Published online Apr 16, 2015. doi: 10.4253/wjge.v7.i4.429
Peer-review started: May 3, 2014
First decision: May 23, 2014
Revised: January 1, 2015
Accepted: January 15, 2015
Article in press: January 19, 2015
Published online: April 16, 2015
A 45-year-old man of Middle Eastern origin, morbid obese, with a body mass index of 39 had an intra-gastric balloon, filled with 500 mL of saline/methylene blue and intended as definite therapy, inserted some 8 wk previously. He was admitted to the emergency department with abdominal cramps. An ultrasound of the abdomen was performed in ER which confirmed the balloon to be in place without any abnormality. He was discharged home on symptomatic medication. Patient remains symptomatic therefore he reported back to ER 2 d later. Computed tomography scan was performed this time for further evaluation which revealed a metallic ring present in the small bowel while the intra-gastric balloon was in its proper position. There was no clinical or radiological sign of intestinal obstruction. Patient was hospitalized for observation and conservative management. The following night, patient experienced sudden and severe abdominal pain, therefore an X-ray of the abdomen in erect position was done, which showed free air under the right dome of diaphragm. Patient was transferred to O.R for emergency laparotomy. There were two small perforations identified at the site of the metallic ring entrapment. The ring was removed and the perforations were repaired. Due to increasing prevalence of obesity and advances in modalities for its management, physicians should be aware of treatment options, their benefits, complications and clinical presentation of the known complications. Physicians need to be updated to approach these complications within time, to avoid life-threatening situations caused by these appliances.
Core tip: Because the rare reported unexpected complications that the balloon safety ring which designed to prevent its complication it was by it self the cause of serious complication. The u/s confirmation of balloon position was miss leading so radiographic images was essential when there is suspicious.
- Citation: Al-Zubaidi AM, Alghamdi HU, Alzobydi AH, Dhiloon IA, Qureshi LA. Bowel perforation due to break and distal passage of the safety ring of an adjustable intra-gastric balloon: A potentially life threatening situation. World J Gastrointest Endosc 2015; 7(4): 429-432
- URL: https://www.wjgnet.com/1948-5190/full/v7/i4/429.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i4.429
Obesity is a major health problem, and is challenging the modern world. Its distribution is insidious throughout the world. Because it is a major risk factor for many potential life-threatening conditions, different invasive and non-invasive therapeutic techniques are being used to help the individuals suffering from obesity return to a healthy life.
Among these modalities, intra-gastric balloons are gaining popularity because of their efficacy, safety, and technical ease, as shown by some studies[1,2]. Moreover, it has been recommended as a weight reduction adjuvant before bariatric surgery, and before all kinds of planned surgery in morbidly obese persons; to reduce life-threatening co-morbidities and reduction of surgical risk[3,4].
Most of the reported serious complications with the newer generation of balloons take place 6 mo after placement of the balloon[5]. Here, we are reporting a case of small bowel perforation, secondary to break down and migration of the safety ring of an adjustable intra-gastric balloon (Spatz) that happened 8 wk after its insertion.
A 45-year-old man was brought to the emergency department with a history of abdominal cramps, on and off, for a few days, associated with anorexia and nausea. Patient had a history of saline filled adjustable intra-gastric balloon placement for the management of obesity 8 wk ago. Initial investigations including an ultrasound abdomen were unremarkable for any complication or pathology. Symptomatic treatment trial was unsuccessful and patient remained symptomatic, therefore, he reported back to ER.
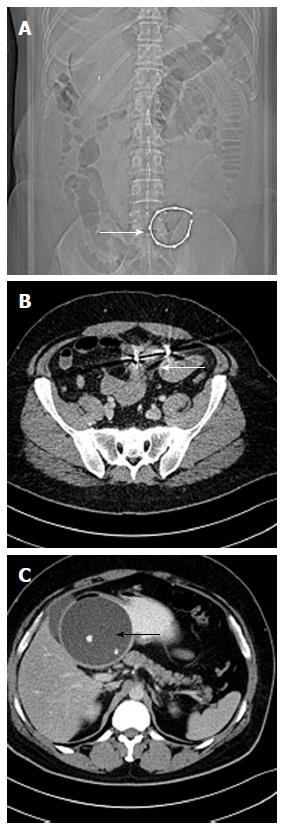
He was in mild distress this time, but stable hemodynamically. Although his abdomen was soft and bowel sounds were active, a new onset mild generalized abdominal tenderness was noticed on clinical examination, therefore an abdominal computed tomography (CT) scan was planned which later reported the presence of a metallic ring (foreign body) in the small bowel without any sign of perforation or obstruction, while the adjustable balloon was in place (Figure 1).
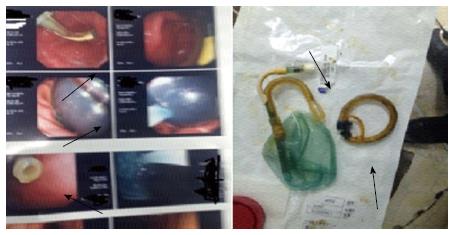
Patient was admitted for observation, advised null per oral, and started on intra-venous fluid. He becomes completely asymptomatic on conservative management. Next morning, patient underwent an upper gastrointestinal endoscopy. Balloon was seen in place but the safety ring was not seen in position, nor was it present in gastric cavity. Therefore, balloon was retrieved. Patient was stable clinically till night when he experienced a sudden and severe abdominal pain.
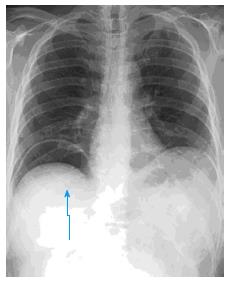
Plain X-ray film of abdomen was taken that revealed the presence of free air under the right dome of the diaphragm. Surgical team was informed immediately. Mean while NG tube was placed and IV antibiotics were initiated. Patient was transferred to the operation room for an emergency laparotomy. A 10 cm mid-line incision was given small bowel was examined. Two perforations were identified in distal jejunum at the site of ring entrapment. Small incision was made at the site of perforation and metallic ring was extracted followed by a successful primary repair of small bowel. Figure 2 shows free air under the diaphragm. Figure 3 shows endoscopic and gross eye views of both balloon and its broken ring after extraction.
Intra-gastric balloons were introduced in the early 1980s for the management of morbid obesity. These IGBs have attracted physicians since their first use[6].
Initial results were promising for this less invasive procedure in comparison with surgery for the treatment of morbid obesity[7-9]. Some published results reveal an average weight loss of 11-15 kg within 6 mo[10-13]. Standard IGBs are having significant undesired effects, e.g., nausea or vomiting, and significant abdominal discomfort in initial phase. Balloon deflation and distal migration that may lead to bowel obstruction and a physical adaptation indicated by lack of further weight loss effects by these IGBs[14-17]. Complications of balloon insertion constitutes a diagnostic challenge because majority of patients were presented with non-specific abdominal pain, nausea or vomiting[18-23].
Spatz adjustable balloon system (SPATZ-ABS) is a vibrant bariatric therapy with significantly improved implantation time, having an adjustable size balloon according to desired weight, and a safety ring that prevents distal migration of device in case of rupture of balloon[24].
In our case, the safety ring was detached from the rest of the system and migrated down to the jejunum while the balloon remains in the stomach. It was retrieved endoscopically. The jejunal perforation caused by migration of the safety ring was managed by emergency surgery. This complication was unexpected as there was no clinical sign of intestinal obstruction. Ultrasonography alone was also not helpful in identifying this complication by SPATZ-ABS.
Because of non-specific clinical presentation and inadequacy of ultrasonography alone, we suggest that whenever there is suspicion of a balloon related complication, a combination of plain abdominal X-ray, ultrasound, an upper GI endoscopy and/or CT scan will be an appropriate approach for early detection and management of complication.
A 45-year-old patient with history of intragastric Bio enteric balloon, experienced a recurrent cramp and abdominal pain, which became severe when perforation occurs.
No significant clinical signs, but when perforation occurs there was abdominal tenderness.
Potential perforated duodenal ulcer, acute pancreatitis, acute intestinal obstruction or biliary colic.
The CBC, LFT, KFT, and coagulation profile were all within normal parameters.
U/S abdominal was normal, computed tomography abdominal the ring was migrated down to the small bowel, when perforation occurred X-ray of the abdominal area showed free air under right dome of the diaphragm.
A pathology sample was not tested, but during surgery two small perforations were closed by sutures.
NPO, endoscopic removal of the balloon, Laparotomy for repair of perforation, Pethedin inj, Paracetamol inj, Cefotoxim inj, Metronidazol infusion and iv fluid.
From this case, any abdominal pain in a patient with an intragastric balloon should be taken seriously, and potential complications managed early.
This case report should be published.
P- Reviewer: Silecchia G S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Genco A, Bruni T, Doldi SB, Forestieri P, Marino M, Busetto L, Giardiello C, Angrisani L, Pecchioli L, Stornelli P. BioEnterics Intragastric Balloon: The Italian Experience with 2,515 Patients. Obes Surg. 2005;15:1161-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 273] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 2. | Evans JD, Scott MH. Intragastric balloon in the treatment of patients with morbid obesity. Br J Surg. 2001;88:1245-1248. [PubMed] [Cited in This Article: ] |
| 3. | De Waele B, Reynaert H, Urbain D, Willems G. Intragastric balloons for preoperative weight reduction. Obes Surg. 2000;10:58-60. [PubMed] [Cited in This Article: ] |
| 4. | Loffredo A, Cappuccio M, De Luca M, de Werra C, Galloro G, Naddeo M, Forestieri P. Three years experience with the new intragastric balloon, and a preoperative test for success with restrictive surgery. Obes Surg. 2001;11:330-333. [PubMed] [Cited in This Article: ] |
| 5. | Vanden Eynden F, Urbain P. Small intestine gastric balloon impaction treated by laparoscopic surgery. Obes Surg. 2001;11:646-648. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Nieben OG, Harboe H. Intragastric balloon as an artificial bezoar for treatment of obesity. Lancet. 1982;1:198-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 187] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | McFarland RJ, Grundy A, Gazet JC, Pilkington TR. The intragastric balloon: a novel idea proved ineffective. Br J Surg. 1987;74:137-139. [PubMed] [Cited in This Article: ] |
| 8. | Ramhamadany EM, Fowler J, Baird IM. Effect of the gastric balloon versus sham procedure on weight loss in obese subjects. Gut. 1989;30:1054-1057. [PubMed] [Cited in This Article: ] |
| 9. | Benjamin SB, Maher KA, Cattau EL, Collen MJ, Fleischer DE, Lewis JH, Ciarleglio CA, Earll JM, Schaffer S, Mirkin K. Double-blind controlled trial of the Garren-Edwards gastric bubble: an adjunctive treatment for exogenous obesity. Gastroenterology. 1988;95:581-588. [PubMed] [Cited in This Article: ] |
| 10. | Roman S, Napoléon B, Mion F, Bory RM, Guyot P, D’Orazio H, Benchetrit S. Intragastric balloon for “non-morbid” obesity: a retrospective evaluation of tolerance and efficacy. Obes Surg. 2004;14:539-544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Mion F, Napoléon B, Roman S, Malvoisin E, Trepo F, Pujol B, Lefort C, Bory RM. Effects of intragastric balloon on gastric emptying and plasma ghrelin levels in non-morbid obese patients. Obes Surg. 2005;15:510-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Melissas J, Mouzas J, Filis D, Daskalakis M, Matrella E, Papadakis JA, Sevrisarianos N, Charalambides D. The intragastric balloon - smoothing the path to bariatric surgery. Obes Surg. 2006;16:897-902. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Hogan RB, Johnston JH, Long BW, Sones JQ, Hinton LA, Bunge J, Corrigan SA. A double-blind, randomized, sham-controlled trial of the gastric bubble for obesity. Gastrointest Endosc. 1989;35:381-385. [PubMed] [Cited in This Article: ] |
| 14. | Busetto L, Segato G, De Luca M, Bortolozzi E, MacCari T, Magon A, Inelmen EM, Favretti F, Enzi G. Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: a case-control study. Obes Surg. 2004;14:671-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Imaz I, Martínez-Cervell C, García-Alvarez EE, Sendra-Gutiérrez JM, González-Enríquez J. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841-846. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 281] [Cited by in F6Publishing: 221] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 16. | Lecumberri E, Krekshi W, Matía P, Hermida C, de la Torre NG, Cabrerizo L, Rubio MÁ. Effectiveness and safety of air-filled balloon Heliosphere BAG® in 82 consecutive obese patients. Obes Surg. 2011;21:1508-1512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Vilallonga R, Valverde S, Caubet E. Intestinal occlusion as unusual complication of new intragastric balloon Spatz Adjustable Balloon system for treatment of morbid obesity. Surg Obes Relat Dis. 2013;9:e16-e17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Doldi SB, Micheletto G, Perrini MN, Librenti MC, Rella S. Treatment of morbid obesity with intragastric balloon in association with diet. Obes Surg. 2002;12:583-587. [PubMed] [Cited in This Article: ] |
| 19. | Pretolesi F, Redaelli G, Papagni L, Derchi LE. Intragastric balloon for morbid obesity causing chronic gastric dilatation. Eur Radiol. 2001;11:588-589. [PubMed] [Cited in This Article: ] |
| 20. | Forlano R, Ippolito AM, Iacobellis A, Merla A, Valvano MR, Niro G, Annese V, Andriulli A. Effect of the BioEnterics intragastric balloon on weight, insulin resistance, and liver steatosis in obese patients. Gastrointest Endosc. 2010;71:927-933. [PubMed] [Cited in This Article: ] |
| 21. | Mohammed AE, Benmousa A. Acute pancreatitis complicating intragastric balloon insertion. Case Rep Gastroenterol. 2008;2:291-295. [PubMed] [Cited in This Article: ] |
| 22. | Benchimol AK, Cardoso IS, Fandiño J, Bittar T, Freitas S, Coutinho WF. [Non-alcoholic steatohepatitis induced by fast weight loss during the use of intragastric balloon--a case report]. Arq Bras Endocrinol Metabol. 2007;51:631-634. [PubMed] [Cited in This Article: ] |
| 23. | Nikolic M, Mirosevic G, Ljubicic N, Boban M, Supanc V, Nikolic BP, Zjacic-Rotkvic V, Bekavac-Beslin M, Gacina P. Obesity treatment using a Bioenterics intragastric balloon (BIB)--preliminary Croatian results. Obes Surg. 2011;21:1305-1310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | de la Riva S, Muñoz-Navas M, Rodriguez-Lago I, Silva C. Small-bowel migration: a possible complication of adjustable intragastric balloons. Endoscopy. 2012;44 Suppl 2 UCTN:E224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |