR was determined between day 3 and 7 of the event, once the patient was stable. The study population was divided into subgroups, depending on whether a patient’s HR was ≥ or < 70 bpm, with the differential characteristics of each subgroup being studied. This cut-off point was selected in accordance with the most recent bibliography[8].
Patients were followed up to 12 mo after hospital discharge to ascertain the occurrence of clinical events. Clinical complications were defined by the registry investigators’ committee and included in the data questionnaire. The primary endpoint was mortality (cardiovascular and non cardiovascular death). Secondary endpoints were hospital admission for myocardial infarction (elevation of serum markers of myocardial damage), heart failure, angina, coronary revascularization and stroke. Angina was defined as the presence of chest pain or discomfort with dynamic changes in the electrocardiogram. Heart failure was defined as the new onset of signs and symptoms of abnormal cardiac function and one imaging diagnosis (X-ray verification of pulmonary congestion or echocardiography diagnosis of left ventricular systolic or diastolic dysfunction). All cardiovascular endpoints were confirmed by hospital reports. Every case of death reported by the medical staff was certified by the investigator of each hospital (death certificates or hospital records at the time of death, or direct contact with the family of patients). Follow-up was performed by medical visits or telephone calls.
All data collected in the study was described in terms of central trend, dispersion measurements and relative frequencies. The Student t test was used for comparison of quantitative variables, the Chi-squared test for comparison of the categorical variables and one-way analysis of variance for comparison of the continuous variables between multiple groups. We used a Cox multivariate regression analysis with adjustment based on the likelihood ratio. The variables entered into the model were those with a P value < 0.1 in the univariate analysis: age, sex, hypertension, diabetes, previous myocardial infarction, previous stroke, ejection fraction < 40%, end-stage renal disease, revascularization at admission (thrombolysis or percutaneous coronary intervention), treatment at discharge with aspirin, clopidogrel, statins, β-blockers or angiotensin receptor blockers, existence of peripheral vascular disease, and HR ≥ 70 bpm. Calibration of the multivariate model was tested by Hosmer-Lemeshow statistic and the discriminative power by the area under the ROC (receiver-operating characteristics) curve obtained by the analysis of the probability of the prognostic value of the multivariate model. The Kaplan-Meier survival method was used for the comparison of survival according to the HR (≥ or < 70 bpm) using the log-rank test. A value of P≤ 0.05 was considered statistically significant. Data were analyzed using SPSS 15.0 software (SPSS Inc., Chicago, IL).
A total of 1410 patients were included in the baseline study and 13 died before hospital discharge. Investigators were then invited to provide follow-up for the 1397 remaining patients for 1 year. A total of 23 investigators participated in the study, while 241 patients declined the invitation. Therefore, the prospective phase of the study included 1156 patients; 1054 (91.2%) of these completed follow-up. The analysis was carried out in 1054 patients with ACS, of which 43.5% had ST segment elevation and 56.5% had no ST segment elevation. The mean age of included patients was 66.6 ± 11.7 years, 744 (70.6%) were male and 310 (29.4%) were female. Table 1 presents the characteristics of the study population.
| HR< 70 (n = 480) | HR≥70 (n = 561) | P | |
| Mean age | 65.8 ± 11.9 | 67.3 ± 11.4 | 0.035 |
| Women | 128.0 (41.7) | 179.0 (58.3) | 0.037 |
| Abdominal circumference (cm) | 99.5 (11.9) | 100.3 (13.0) | NS |
| Body mass index | 28.1 (3.9) | 28.1 (4.0) | NS |
| Hypertension | 372.0 (77.5) | 470.0 (83.8) | 0.011 |
| Diabetes mellitus | 136.0 (28.3) | 236.0 (42.1) | < 0.001 |
| Dislipidemia | 416.0 (86.7) | 471.0 (84.0) | NS |
| Smokers | 144.0 (30.3) | 154.0 (27.5) | NS |
| History of heart disease | 208.0 (43.3) | 234.0 (41.7) | NS |
| History of CVA | 37.0 (7.7) | 57.0 (10.2) | NS |
| Peripheral Artery Disease | 62.0 (12.9) | 108.0 (19.3) | 0.004 |
| Previous heart failure | 22.0 (4.6) | 61.0 (10.9) | < 0.001 |
| EF < 40% | 32.0 (7.5) | 83.0 (17.0) | < 0.001 |
| Mean SBP (mmHg) | 124.3 (18.5) | 129.6 (22.4) | < 0.001 |
| Mean DBP (mmHg) | 71.8 (11.2) | 74.2 (13.4) | NS |
| Mean HR (bpm) | 60.3 (5.9) | 80.6 (12.6) | < 0.001 |
| Glucose (mg/dL) | 116.7 (46.5) | 131.4 (55.0) | < 0.001 |
| Hemoglobin (g/L) | 13.6 (1.6) | 13.2 (1.9) | 0.002 |
| Total cholesterol (mg/dL) | 180.6 (40.3) | 180.9 (42.8) | 0.015 |
| LDL cholesterol (mg/dL) | 109.9 (34.1) | 109.5 (34.6) | NS |
| Creatinine (mg/dL) | 1.03 ± 0.31 | 1.13 ± 0.82 | NS |
| GFR (mL/min every 1.73 m2) | 77.70 ± 23.80 | 75.30 ± 26.10 | NS |
| ASA | 409.0 (87.6) | 446.0 (86.1) | NS |
| Diuretics | 81.0 (16.9) | 137.0 (62.8) | 0.003 |
| β-blockers | 387.0 (80.6) | 379.0 (67.6) | < 0.001 |
| Calcium antagonists | 72.0 (15.0) | 119.0 (21.2) | 0.010 |
| ACE inhibitors | 255.0 (53.1) | 304.0 (54.2) | NS |
| Angiotensin II receptor blockers | 51.0 (10.6) | 80.0 (14.3) | NS |
| Statins | 413.0 (86.0) | 453.0 (80.7) | 0.025 |
| Coronary revascularization (PCI/thrombolysis) | 294.0 (61.2) | 287.0 (53.9) | 0.001 |
Fifty-three percent (53%) of patients had a resting HR ≥ 70 bpm. These patients were elderly with a higher percentage of women, hypertension, diabetes, history of heart failure and diagnosed with peripheral artery disease (Table 1). During admission, these patients had higher blood sugar and cholesterol levels, while their hemoglobin levels were lower. Mean systolic blood pressure was higher in patients with HR ≥ 70 bpm, as was the percentage of patients with left ventricular ejection fraction < 40% at admission. Patients with HR ≥ 70 bpm received more diuretics and calcium antagonists, while the use of β-blockers, statins and coronary revascularization was lower (Table 1).
During the follow-up period of approximately 1 year (median 382 d, interquartile range 66), patients with HR ≥ 70 bpm had a poorer outcome (Figure 1), with more hospitalizations for heart failure and higher cardiovascular and non-cardiovascular mortality rates. No differences were observed with respect to ischemic complications (re-infarction or need for revascularization) (Table 2).
| HR < 70 (n = 480) | HR≥70 (n = 561) | P | |
| Total deaths | 13 (2.7) | 45 (8.0) | < 0.001 |
| Cardiovascular death | 11 (2.3) | 35 (6.2) | 0.001 |
| Non-cardiovascular death | 2 (0.5) | 10 (1.8) | 0.035 |
| Hospitalized for heart failure | 22 (4.6) | 63 (11.2) | < 0.001 |
| Revascularization (PCI or surgical) | 48 (10.0) | 53 (9.4) | NS |
| Hospitalized for AMI | 22 (4.6) | 31 (5.5) | NS |
In the multivariate analysis, HR ≥ 70 bpm was independently correlated with mortality during follow-up (hazard ratio 2.5; 95% confidence interval (CI), 1.26-4.97, P = 0.009), along with peripheral artery disease during hospitalization, ejection fraction < 40%, age and type 2 diabetes mellitus. In-hospital revascularization (in the form of thrombolysis or angioplasty) acted as a protective factor (Table 3). The multivariate analysis was accurately calibrated (P = NS; χ2 = 18.5) and had discriminative power (area under the curve 0.81; 95% CI, 0.74-0.90, P < 0.01).
| Variable | Hazard ratio | 95% CI | P |
| Heart rate ≥ 70 bpm | 2.50 | 1.26-4.97 | 0.009 |
| Peripheral artery disease | 1.51 | 1.14-2.01 | 0.004 |
| Revascularization at admission | 0.53 | 0.29-0.97 | 0.040 |
| EF < 40% | 1.87 | 0.98-3.58 | 0.057 |
| Age (per year) | 1.08 | 1.03-1.12 | < 0.001 |
| Type 2 diabetes mellitus | 1.80 | 1.01-3.22 | 0.047 |
Our study revealed the prognostic significance of resting HR in patients who survived ACS. We found that HR ≥ 70 bpm identified a population that is at high risk of suffering cardiovascular events (death or heart failure) during follow-up.
These results confirm those from studies which demonstrated that baseline HR is directly and independently related to ischemic events, sudden death, cardiovascular death and mortality from any cause, both in patients with known ischemic events and in the normal population or in patients with increased cardiovascular risk[2,7,8]. It is probable that HR is not only a prognostic marker, but also has a detrimental cardiovascular effect due to several mechanisms: (1) an atherogenic effect (an increase in shear stress in the artery which causes increased parietal stress and decreased distensibility); (2) increased sympathetic tone (which would induce a procoagulant state); (3) increased blood pressure (regardless of other factors); and (4) an increase in the metabolic needs of the heart. The above abnormalities could explain the cardiovascular complications in these patients[12-15].
The relationship between HR (its increase) and cardiovascular mortality has long been known, but its importance as a risk factor was only established in an article published in 1980 by Dyer et al[10]. Subsequently, several studies have observed how, in individuals with no previous evidence of cardiovascular disease, there is a very significant relationship between baseline HR, an increase in blood pressure and the adjusted rate of all fatal and non-fatal coronary events. Risk increased starting at a value of 60 bpm; risk was five times greater if baseline HR was > 90 bpm, regardless of age, sex and weight.
In a sample of 24913 patients with suspected or proven coronary artery disease monitored for an average of 14.7 years, Diaz et al[2] recently highlighted that total mortality, cardiovascular mortality and re-hospitalization due to cardiovascular causes were associated with an increase in HR (P < 0.0001). Patients with HR ≥ 83 bpm in the baseline study had total mortality 32% higher than the reference group after adjusting for multiple variables. In our study conducted in patients with acute myocardial infarction who survived after admission, HR ≥ 70 bpm during hospitalization (once stabilized) was associated with a higher overall mortality, irrespective of important variables such as age, treatment upon discharge or ejection fraction in long-term follow-up. These findings concur with recent data from the BEAUTIFUL study which demonstrated that patients with a history of ischemic heart disease and depressed systolic function who had a resting HR ≥ 70 bpm were at higher risk of cardiovascular complications and death[8]. However, they did not concur with regard to adverse events, which were not significant in our study. The absence of long-term follow-up in our study could explain these differences.
These epidemiological data are supported by the findings of various clinical trials which have demonstrated that a decrease in HR using drugs, such as β-blockers or ivabradin improves prognosis in patients with acute myocardial infarction[16], heart failure[9,17-20], and angina[21-25], and is an essential part of the beneficial effect of these drugs in prognosis. In this respect, an important finding in our study is the decreased use of β-blockers, statins and coronary revascularization in patients with a higher HR, even though they were at higher risk. The reason behind this therapeutic nihilism could be due to a lack of awareness that increased HR can be related to poorer prognosis and therefore greater risk, in which case therapeutic strategies should be more aggressive.
The limitations of our study are those inherent to any observational registry, from which only an association between variables can be established (and not a cause-effect relationship), the limitations of obtaining medical history data, and of the comorbidities that could explain the changes in HR.
In conclusion, our study reflects that a resting HR ≥ 70 bpm after an ACS identifies a population that is at high risk of suffering cardiovascular events, with a higher mortality during follow-up. It is possible that more aggressive treatment of these patients, especially with the use of HR-lowering drugs, could translate into an improvement in their prognosis.
To Laboratorios Sanofi-Aventis for its contribution, assistance and unwavering dedication in this project. To all participating investigators, whose daily work and efforts made the conduct of this study possible.
Heart rate (HR) is increasingly being postulated as a modifiable risk factor for cardiovascular disease. Previous studies have shown a relationship between elevated resting HR and the risk of cardiovascular disease in the general population. There are few observational studies which have analyzed the prognostic impact of resting HR in patients with acute coronary syndrome, independent of factors which suggest advanced arteriosclerotic heart disease (peripheral artery disease and kidney disease).
HR is of great interest if confirmed as a cardiovascular risk factor, as measures can be taken to reduce it. Thus we are developing a series of drugs for its reduction (such as ivabradine), and for the possible prevention of cardiovascular events.
It is possible that more aggressive treatment of these patients, especially with the use of HR-lowering drugs, could translate into an improvement in their prognosis.
The study results suggest that the HR is a predictor of cardiovascular events, and treatment to reduce HR is beneficial for patients with ischemic heart disease.
HR is the number of heartbeats per unit of time, typically expressed as beats per minute (bpm). HR can vary as the body’s need to absorb oxygen and excrete carbon dioxide changes, such as during exercise or sleep. Ivabradine is a novel medication used for the symptomatic management of stable angina pectoris. Ivabradine acts on the If (f is for “funny”, so called because it had unusual properties compared with other current systems known at the time of its discovery) ion current, which is highly expressed in the sinoatrial node. If is a mixed Na+-K+ inward current activated by hyperpolarization and modulated by the autonomic nervous system. It is one of the most important ionic currents for regulating pacemaker activity in the sinoatrial (SA) node. Ivabradine selectively inhibits the pacemaker If current in a dose-dependent manner. Blocking this channel reduces cardiac pacemaker activity, slowing the HR and allowing more time for blood to flow to the myocardium.
This is a good descriptive study in which authors analyze the the prognostic impact of HR in patients with non-ST elevation acute coronary syndrome (ACS). The authors reflects that a resting HR ≥ 70 bpm after an non-ST ACS identifies a population that is at high risk of suffering cardiovascular events, with a higher mortality during follow-up. It is possible that more aggressive treatment of these patients, especially with the use of HR-lowering drugs, could translate into an improvement in their prognosis.
Peer reviewer: Robert Lee Page II, PhD, MSPH, FASHP, FASCP, FCCP, FAHA, BCPS, CGP, Associate Professor of Clinical Pharmacy and Physical Medicine, Clinical Specialist, Division of Cardiology, University of Colorado, School of Pharmacy and Medicine, C238-L15, Academic Office 1, 12631 East 17th Ave, Room L15-1415, PO Box 6511, Aurora, CO 80045, United States
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
| 1. | Kannel WB, Kannel C, Paffenbarger RS, Cupples LA. Heart rate and cardiovascular mortality: the Framingham Study. Am Heart J. 1987;113:1489-1494. [PubMed] [Cited in This Article: ] |
| 2. | Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J. 2005;26:967-974. [PubMed] [Cited in This Article: ] |
| 3. | Palatini P, Thijs L, Staessen JA, Fagard RH, Bulpitt CJ, Clement DL, de Leeuw PW, Jaaskivi M, Leonetti G, Nachev C. Predictive value of clinic and ambulatory heart rate for mortality in elderly subjects with systolic hypertension. Arch Intern Med. 2002;162:2313-2321. [PubMed] [Cited in This Article: ] |
| 4. | Kovar D, Cannon CP, Bentley JH, Charlesworth A, Rogers WJ. Does initial and delayed heart rate predict mortality in patients with acute coronary syndromes? Clin Cardiol. 2004;27:80-86. [PubMed] [Cited in This Article: ] |
| 5. | Palatini P, Benetos A, Julius S. Impact of increased heart rate on clinical outcomes in hypertension: implications for antihypertensive drug therapy. Drugs. 2006;66:133-144. [PubMed] [Cited in This Article: ] |
| 6. | Palatini P, Julius S. Elevated heart rate: a major risk factor for cardiovascular disease. Clin Exp Hypertens. 2004;26:637-644. [PubMed] [Cited in This Article: ] |
| 7. | Kolloch R, Legler UF, Champion A, Cooper-Dehoff RM, Handberg E, Zhou Q, Pepine CJ. Impact of resting heart rate on outcomes in hypertensive patients with coronary artery disease: findings from the INternational VErapamil-SR/trandolapril STudy (INVEST). Eur Heart J. 2008;29:1327-1334. [PubMed] [Cited in This Article: ] |
| 8. | Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R. Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet. 2008;372:817-821. [PubMed] [Cited in This Article: ] |
| 9. | Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875-885. [PubMed] [Cited in This Article: ] |
| 10. | Dyer AR, Persky V, Stamler J, Paul O, Shekelle RB, Berkson DM, Lepper M, Schoenberger JA, Lindberg HA. Heart rate as a prognostic factor for coronary heart disease and mortality: findings in three Chicago epidemiologic studies. Am J Epidemiol. 1980;112:736-749. [PubMed] [Cited in This Article: ] |
| 11. | Bertomeu V, Morillas P, Gonzalez-Juanatey JR, Quiles J, Guindo J, Soria F, Llacer A, Lekuona I, Mazón P, Martín-Luengo C. Prevalence and prognostic influence of peripheral arterial disease in patients & gt; or=40 years old admitted into hospital following an acute coronary event. Eur J Vasc Endovasc Surg. 2008;36:189-196. [PubMed] [Cited in This Article: ] |
| 12. | Julius S, Pascual AV, London R. Role of parasympathetic inhibition in the hyperkinetic type of borderline hypertension. Circulation. 1971;44:413-418. [PubMed] [Cited in This Article: ] |
| 13. | Bassiouny HS, Zarins CK, Kadowaki MH, Glagov S. Hemodynamic stress and experimental aortoiliac atherosclerosis. J Vasc Surg. 1994;19:426-434. [PubMed] [Cited in This Article: ] |
| 14. | Palatini P, Casiglia E, Julius S, Pessina AC. High heart rate: a risk factor for cardiovascular death in elderly men. Arch Intern Med. 1999;159:585-592. [PubMed] [Cited in This Article: ] |
| 15. | Heidland UE, Strauer BE. Left ventricular muscle mass and elevated heart rate are associated with coronary plaque disruption. Circulation. 2001;104:1477-1482. [PubMed] [Cited in This Article: ] |
| 16. | Kjekshus JK. Importance of heart rate in determining beta-blocker efficacy in acute and long-term acute myocardial infarction intervention trials. Am J Cardiol. 1986;57:43F-49F. [PubMed] [Cited in This Article: ] |
| 17. | Kjekshus JK, Gullestad L. Heart rate as a therapeutic target in heart failure. Eur Heart J. 1999;1:H65-H69. [Cited in This Article: ] |
| 18. | Mulder P, Barbier S, Chagraoui A, Richard V, Henry JP, Lallemand F, Renet S, Lerebours G, Mahlberg-Gaudin F, Thuillez C. Long-term heart rate reduction induced by the selective I(f) current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failure. Circulation. 2004;109:1674-1679. [PubMed] [Cited in This Article: ] |
| 19. | Fang Y, Debunne M, Vercauteren M, Brakenhielm E, Richard V, Lallemand F, Henry JP, Mulder P, Thuillez C. Heart Rate Reduction Induced by the If Current Inhibitor Ivabradine Improves Diastolic Function and Attenuates Cardiac Tissue Hypoxia. J Cardiovasc Pharmacol. 2011;Epub ahead of print. [PubMed] [Cited in This Article: ] |
| 20. | Thackray SD, Ghosh JM, Wright GA, Witte KK, Nikitin NP, Kaye GC, Clark AL, Tweddel A, Cleland JG. The effect of altering heart rate on ventricular function in patients with heart failure treated with beta-blockers. Am Heart J. 2006;152:713.e9-713.13. [PubMed] [Cited in This Article: ] |
| 21. | Gayet JL, Paganelli F, Cohen-Solal A. Update on the medical treatment of stable angina. Arch Cardiovasc Dis. 2011;104:536-544. [PubMed] [Cited in This Article: ] |
| 22. | Kones R. Recent advances in the management of chronic stable angina II. Anti-ischemic therapy, options for refractory angina, risk factor reduction, and revascularization. Vasc Health Risk Manag. 2010;6:749-774. [PubMed] [Cited in This Article: ] |
| 23. | Tardif JC, Ford I, Tendera M, Bourassa MG, Fox K. Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable angina. Eur Heart J. 2005;26:2529-2536. [PubMed] [Cited in This Article: ] |
| 24. | Cucherat M, Borer JS. Reduction of Resting Heart Rate With Antianginal Drugs: Review and Meta-Analysis. Am J Ther. 2011;Epub ahead of print. [PubMed] [Cited in This Article: ] |
| 25. | Dominguez-Rodriguez A, Blanco-Palacios G, Abreu-Gonzalez P. Increased heart rate and atherosclerosis: potential implications of ivabradine therapy. World J Cardiol. 2011;3:101-104. [PubMed] [Cited in This Article: ] |