Published online Dec 16, 2023. doi: 10.4253/wjge.v15.i12.699
Peer-review started: November 10, 2023
First decision: November 21, 2023
Revised: November 25, 2023
Accepted: December 6, 2023
Article in press: December 6, 2023
Published online: December 16, 2023
Preoperative diagnosis of appendiceal mucinous neoplasms is challenging, and there are few reports regarding the endosonographic characteristics of these neoplasms.
To provide a retrospective assessment of the imaging features of appendiceal mucinous neoplasms using endoscopic ultrasound (EUS) by curved linear-array echoendoscope.
A database of all patients with appendiceal mucinous neoplasms who had received EUS examination at our hospital between January 2018 and July 2023 was retrospectively analyzed. The EUS characteristics and patients’ clinical data were reviewed.
Twenty-two patients were included in the study. The linear-array echoendoscope successfully reached the ileocecal region in every patient. In the endoscopic view, we could observe the protrusion in the appendiceal orifice in all patients. A volcano sign was observed in two patients, and an atypical volcano sign was seen in two patients. EUS showed that all 22 lesions were submucosal cystic hypoechoic lesions with clear boundaries. No wall nodules were observed, but an onion-peeling sign was observed in 17 cases.
Linear-array echoendoscope is safe to reach the ileocecal region under the guidance of EUS. Image features on endoscopic and echoendosonograhic views could be used to diagnose appendiceal mucinous neoplasms.
Core Tip: Appendiceal mucocele is a relatively rare disease. The preoperatively accurate diagnosis is crucial to the treatment strategy. Endoscopy has played an important role in the diagnosis of appendiceal mucocele. Image features on endoscopic and echoendosonograhic views could be used to diagnose appendiceal mucinous neoplasms.
- Citation: Zhang JC, Ma YY, Lan YZ, Li SB, Wang X, Hu JL. Evaluation of appendiceal mucinous neoplasms by curved linear-array echoendoscope: A preliminary study. World J Gastrointest Endosc 2023; 15(12): 699-704
- URL: https://www.wjgnet.com/1948-5190/full/v15/i12/699.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i12.699
Appendiceal mucocele is a relatively rare disease. Based on the pathological type, appendiceal mucocele can be classified as mucosal hyperplasia, mucinous cystadenoma, or mucinous cystadenocarcinoma. Even though appendiceal mucocele, expect mucinous cystadenocarcinoma, does not typically show definitive malignant features, it can rupture and lead to the development of pseudomyxoma peritonei, a life-threatening complication with a 10-year survival rate of 45%[1]. Therefore, an accurate diagnosis is crucial to the treatment strategy. However, patients with appendiceal mucocele do not have specific clinical manifestations, delaying diagnosis[2,3]. The patient may have no symptoms or show acute appendicitis-like presentation in the early stages of the disease with right lower quadrant pain secondary to distention of the appendix by mucin[4]. Since the development of endoscopic ultrasound (EUS)[5], endoscopy has played an important role in the diagnosis of appendiceal mucocele. To date, only a few studies have demonstrated the EUS characteristics of appendiceal mucocele using miniprobe catheter EUS. Moreover, miniprobe EUS exhibited limited depth of penetration. In this work, we evaluated the EUS characteristics of appendiceal mucocele by curved linear-array echoendoscope to assess the accurate diagnosis.
Patients with a pathological diagnosis of appendiceal mucocele who had received EUS examination by linear echoendoscope from January 2018 to July 2023 were reviewed. The patients’ general characteristics, EUS results, and surgery method were recorded. This study was approved by the institutional review board of Hebei Cangzhou Hospital of Integrated Traditional Chinese Medicine and Western Medicine.
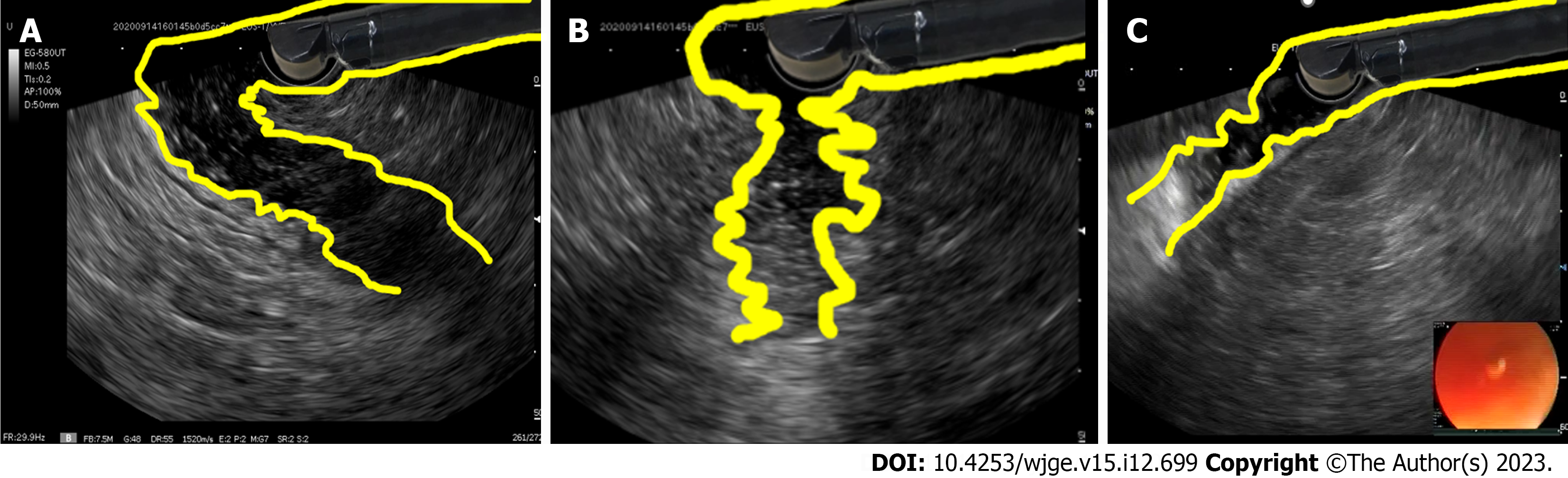
All cases were performed after a standard bowel preparation, using either a linear echoendoscope (3870UTK, Pentax company, Japan) or linear echoendoscope (EG-580UT, Fujifilm company, Japan). We inserted the linear echoendoscope with the guidance of endoscopic and ultrasound views. During the insertion of the endoscope, if the angle of the colon was too large to display the endoscopic view, we used ultrasound to scan the direction of the proximal colon to assist in inserting the endoscope (Figure 1). Closed intestinal cavities are often difficult to distinguish on ultrasound images. The direction of the intestinal cavity can be easier to identify by injecting water into the cavity.
This study included 22 patients that were diagnosed with appendiceal mucocele and received EUS examination. Among them, there were 9 male and 13 female patients, aged 26-80 years. The average age was 60.9 ± 12.6 years. Clinical symptoms included discomfort in the right lower abdomen in 6 cases, appendicitis in 10 cases, and physical examination in 6 cases.
The echoendoscope successfully reached the ileocecal region in all 22 patients. In the endoscopic view, we could observe the protrusion in the appendiceal orifice. The surface of the protrusion was smooth, and no secretion was observed in 20 cases, of which the appendiceal orifice was compressed to one side of the lesion in 18 cases and the appendiceal orifice was located on the surface of the lesion in 2 cases (volcano sign). The appendiceal orifice was located on the surface of the lesion with white secretion in 2 cases (atypical volcano sign) (Figure 2). EUS showed that all 22 lesions were submucosal cystic hypoechoic lesions with clear boundaries and no wall nodules were observed. The size of the lesions ranged from 1.1 cm to 5.7 cm, with the average size being 3.1 ± 1.1 cm. Onion-peeling sign, which was defined as intermittent hyperechoic lines in the hypoechoic lesion, could be observed in 17 cases (Figure 3). Overall, 16 cases underwent appendectomy, 4 cases received ileocecal resection, and 2 cases underwent right hemicolectomy. The surgical process was smooth and there were no complications. Postoperative pathology confirmed 20 cases of appendiceal mucinous adenoma and 2 cases of mucinous adenocarcinoma.
Appendiceal mucocele, caused by dilation of the lumen because of an accumulation of mucus, is a relatively uncommon disease. Appendiceal mucinous cystadenoma can secrete mucin and present in a malignant fashion, resulting in the development of life-threatening pseudomyxoma peritonei. However, it is difficult to make the diagnosis of appendiceal mucocele. The presentation of appendiceal mucocele is quite variable, and the clinical symptoms are vague and non-specific. For asymptomatic patients, appendiceal mucocele may be incidentally detected on imaging examination or during a colonoscopy. For symptomatic patients, appendiceal mucocele has an overlap of symptoms with acute appendicitis, frequently leading to a preoperative misdiagnosis. Therefore, sufficient preoperative examinations are necessary to make an accurate diagnosis. For multiphase computed tomography images, appendiceal mucocele should be considered when a focal well-defined cystic mass with slightly higher water attenuation, thickened cystic wall with ring mural enhancement, and a characteristic progressive contrast enhancement in imaging, especially in older females with non-specific symptoms that are similar to appendicitis[6].
During colonoscopy, the classical appearance of appendiceal mucocele is a ‘‘volcano sign’’, with the appendiceal orifice seen at the center of the mound[7,8]. Colonoscopic biopsy is not recommended because the overlying mucosa is not involved, and biopsy carries the potential risk of rupturing the appendiceal mucocele. The author described an atypical “volcano sign” with mucus spewing out of the appendicular orifice and the final diagnosis was appendiceal mucinous adenocarcinoma[9]. Our study also found two mucinous adenocarcinomas that presented as an atypical “volcano sign”, which may be caused when the tumor ruptured into the lumen of the colon, releasing mucus. Overall, an atypical “volcano sign” might be the sign of mucinous adenocarcinoma.
EUS can be useful in confirming the nature of the lesion, thereby ruling out solid lesions such as carcinoid, lipoma, or gastrointestinal stromal tumor[10,11]. Due to the maneuverability of the linear array echoendoscope, it was widely used to evaluate lesions in left colon and rectum[12,13]. Using a linear array echoendoscope to evaluate the proximal colon has been reported in only a few studies. For more proximal areas of the colon, forward-viewing echocolonoscopes and through-the-scope miniprobe catheter ultrasound were typically used, but these methods have limitations. In this study, we used a linear array echoendoscope to evaluate the appendiceal lesions. Advancement of a conventional curved linear echoendoscope beyond the sigmoid colon usually requires previous placement of an overtube or a guidewire[14]. In this study, we inserted the linear echoendoscope just with the guidance of endoscopic and ultrasound views. If the intestinal lumen could not be seen under endoscopic view, we injected water into the intestinal lumen to help identify the direction of the intestinal lumen using ultrasound view. We passed through the sigmoid and descending colon without loop and maintained a good freedom of scope. If the scope is difficult to pass, we could use a guidewire method. Appendiceal mucocele is a hypoechoic lesion with clear boundaries and is without mural nodes. In addition, we found that the “onion-peeling sign” could be seen in most cases, which may be due to the different timing of mucus secretion. The “onion-peeling sign” could help us to make a differential diagnosis. For unclear lesions, EUS-fine-needle aspiration (FNA) could be performed to confirm the diagnosis[15-17]. However, if appendiceal mucocele is suspected, EUS-FNA is forbidden to avoid the formation of pseudomyxoma peritonei.
Surgery is a standard method for the treatment of appendiceal mucocele. A simple appendectomy could be performed for mucosal hyperplasia and mucinous cystadenoma. In addition, a right hemicolectomy with lymph node dissection is indicated for cystadenocarcinoma. After surgery, patients should be offered follow-up to exclude the subsequent development of pseudomyxoma peritonei[18]. The risk of pseudomyxoma peritonei is related to the pathological finding and is higher if acellular mucin is found beyond the appendiceal serosa[19].
There are limitations in our study. The study was a retrospective study and only a small cohort of patients were included. All the procedures were performed by experienced doctor. For difficult colonoscopy, the safety of intubation of linear echoendoscope into cecum should be further studied.
Endoscopy plays an important role in the diagnosis of appendiceal mucocele. We can safely evaluate the lesion in the ileocecal region by using a linear-array echoendoscope. A volcano sign on endoscopic view and EUS features could be used to diagnose appendiceal mucinous neoplasms.
Appendiceal mucinous neoplasms can present in a malignant fashion, but preoperative diagnosis of appendiceal mucinous neoplasms is difficult. Endoscopy plays an important role in the diagnosis of appendiceal mucinous neoplasms. There are limited reports regarding the endosonographic characteristics of these neoplasms.
We evaluated the imaging features of appendiceal mucinous neoplasms using endoscopic ultrasound (EUS) by curved linear-array echoendoscope.
To describe image features on endoscopic and echoendosonograhic views of appendiceal mucinous neoplasms.
The EUS characteristics and patients’ clinical data were reviewed.
The appendiceal orifice located on the surface of the lesion in 2 cases (volcano sign) and the appendiceal orifice located on the surface of the lesion with white secretion in 2 cases (atypical volcano sign) were seen. EUS showed that the lesions were submucosal cystic hypoechoic lesions with clear boundaries and no wall nodules were observed. Onion-peeling sign, which was defined as intermittent hyperechoic lines in the hypoechoic lesion, could be observed in part of cases.
This study demonstrated that we can safely evaluate the lesion in the ileocecal region by using a linear-array echoendoscope. A volcano sign on endoscopic view and EUS features could be used to diagnose appendiceal mucinous neoplasms.
In the future, for difficult colonoscopy, the safety of intubation of linear echoendoscope into cecum should be studied.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garcia-Ibanez P, Spain S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Nishikawa G, Sekine S, Ogawa R, Matsubara A, Mori T, Taniguchi H, Kushima R, Hiraoka N, Tsuta K, Tsuda H, Kanai Y. Frequent GNAS mutations in low-grade appendiceal mucinous neoplasms. Br J Cancer. 2013;108:951-958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol. 2006;7:69-76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 459] [Cited by in F6Publishing: 478] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 3. | Ito H, Osteen RT, Bleday R, Zinner MJ, Ashley SW, Whang EE. Appendiceal adenocarcinoma: long-term outcomes after surgical therapy. Dis Colon Rectum. 2004;47:474-480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Bradley RF, Stewart JH 4th, Russell GB, Levine EA, Geisinger KR. Pseudomyxoma peritonei of appendiceal origin: a clinicopathologic analysis of 101 patients uniformly treated at a single institution, with literature review. Am J Surg Pathol. 2006;30:551-559. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 250] [Cited by in F6Publishing: 270] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 5. | Tabacelia D, Martiniuc A, Burtea DE, Saftoiu A, Stroescu C. Hot topics in therapeutic EUS. Endosc Ultrasound. 2022;11:153-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 6. | Yu XR, Mao J, Tang W, Meng XY, Tian Y, Du ZL. Low-grade appendiceal mucinous neoplasms confined to the appendix: clinical manifestations and CT findings. J Investig Med. 2020;68:75-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Shiihara M, Ohki T, Yamamoto M. Preoperative Diagnosis and Surgical Approach of Appendiceal Mucinous Cystadenoma: Usefulness of Volcano Sign. Case Rep Gastroenterol. 2017;11:539-544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Zanati SA, Martin JA, Baker JP, Streutker CJ, Marcon NE. Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc. 2005;62:452-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Vashistha N, Deo A, Singhal D. Gastrointestinal: Mucocele appendix with atypical "volcano sign". J Gastroenterol Hepatol. 2022;37:45. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (1)] |
| 10. | Uradomo LT, Darwin PE. Evaluation of subepithelial abnormalities of the appendix by endoscopic ultrasound. Diagn Ther Endosc. 2009;2009:295379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Cortellini F, Carrara S, Fusaroli P. EUS-guided fine-needle biopsy for gastric submucosal tumors: Does one size fit all? Endosc Ultrasound. 2022;11:151-152. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 12. | Bhutani MS, Nadella P. Utility of an upper echoendoscope for endoscopic ultrasonography of malignant and benign conditions of the sigmoid/left colon and the rectum. Am J Gastroenterol. 2001;96:3318-3322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Kongkam P, Linlawan S, Aniwan S, Lakananurak N, Khemnark S, Sahakitrungruang C, Pattanaarun J, Khomvilai S, Wisedopas N, Ridtitid W, Bhutani MS, Kullavanijaya P, Rerknimitr R. Forward-viewing radial-array echoendoscope for staging of colon cancer beyond the rectum. World J Gastroenterol. 2014;20:2681-2687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Sasaki Y, Niwa Y, Hirooka Y, Ohmiya N, Itoh A, Ando N, Miyahara R, Furuta S, Goto H. The use of endoscopic ultrasound-guided fine-needle aspiration for investigation of submucosal and extrinsic masses of the colon and rectum. Endoscopy. 2005;37:154-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Ragab K, Elmeligui AM, Atalla H, Okasha HH. An unexpected complication during EUS-FNA. Endosc Ultrasound. 2022;11:145-146. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 16. | Facciorusso A, Gkolfakis P, Tziatzios G, Ramai D, Papanikolaou IS, Triantafyllou K, Lisotti A, Fusaroli P, Mangiavillano B, Chandan S, Mohan BP, Crinò SF. Comparison between EUS-guided fine-needle biopsy with or without rapid on-site evaluation for tissue sampling of solid pancreatic lesions: A systematic review and meta-analysis. Endosc Ultrasound. 2022;11:458-465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 15] [Reference Citation Analysis (0)] |
| 17. | Feng L, Guo J, Wang S, Liu X, Ge N, Wang G, Sun S. Endoscopic Transmural Drainage and Necrosectomy in Acute Necrotizing Pancreatitis: A Review. J Transl Int Med. 2021;9:168-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Honoré C, Caruso F, Dartigues P, Benhaim L, Chirica M, Goéré D, Elias D. Strategies for Preventing Pseudomyxoma Peritonei After Resection of a Mucinous Neoplasm of the Appendix. Anticancer Res. 2015;35:4943-4947. [PubMed] [Cited in This Article: ] |
| 19. | Yantiss RK, Shia J, Klimstra DS, Hahn HP, Odze RD, Misdraji J. Prognostic significance of localized extra-appendiceal mucin deposition in appendiceal mucinous neoplasms. Am J Surg Pathol. 2009;33:248-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |