Published online Dec 15, 2021. doi: 10.4239/wjd.v12.i12.2107
Peer-review started: May 12, 2021
First decision: July 4, 2021
Revised: July 13, 2021
Accepted: November 24, 2021
Article in press: November 24, 2021
Published online: December 15, 2021
Vaccination against influenza and pneumococcus is effective in reducing morbidity and mortality in patients with diabetes.
To investigate the prevalence of influenza and pneumococcal vaccinations and to search for the independent associates of vaccination in Turkish patients with diabetes.
In this cross-sectional, nationwide, multicenter study, adult patients with type 1 diabetes (T1DM) (n = 454) and type 2 diabetes (T2DM) (n = 4721), who were under follow-up for at least a year in the outpatient clinics, were consecutively enrolled. Sociodemographic, clinical, and laboratory parameters of patients were recorded. Vaccination histories were documented according to the self-statements of the patients.
Patients with T1DM and T2DM had similar vaccination rates for influenza (23.6% vs 21.2%; P = 0.240) and pneumococcus (8% vs 7%; P = 0.451) vaccinations. Longer diabetes duration and older age were the common independent associates of having vaccination for both types of diabetes patients. Higher education level, using statin treatment, and having optimal hemoglobin A1c levels were the common independent associates of influenza and pneumococcal vaccination in patients with T2DM.
TEMD Vaccination Study shows that patients with T1DM and T2DM had very low influenza and pneumococcal vaccination rates in Turkey. The lower rates of vaccination in certain populations urges the necessity of nationwide vaccination strategies targeting these populations.
Core Tip: The TEMD Vaccination Study is a cross-sectional, multicenter survey, which was carried out between April 1 and June 30, 2017, in 68 tertiary endocrine units from 37 cities throughout Turkey. The study revealed that the vaccination rates for pneumococcus and influenza were very low in patients with diabetes. Only 6.6% patients with type 1 diabetes (T1DM) and 5.8% patients with type 2 diabetes (T2DM) received both vaccines. Older age and longer diabetes duration were the common independent associates of vaccination in patients with T1DM and T2DM. The common independent associates of vaccination rates for T2DM were using statins, higher education and the lower hemoglobin A1c levels.
- Citation: Demirci I, Haymana C, Salman S, Tasci I, Corapcioglu D, Kirik A, Yetkin İ, Altay M, Sabuncu T, Bayram F, Satman I, Sonmez A, TEMD Study Group. Rates and associates of influenza and pneumococcus vaccination in diabetes mellitus: A nationwide cross-sectional study (TEMD vaccination study). World J Diabetes 2021; 12(12): 2107-2118
- URL: https://www.wjgnet.com/1948-9358/full/v12/i12/2107.htm
- DOI: https://dx.doi.org/10.4239/wjd.v12.i12.2107
Patients with diabetes are prone to influenza and pneumococcal infections with a more severe clinical course[1-3]. Deaths due to influenza and pneumococcal infections are two to three times higher in patients with diabetes compared to non-diabetic patients[4]. Moreover, the need for hospitalization due to influenza and pneumococcal infections is also higher in patients with diabetes[2]. Various observational studies reported that vaccination against influenza and pneumococcus is effective in reducing morbidity and mortality in patients with diabetes[5,6]. Therefore, many national and international guidelines recommend annual influenza vaccination, and one or two doses of pneumococcal vaccination depending on age under or over 65 years, for both type 1 (T1DM) or type 2 diabetes mellitus (T2DM)[7-9].
Despite all these recommendations, the vaccination rates in patients with diabetes are unsatisfactory around the world[10-12]. To establish better immunization policies, there is a need to find out the regional or national barriers to vaccination. So far, various factors such as low availability of the vaccine, healthcare costs, physician and patient attitudes, racial disparities, social influences, and misbeliefs were mentioned in various reports as the causes of low vaccination rates[13,14]. However, there is hardly enough data about the rates and predictors of influenza and pneumococcal vaccination in Turkish patients with diabetes[15,16].
The recently published national survey “Turkish Nationwide SurvEy of Glycemic and Other Metabolic Parameters of Patients with Diabetes Mellitus (TEMD Study)” reported the clinical and demographical factors predicting the glycemic and metabolic targets in Turkish patients with diabetes[17]. TEMD Vaccination Study was carried out by using the TEMD database to investigate the prevalence of influenza and pneumococcal vaccinations and to search for the independent associates of vaccination in Turkish patients with T1DM and T2DM.
The TEMD Study is a cross-sectional, nationwide, multicenter survey, which was carried out between April 1 and June 30, 2017, in 68 tertiary endocrine units from 37 cities throughout Turkey. The study centers were selected according to the 12 Nomenclature of Territorial Units for Statistics (NUTS) regions of the country. Both local and central ethics committees approved the study. The ClinicalTrials.gov registration number is NCT03455101. All patients signed informed consent forms before data collection.
Patients with either T1DM or T2DM who were under follow-up in the same center for at least one year were consecutively enrolled in the original study[17]. Patients were excluded if they were pregnant, younger than 18 years, had decompensated liver disease, psychiatric disorders interfering with cognition or compliance, had bariatric surgery, or were undergoing renal replacement therapy.
Patients were asked to fill specifically designed questionnaires about sociodemographic characteristics (age, marital status, education, occupation, and income), concomitant diseases, medications, macro-and microvascular complications, family history, lifestyle, personal diabetes management (diet, exercise, smoking, self-monitoring of blood glucose, and frequency of hypoglycemia), data of outpatient care standards (dietitian visits, diabetes nurse interviews, foot, and dental examinations, and vaccinations), treatment regimens, and current and previous laboratory data. The history of pneumococcal vaccination after diagnosis of diabetes and influenza vaccination in the last year was obtained from the patient's own statement.
The height, weight, and waist circumference recordings were performed according to the standard protocol with the patients in their underwear. The ratio of weight to the square of height (kg/m2) was given as body mass index (BMI). Arterial blood pressure (ABP) was recorded using automatic blood pressure (BP) monitors (Omron M2, HEM-7121-E) in a sitting position after at least 5 min of rest. Three consecutive measurements were conducted on the same arm, and the mean was recorded.
Hypertension was defined as the presence of high office BP recordings or currently undergoing antihypertensive treatment. For patients who were not under antihypertensive medication, an average office BP > 140/90 mmHg in two different visits was defined as hypertension. Dyslipidemia was triglycerides (TG) > 150 or low-density lipoprotein cholesterol (LDL-C) > 100, or low high-density lipoprotein cholesterol (HDL-C; men < 40, women < 50 mg/ dL), or receiving medications for dyslipidemia. The BMI values ≥ 30 kg/m2 were defined as obesity[18]. Treatment targets were defined as glycosylated hemoglobin A1c (HbA1c) < 7% (< 53 mmol/mol), office ABP < 140/90 mmHg, and LDL-C < 100 mg/dL. Regular exercise was defined as performing physical activity on more than two days a week, with each episode lasting for more than 30 min. Low income was self-reported monthly earnings below the minimum wage level declared in 2017. A low education level was defined as receiving less than 8 years of formal education. Macrovascular complications were either self-reported, having a history of coronary artery disease, angina, heart attack, cerebrovascular event, or peripheral artery disease, or recorded by the physicians according to findings such as non-palpable extremity pulses, and low ankle-brachial index (ABI ≤ 0.9), positive findings on coronary or peripheral arteriography, and carotid or peripheral arterial duplex ultrasound examination. Retinopathy was self-reported by the patients when asked whether they have been told in eye examinations that they have any problem related to diabetes mellitus. Nephropathy was defined as the presence of albuminuria or decreased estimated glomerular filtration rate[19]. Neuropathy was defined as the presence of symptoms related to bilateral distal symmetrical neuropathy or other autonomous neuropathies attributed to diabetes mellitus.
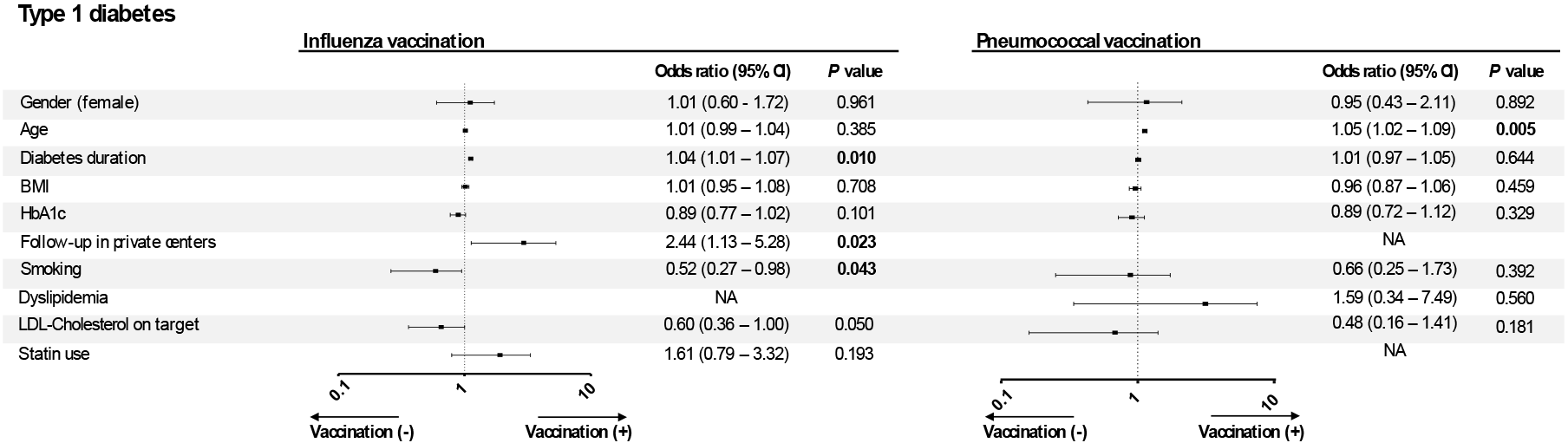
Statistical analysis was performed in SPSS 18.0 (SPSS Inc., Chicago, IL, United States). Normality of distribution was tested using the Shapiro-Wilk test. Data are presented as the mean ± SD for continuous variables or as number (percentage) for categorical variables. An independent sample t-test was used for comparisons among continuous variables, and a Chi-square test was employed for categorical variables. Uni- and multivariate logistic regressions were studied to identify independent variables associated with receiving influenza and pneumococcal vaccination. Having statistical significance (P < 0.05) in the univariate analysis, as well as the clinical rationale for a potential association with vaccination, were the criteria for inclusion in the model for these variables, which were gender, age (years), diabetes duration (years), BMI (kg/m2), HbA1c (%), BP on target (< 140/90 mmHg vs higher), having microvascular and macrovascular complications, education level, smoking, exercise (≤ 2 d/wk vs higher), statin treatment, insulin use, hypertension, dyslipidemia, follow-up center type (private center vs government hospital), and monthly income (in two categories). Odds ratios (ORs) with 95% confidence intervals (CIs) are given in Figures 1 and 2. The P value was two-tailed with a significance level of ≤ 0.05.
Patients with T1DM (n = 454) and T2DM (n = 4721) were included. The clinical and sociodemographic characteristics of patients who have been vaccinated and not vaccinated for influenza and pneumococcus are given in Tables 1 and 2, respectively. The ratio of receiving both vaccines was 6.6% (n = 30) in patients with T1DM and 5.8% (n = 274) in patients with T2DM.
| Patients with T1DM, n = 454 | ||||||
| Influenza vac (+), n = 107 (23.6%) | Influenza vac (-), n = 346 (76.4%) | P value | Pneumo. vac (+), n = 36 (8.0%) | Pneumo. vac (-), n = 415 (92.0%) | P value | |
| Sex (female) | 72 (67.3) | 207 (59.8) | 0.165 | 23 (63.9) | 254 (61.2) | 0.751 |
| Age (yr) | 38.48 ± 13.61 | 32.18 ± 11.58 | < 0.001 | 42.34 ± 14.51 | 32.94 ± 11.89 | < 0.001 |
| Diabetes duration (yr) | 18.20 ± 11.20 | 12.19 ± 9.33 | < 0.001 | 18.17 ± 11.52 | 13.23 ± 9.92 | 0.005 |
| BMI (kg/m2) | 24.67 ± 4.26 | 23.61 ± 4.08 | 0.021 | 24.44 ± 3.70 | 23.83 ± 4.18 | 0.399 |
| SBP office (mm Hg) | 118.44 ± 13.83 | 117.65 ± 15.35 | 0.635 | 119.64 ± 15.30 | 117.68 ± 14.99 | 0.452 |
| DBP office (mm Hg) | 74.44 ± 9.60 | 74.17 ± 9.44 | 0.796 | 75.22 ± 9.43 | 74.15 ± 9.51 | 0.518 |
| HbA1c (%) (mmol/mol) | 8.24 ± 1.77 (66.61 ± 19.33) | 8.79 ± 2.04 (72.56 ± 22.33) | 0.014 | 8.11 ± 2.05 (65.19 ± 22.42) | 8.71 ± 1.99 (71.70 ± 21.72) | 0.095 |
| LDL-C (mg/dL) | 112.75 ± 39.00 | 105.18 ± 35.67 | 0.072 | 117.12 ± 35.19 | 106.04 ± 36.65 | 0.086 |
| TG (mg/dL) | 110.83 ± 74.83 | 116.32 ± 170.15 | 0.754 | 132.29 ± 82.02 | 113.41 ± 158.08 | 0.486 |
| HDL-C (mg/dL) | 60.23 ± 18.70 | 56.32 ± 17.36 | 0.056 | 57.78 ± 19.49 | 57.01 ± 17.49 | 0.805 |
| Macrovascular complications, n (%) | 12 (11.2) | 25 (7.2) | 0.188 | 4 (11.1) | 33 (8.0) | 0.508 |
| Microvascular complications, n (%) | 42 (39.3) | 125 (36.1) | 0.558 | 17 (47.2) | 149 (35.9) | 0.177 |
| Higher education, n (%) | 82 (76.6) | 255 (75.0) | 0.732 | 31 (86.1) | 304 (74.3) | 0.116 |
| Private care center, n (%) | 18 (16.8) | 23 (6.6) | 0.001 | 6 (16.7) | 35 (8.4) | 0.099 |
| Lower-income, n (%) | 18 (21.4) | 69 (25.7) | 0.423 | 4 (14.3) | 83 (25.7) | 0.180 |
| Current smoking, n (%) | 19 (17.8) | 98 (28.5) | 0.027 | 9 (25.0) | 109 (26.3) | 0.862 |
| Regular exercise, n (%) | 30 (28.3) | 67 (19.5) | 0.055 | 9 (25.0) | 88 (21.4) | 0.616 |
| Obesity, n (%) | 13 (12.3) | 26 (7.5) | 0.130 | 4 (11.1) | 35 (8.5) | 0.590 |
| Hypertension, n (%) | 33 (30.8) | 82 (23.8) | 0.147 | 14 (38.9) | 102 (24.7) | 0.062 |
| Dyslipidemia, n (%) | 84 (83.2) | 232 (70.9) | 0.015 | 31 (88.6) | 284 (72.6) | 0.040 |
| Statin treatment, n (%) | 23 (21.5) | 31 (9.0) | < 0.001 | 7 (19.4) | 47 (11.3) | 0.150 |
| Insulin pump, n (%) | 25 (23.8) | 64 (18.6) | 0.236 | 6 (16.7) | 82 (19.9) | 0.827 |
| Achieving metabolic targets, n (%) | ||||||
| HbA1c on target (< 7%), (< 53 mmol/mol) | 16 (15.2) | 52 (15.4) | 0.971 | 7 (20.6) | 61 (15.0) | 0.385 |
| BP on target (< 130/80 mm Hg) | 98 (91.6) | 308 (89.5) | 0.536 | 32 (89.9) | 371 (89.8) | 0.858 |
| LDL-C on target (< 100 mg/dL) | 35 (35.7) | 162 (49.1) | 0.020 | 10 (28.6) | 186 (47.6) | 0.031 |
| Patients with T2DM, n = 4721 | ||||||
| Influenza vac (+), n = 1003 (21.2%) | Influenza vac (-), n = 3718 (78.8%) | P value | Pneumo. vac (+), n = 330 (7.0%) | Pneumo. vac (-), n = 4366 (93.0%) | P value | |
| Sex (female) | 525 (52.3) | 2251 (60.5) | < 0.001 | 180 (54.5) | 2581 (59.1) | < 0.001 |
| Age (yr) | 62.22 ± 9.93 | 57.44 ± 10.36 | < 0.001 | 63.97 ± 9.83 | 58.02 ± 10.38 | < 0.001 |
| Diabetes duration (yr) | 13.62 ± 8.36 | 10.08 ± 7.09 | < 0.001 | 14.10 ± 8.84 | 10.57 ± 7.36 | < 0.001 |
| BMI (kg/m2) | 31.60 ± 6.28 | 32.39 ± 6.65 | 0.004 | 31.08 ± 5.94 | 32.21 ± 6.61 | < 0.001 |
| SBP office (mm Hg) | 133.32 ± 18.15 | 132.34 ± 18.40 | 0.138 | 133.83 ± 17.63 | 132.46 ± 18.40 | 0.191 |
| DBP office (mm Hg) | 79.56 ± 10.84 | 80.81 ± 10.79 | 0.001 | 78.90 ± 10.28 | 80.67 ± 10.86 | 0.004 |
| HbA1c (%) (mmol/mol) | 7.54 ± 1.59 (58.95 ± 17.41) | 7.79 ± 1.78 (61.62 ± 19.49) | < 0.001 | 7.44 ± 1.59 (57.80 ± 17.33) | 7.76 ± 1.76 (61.29 ± 19.20) | 0.001 |
| LDL-C (mg/dL) | 109.27 ± 35.76 | 115.13 ± 36.15 | < 0.001 | 107.80 ± 35.82 | 114.32 ± 36.14 | 0.002 |
| TG (mg/dL) | 169.75 ± 100.06 | 185.77 ± 136.46 | 0.001 | 172.21 ± 111.17 | 183.20 ± 131.21 | 0.144 |
| HDL-C (mg/dL) | 46.81 ± 12.55 | 46.46 ± 13.04 | 0.464 | 47.63 ± 11.91 | 46.43 ± 12.97 | 0.109 |
| Macrovascular complications, n (%) | 317 (31.6) | 827 (22.2) | < 0.001 | 119 (36.1) | 1013 (23.2) | < 0.001 |
| Microvascular complications, n (%) | 509 (50.7) | 1734 (46.6) | 0.021 | 175 (53.0) | 2058 (47.1) | 0.039 |
| Higher education, n (%) | 461 (46.7) | 1331 (36.3) | < 0.001 | 155 (47.7) | 1630 (37.9) | < 0.001 |
| Private care center, n (%) | 154 (15.4) | 319 (8.6) | < 0.001 | 154 (15.4) | 319 (8.6) | < 0.001 |
| Lower income, n (%) | 237 (29.8) | 981 (33.5) | 0.052 | 54 (23.9) | 1157 (33.2) | 0.004 |
| Current smoking, n (%) | 108 (10.8) | 491 (13.3) | 0.039 | 26 (7.9) | 570 (13.1) | 0.006 |
| Regular exercise, n (%) | 226 (22.9) | 688 (18.8) | 0.003 | 87 (26.7) | 824 (19.2) | 0.001 |
| Obesity, n (%) | 548 (55.2) | 2180 (59.4) | 0.016 | 173 (52.9) | 2538 (58.9) | 0.034 |
| Hypertension, n (%) | 768 (77.0) | 2433 (65.9) | < 0.001 | 258 (78.7) | 2924 (67.4) | < 0.001 |
| Dyslipidemia, n (%) | 939 (95.0) | 3457 (95.1) | 0.989 | 310 (94.8) | 4061 (95.1) | 0.835 |
| Statin treatment, n (%) | 531 (52.9) | 1333 (35.9) | < 0.001 | 196 (59.4) | 1659 (38.0) | < 0.001 |
| Achieving targets, n (%) | ||||||
| HbA1c on target (< 7%) (53 mmol/mol) | 434 (44.2) | 1417 (39.1) | 0.004 | 165 (50.8) | 1677 (39.4) | < 0.001 |
| BP on target (< 130/80 mg/dL) | 700 (70.4) | 2563 (69.6) | 0.636 | 249 (75.9) | 2999 (69.4) | 0.013 |
| LDL-C on target (< 100 mg/dL) | 422 (43.6) | 1245 (35.5) | < 0.001 | 141 (43.9) | 1517 (36.7) | 0.010 |
In patients with T1DM, the rate of influenza vaccination was 23.6% (n = 107) and pneumococcus vaccination was 8.0% (n = 36). Compared to patients who were not vaccinated for influenza, patients who were vaccinated were older, had longer diabetes duration, higher BMI levels, higher rates of dyslipidemia and statin use, higher private care center follow-up rates, lower rates of smoking, lower HbA1c levels and LDL-C target achievement rates (P < 0.05 for all). Patients who received pneumococcal vaccination were also older, with longer diabetes duration, higher rates of dyslipidemia, and lower LDL-C target achievement rates (P < 0.05 for all) (Table 1).
In patients with T2DM, the rate of influenza vaccination was 21.2% (n = 1003) and pneumococcus vaccination was 7.0% (n = 330). Patients vaccinated against influenza and/or pneumococcus were predominantly male, older, with longer diabetes duration, lower BMI, diastolic BP, HbA1c, LDL-C, and TG levels (for the influenza group), higher rates of macro and microvascular complications, higher education levels, higher income, a higher rate of private center follow-up, exercising regularly, smoking less, more frequently use statins and higher rate of achieve metabolic targets for HbA1c, BP(for pneumococcus) and LDL-C P < 0.05 for all) (Table 2).
In the multivariable model, longer diabetes duration (OR: 1.04, 95%CI: 1.01-1.07), being followed up in private care center (OR: 2.44, 95%CI: 1.13-5.28) and not smoking (OR: 0.52, 95%CI: 0.27-0.98) were significantly associated with being vaccinated for influenza. Age was the only significant associate of pneumococcus vaccination (OR: 1.05, 95%CI: 1.02-1.09) (Figure 1).
In the multivariable model, female gender (OR: 0.73, 95%CI: 0.60-0.89), age (OR: 1.03, 95%CI: 1.02-1.05), diabetes duration (OR: 1.05, 95%CI: 1.03-1.06), higher education (OR: 1.50, 95%CI: 1.22-1.83), having optimal HbA1c levels (OR: 1.36, 95%CI: 1.13-1.64) and using statins (OR: 1.57, 95%CI: 1.31-1.89) were significantly associated with receiving influenza vaccination.
The significant associates of receiving pneumococcal vaccination were age (OR: 1.05, 95%CI: 1.03-1.07), longer diabetes duration (OR: 1.04, 95%CI: 1.02-1.06), higher education (OR: 1.50, 95%CI: 1.06-2.12), followed up in a private care center (OR: 2.27, 95%CI: 1.47-3.49), having optimal HbA1c levels (OR: 1.69, 95%CI: 1.24-2.30) and statin treatment (OR: 1.65, 95%CI: 1.21-2.25) (Figure 2).
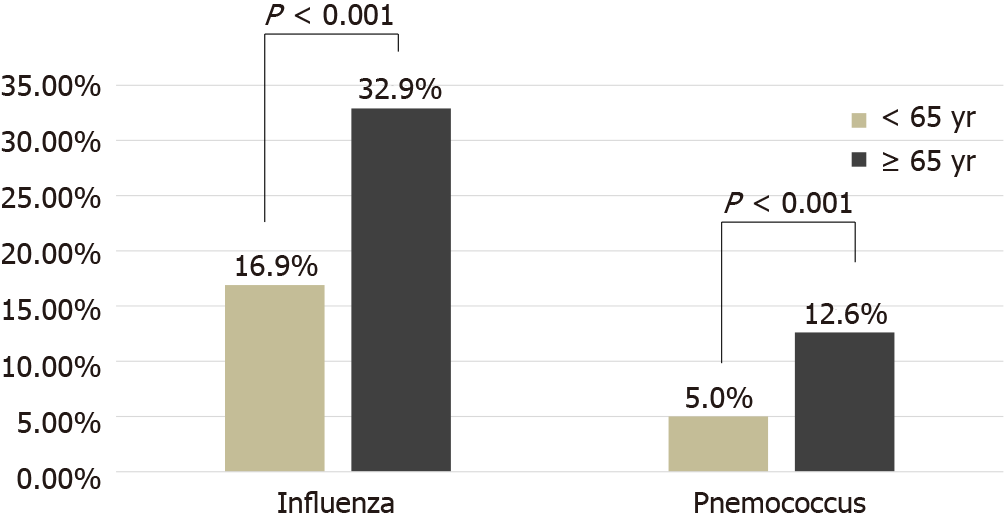
The rates of vaccination were higher in patients with T2DM who were over 65 years old for both influenza (36.4% vs 23.2%, P < 0.001) and pneumococcus (27.3% vs 7.4%, P < 0.001). (Figure 3) We did not compare the vaccination rates in patients with T1DM since there were few patients over 65 years in this group.
The results of the present study showed that Turkish patients with diabetes had very low vaccination rates for influenza and pneumococcus infections. There were no significant differences between the vaccination rates in patients with T1DM and T2DM and the influenza vaccination was much more common in both types. Longer diabetes duration and older age were the common independent associates of having vaccination for both types of patients. On the other hand, higher education levels, having optimal glycemic control, and using statins were the common independent associates of vaccination in patients with T2DM. Regarding the growing awareness of the importance of vaccination, the implications of these findings are discussed below.
Prevention of influenza and pneumococcal infections with routine vaccination decreased mortality and morbidity and the hospitalization rates in patients with diabetes[5,6]. The importance of having vaccinations against influenza and pneumococcus has become more evident during the outbreak of coronavirus disease 2019. Several studies show that influenza and pneumococcal vaccinations may protect against symptomatic cases of infection and death by cross-reactivity with severe acute respiratory syndrome coronavirus 2 antigens[20,21]. On the other hand, the prevention of influenza and pneumococcal infections will help to reduce diagnostic dilemmas, and inappropriate management in terms of antiviral therapy and infection control[22]. National and international guidelines strongly recommend routine vaccinations of influenza and pneumococcal pneumonia in patients with diabetes[7,9]. But the overall vaccination rates are not at the desired levels in many countries. Studies in different populations reported influenza vaccination rates between 40% and 60%[12,23-25]. In terms of pneumococcal vaccine, the situation is slightly worse, and the rate of vaccination in various countries varies between 18% and 53% in patients with diabetes[26-28]. Moreover, there are various reasons for the lower vaccination rates in studies. The most common reason for low vaccination rates in these studies seems to be the low vaccination awareness of both patients and healthcare providers. To produce effective nationwide vaccination policies, it is necessary to know the regional factors that resulted in low vaccination rates.
TEMD Vaccination study showed that the vaccination rates in Turkey are much lower than those of the other countries in patients with T1DM and T2DM. These findings are in line with the results of a previous report about the vaccination rates in Turkish patients with diabetes, which mentioned the rate of receiving influenza and pneumococcus vaccinations in patients with T2DM as 27% and 9.8%, respectively[15]. Another previous single-center study reported the vaccination rates for influenza and pneumococcus as 14.6% and 3.8% in patients with diabetes[16]. Considering that the patients enrolled in the current study were followed up in tertiary endocrine or diabetes units, it is seen that the current vaccination rates are quite low and there is no significant increase in these rates compared to previous studies. In this regard, the low vaccination rates even in this patient group, which includes patients with significantly complicated and advanced diabetic ages, suggest that healthcare givers do not pay sufficient attention to vaccination even in the tertiary care centers for diabetes.
TEMD Vaccination Study also gives us data about the sociodemographical characteristics of patients vaccinated for influenza and pneumococcal infections. Especially the older age and longer diabetes duration were common determinants in patients with both T1DM and T2DM. Patients with a longer duration of diabetes are likely to be more complicated, and therefore, they are likely to visit health centers more frequently and may have a higher chance to get advice for vaccination from healthcare professionals. In this regard, a Spanish study showed that physician visits increase the probability of receiving the vaccination[29]. The multivariable analysis also showed that age had a significant impact on vaccination rates of patients with diabetes. The rates of vaccination for influenza and pneumococcus more than doubled in patients with T2DM over 65 years. The effect of age on vaccination was also reported in many other studies of the diabetes population[10-12]. The reason why age was an important factor for receiving vaccination in many studies may be that patients of older ages are more complicated, have a higher number of comorbidities, and therefore, apply to health centers more frequently. Another reason may be that in many countries, including Turkey, influenza and pneumococcal vaccines are recommended routinely for older ages, regardless of diabetes[30-32].
Being followed up in private centers appear to be another important factor for the higher vaccination rates of patients with diabetes. The reason for this association may be that healthcare providers working in private centers can devote more time to patients and thus may be much more concerned about preventive measures such as recommending vaccination. In this regard, inadequate knowledge provided by the healthcare professionals to patients and/or the clinical inertia of physicians to prevent diseases has been shown as the main obstacles to increasing vaccination rates[33]. In patients with T2DM, optimal glycemic control was also associated with receiving influenza and pneumococcal vaccination. Similarly, higher education level was also a determinant of receiving influenza and pneumococcal vaccination in these patients. In our previous study, high education level was found to be an important predictor for optimal glycemic control[17]. The higher rates of vaccination in educated patients with better glycemic regulation can be explained by the better self-care and higher demand for preventive health measures in these patients. Overall, when the parameters determining vaccination in both types of diabetes are evaluated together, it is seen that especially young patients and patients with shorter diabetes duration are less likely to be vaccinated.
There may be several limitations of the TEMD Vaccination Study. First of all, the cross-sectional design of the study may preclude the casual relationship between patients’ characteristics and receiving influenza and pneumococcal vaccination. Additionally, there may be a possibility of selection bias in the present study. Patients enrolled in this study are under follow-up in the tertiary endocrine or diabetes units, therefore, they are more likely to have multiple comorbidities and complications. For this reason, the study population may not reflect entirely the general population with diabetes. Also, the design of the current study does not include the beliefs and attitudes of physicians about vaccination of patients. However, the large study population, multicenter design, and the presentation of the results for patients with T1DM and T2DM in separate are the strengths of the present study.
In conclusion, the findings of the TEMD Vaccination study indicate that Turkish patients with diabetes have very low influenza and pneumococcal vaccination rates. Considering that this study was conducted in tertiary endocrine or diabetes units, the physicians focused only on the treatment of the disease, and consequently, stay away from preventive medicine. The lower rates of vaccination in some special populations, such as younger patients and patients with short duration of diabetes, suggest that specific vaccination strategies should be developed for these populations. Finally, the TEMD study showed that not only metabolic control but also preventive measures are not sufficient enough for people with diabetes living in Turkey.
In conclusion, this study identified demographic and clinical factors related to low influenza and pneumococcus vaccination rates among the adult population with diabetes. Regarding that this nationwide survey was held in tertiary endocrine or diabetes centers, it is highly likely that the rates of vaccination could be much lower in the overall country. These results should mandate urgent measures to increase vaccination rates including the efforts to improve health awareness in patients and prevent inertia in physicians caring for patients with diabetes.
The prevalence of diabetes is increasing worldwide, and increased diabetes frequency means an increase in the incidence of diabetes-related mortality and morbidity. Turkey stands as the country with the highest diabetes mellitus prevalence in Europe. Since commonly seen infections are associated with significantly increased morbidity and mortality, vaccination programs are now among the standard of care for diabetes mellitus. Vaccination for influenza and pneumococcal infections has gained broad acceptance worldwide.
Although current guidelines emphasize the importance of influenza and pneumococcal vaccination in diabetic patients and that physician acceptance has been reported to increase, the reported vaccination rates still remain low in many countries with different economic development. The rates of vaccination in patients with diabetes mellitus in Turkey have not been systematically evaluated so far.
The main objective of the current study was to perform a nationwide survey to explore the vaccination status for two major diseases, pneumococcus and influenza, among patients with diabetes mellitus. The secondary objective was to determine which patients tend to get vaccinated or not vaccinated.
In a multicenter, cross-sectional survey design, the TEMD Vaccination Study enrolled 454 patients with type 1 diabetes mellitus (T1DM) and 4721 patients with type 2 diabetes mellitus (T2DM), who were under followed up in 68 tertiary endocrinology clinics. Vaccination status was assessed by self-reports and medical records.
The study found 23.6% and 8% vaccination rates for influenza and pneumococcus, respectively, in patients with T1DM. The rates were 21.2% and 8% in patients with T2DM. Vaccination for both conditions was recorded in 6.6% of patients with T1DM and 5.8% of patients with T2DM. Older age and longer diabetes duration were the most common associates of vaccination for both types of diabetes. Among patients with T2DM, higher education level, statin use, and lower HbA1c level were also independently associated with higher vaccination status.
This study showed for the first time that patients with T1DM and T2DM had very low influenza and pneumococcal vaccination rates in Turkey. The findings warrant new and improved strategies to increase the awareness of vaccination among the partners involved in different levels of diabetes care, from patients to policymakers and healthcare professionals.
As vaccination programs are cost-saving by reducing diabetes-related mortality and morbidity, there is an unmet need to identify the barriers and obstacles against the acceptance of vaccination programs by the patients and healthcare programs in this population. Additionally, potential difficulties in implementing the vaccination programs at the system level need to be identified. Finally, increasing the number of patients with diabetes mellitus who are vaccinated should be prioritized as these patients are considered much defenseless against opportunistic infections.
Provenance and peer review: Invited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Azarbakhsh H S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14:29-34. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Bouter KP, Diepersloot RJ, van Romunde LK, Uitslager R, Masurel N, Hoekstra JB, Erkelens DW. Effect of epidemic influenza on ketoacidosis, pneumonia and death in diabetes mellitus: a hospital register survey of 1976-1979 in The Netherlands. Diabetes Res Clin Pract. 1991;12:61-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Koziel H, Koziel MJ. Pulmonary complications of diabetes mellitus. Pneumonia. Infect Dis Clin North Am. 1995;9:65-96. [PubMed] [Cited in This Article: ] |
| 4. | Valdez R, Narayan KM, Geiss LS, Engelgau MM. Impact of diabetes mellitus on mortality associated with pneumonia and influenza among non-Hispanic black and white US adults. Am J Public Health. 1999;89:1715-1721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 100] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Heymann AD, Shapiro Y, Chodick G, Shalev V, Kokia E, Kramer E, Shemer J. Reduced hospitalizations and death associated with influenza vaccination among patients with and without diabetes. Diabetes Care. 2004;27:2581-2584. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Vamos EP, Pape UJ, Curcin V, Harris MJ, Valabhji J, Majeed A, Millett C. Effectiveness of the influenza vaccine in preventing admission to hospital and death in people with type 2 diabetes. CMAJ. 2016;188:E342-E351. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Freedman MS, Hunter P, Ault K, Kroger A. Advisory Committee on Immunization Practices Recommended Immunization Schedule for Adults Aged 19 Years or Older - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:133-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | American Diabetes Association. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44:S40-S52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 80] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 9. | SEMT Diabetes Mellitus Study Group. Clinical Practice Guideline for Diagnosis, Treatment, and Follow-up of Diabetes Mellitus and Its Complications-2019. 12th ed. SEMT Diabetes Mellitus Working Group, 2019. [Cited in This Article: ] |
| 10. | Looijmans-Van den Akker I, Verheij TJ, Buskens E, Nichol KL, Rutten GE, Hak E. Clinical effectiveness of first and repeat influenza vaccination in adult and elderly diabetic patients. Diabetes Care. 2006;29:1771-1776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, Narayan KM. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002. Ann Intern Med. 2006;144:465-474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 394] [Cited by in F6Publishing: 423] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 12. | Jiménez-García R, Jimenez I, Garrido PC, Hernández-Barrera V, de Andres AL, del Barrio JL, de Miguel AG. Coverage and predictors of influenza vaccination among adults with diabetes in Spain. Diabetes Res Clin Pract. 2008;79:510-517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of Influenza Vaccination Intention and Behavior - A Systematic Review of Influenza Vaccine Hesitancy, 2005 - 2016. PLoS One. 2017;12:e0170550. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 717] [Cited by in F6Publishing: 692] [Article Influence: 98.9] [Reference Citation Analysis (0)] |
| 14. | Zimmerman RK, Santibanez TA, Fine MJ, Janosky JE, Nowalk MP, Bardella IJ, Raymund M, Wilson SA. Barriers and facilitators of pneumococcal vaccination among the elderly. Vaccine. 2003;21:1510-1517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Satman I, Akalin S, Cakir B, Altinel S; diaVAX Study Group. The effect of physicians' awareness on influenza and pneumococcal vaccination rates and correlates of vaccination in patients with diabetes in Turkey: an epidemiological Study "diaVAX". Hum Vaccin Immunother. 2013;9:2618-2626. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Arslan IE, Altinova A, Gazi FT. Awareness of hepatitis B, influenza and pneumococcal vaccine among diabetic patients. Gazi Med J. 2016;27. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Sonmez A, Haymana C, Bayram F, Salman S, Dizdar OS, Gurkan E, Kargili Carlıoglu A, Barcin C, Sabuncu T, Satman I; TEMD Study Group. Turkish nationwide survEy of glycemic and other Metabolic parameters of patients with Diabetes mellitus (TEMD study). Diabetes Res Clin Pract. 2018;146:138-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894: i-xii, 1. [PubMed] [Cited in This Article: ] |
| 19. | Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-612. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15626] [Cited by in F6Publishing: 17813] [Article Influence: 1187.5] [Reference Citation Analysis (0)] |
| 20. | Green I, Ashkenazi S, Merzon E, Vinker S, Golan-Cohen A. The association of previous influenza vaccination and coronavirus disease-2019. Hum Vaccin Immunother. 2021;17:2169-2175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Root-Bernstein R. Possible Cross-Reactivity between SARS-CoV-2 Proteins, CRM197 and Proteins in Pneumococcal Vaccines May Protect Against Symptomatic SARS-CoV-2 Disease and Death. Vaccines (Basel). 2020;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Maltezou HC, Theodoridou K, Poland G. Influenza immunization and COVID-19. Vaccine. 2020;38:6078-6079. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 23. | Athamneh LN, Sansgiry SS. Influenza vaccination in patients with diabetes: disparities in prevalence between African Americans and Whites. Pharm Pract (Granada). 2014;12:410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Yang L, Nan H, Liang J, Chan YH, Chan L, Sum RW, Kwan YM, Zhou F, Meng H, Suen LK. Influenza vaccination in older people with diabetes and their household contacts. Vaccine. 2017;35:889-896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Thewjitcharoen Y, Butadej S, Malidaeng A, Yenseung N, Nakasatien S, Lekpittaya N, Kittipoom W, Krittiyawong S, Himathongkam T. Trends in influenza and pneumococcal vaccine coverage in Thai patients with type 2 diabetes mellitus 2010-2018: Experience from a tertiary diabetes center in Bangkok. J Clin Transl Endocrinol. 2020;20:100227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Yang TU, Song JY, Noh JY, Cheong HJ, Kim WJ. Influenza and Pneumococcal Vaccine Coverage Rates among Patients Admitted to a Teaching Hospital in South Korea. Infect Chemother. 2015;47:41-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Sotiropoulos A, Merkouris P, Gikas A, Skourtis S, Skliros E, Lanaras L, Nikolaou T, Pappas S. Influenza and pneumococcal vaccination rates among Greek diabetic patients in primary care. Diabet Med. 2005;22:110-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Gilani F, Majumdar SR, Johnson JA, Simpson SH; ABCD Cohort Investigators. Factors associated with pneumococcal vaccination in 2040 people with type 2 diabetes: A cross-sectional study. Diabetes Metab. 2020;46:137-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Jimenez-Trujillo I, López-de Andrés A, Hernández-Barrera V, Carrasco-Garrido P, Santos-Sancho JM, Jiménez-García R. Influenza vaccination coverage rates among diabetes sufferers, predictors of adherence and time trends from 2003 to 2010 in Spain. Hum Vaccin Immunother. 2013;9:1326-1332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Türkiye Enfeksiyon Hastalıkları ve Klinik Mikrobiyoloji Uzmanlık Derneği (EKMUD). Erişkin Bağışıklama Rehberi - 2019. [cited 26 Apr 2021]. In: Türkiye Enfeksiyon Hastalıkları ve Klinik Mikrobiyoloji Uzmanlık Derneği (EKMUD) [Internet]. Available from: https://www.ekmud.org.tr/emek/rehber/indir/97. [Cited in This Article: ] |
| 31. | TC. Sağlık Bakanlığı, Halk Sağılığı Genel Müdürlüğü, Yetişkin Aşılama Rehberi. 30 yetişkin aşılama. [cited 26 Apr 2021]. In: Asi.saglik [Internet]. Available from: https://asi.saglik.gov.tr/asi-kimlere-yapilir/Liste/30-yetişkin-aşılama.html. [Cited in This Article: ] |
| 32. | Centers for Disease Control and Prevention. Recommended Adult Immunization Schedule for Ages 19 Years or Older. [cited 26 Apr 2021]. In: Centers for Disease Control and Prevention [Internet]. Available from: https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html#vacc-adult. [Cited in This Article: ] |
| 33. | Takayama M, Wetmore CM, Mokdad AH. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev Med. 2012;54:358-362. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |